Category: Tips For Nurses
Articles for nurses caring for terminally ill patients including how to manage challenging situations.
Articles for nurses caring for terminally ill patients including how to manage challenging situations.

Discover how acuity impacts hospice care. From assessment tools to real-world examples, this guide helps nurses and families navigate acuity levels.

Explore five essential strategies for maintaining hospice GIP compliance, including documentation best practices, staff preparedness, and emerging technological solutions. This guide helps hospice organizations navigate complex regulatory requirements while ensuring quality patient care.

This comprehensive guide provides essential insights into recognizing and addressing delirium in terminally ill individuals. It’s an invaluable resource for nurses, caregivers, and families, offering practical advice and empathetic support.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

This article delves into the challenges faced by family caregivers in hospice and palliative care, offering practical strategies and resources to support them in their indispensable roles.

This article offers insight into the complexities of dementia’s progression, providing families and caregivers with the knowledge to differentiate between everyday fluctuations and actual advancements in stages.

This article delves into the transformative role of caregiver training in boosting Hospice CAHPS scores. Drawing on recent studies and expert insights, we explore practical strategies for enhancing caregiver education, ultimately leading to improved patient care and higher satisfaction ratings.

Discover how to manage wandering in dementia with practical strategies. Learn to create a safe environment and prevent risks effectively.

Creating a safe space for dementia patients involves innovative techniques like camouflage to prevent wandering. By disguising doors as walls or windows, caregivers can reduce elopement risk and ensure a secure, comforting environment. Learn how these methods can enhance safety and dignity.

Discover Bullosis Diabeticorum, a rare skin condition in people with diabetes causing painless blisters. Learn how to identify, treat, and care for loved ones with BD and a terminal illness.
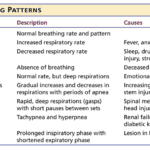
Understanding breathing patterns in end-of-life care is crucial for providing comfort to your loved one. Learn about regular vs. irregular breathing rhythms and when to contact hospice for additional support.
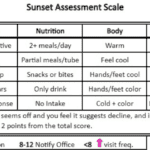
Discover how the Sunset Assessment Scale guides hospice nurses in determining visit frequencies, ensuring compassionate, patient-centered care during the final journey.
Dementia can lead to aggressive behavior in elderly patients, causing distress for both them and their caregivers. This comprehensive guide explores the underlying causes of aggression, from sleep disturbances to medication side effects, and offers practical, empathetic strategies for managing these challenging situations and improving the quality of life for all involved.

Vitamin B deficiencies can lead to severe health issues mimicking terminal diseases like nerve damage, anemia, and increased cancer risk. This comprehensive guide explores the symptoms, causes, diagnosis, and treatment options for vitamin deficiencies B1, B2, B3, B5, B6, B7, B9, and B12. Understand the importance of adequate vitamin B intake for energy production, metabolism, cell growth, and overall well-being.
Explore the complex world of dementia-related aggression and learn how to identify its underlying causes. This comprehensive guide offers insights into medication-related issues, pain management, and non-pharmacological interventions. Discover compassionate care strategies to support patients and caregivers on this challenging journey.
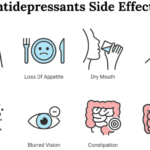
Dive into the world of Selective Serotonin Reuptake Inhibitors (SSRIs) and their role in treating depression. Discover the importance of medication half-life, the risks of serotonin syndrome, and why the chemical imbalance theory of depression is being challenged. Learn about the concerns of overprescription in older adults.
Hospice care focuses on comfort, not curing illness. But what if an emergency arises? This guide explains when hospice covers emergency care, how to proceed, and how hospice services continue during/after hospitalization - ensuring you make informed decisions without losing benefits.
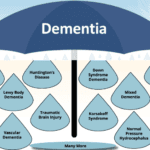
This article is like a flashlight in the dark. It’s here to shine a light on the path ahead, even when we don’t have all the answers. We’ll talk about how dementia can affect people differently and share some common signs that can help you guess what stage your loved one might be in.

Medications like anticoagulants, antidepressants, and NSAIDs can cause harm to hospice patients. Learn how to balance comfort and safety with individualized care.
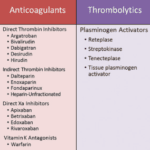
Anticoagulants can prevent blood clots but also cause bleeding risks for terminally ill patients. This article explains why these medications should be regularly reviewed for deprescribing, outlining factors like prognosis, preferences, and palliative care options to consider when making informed, compassionate choices aligned with the patient's goals.

This article discusses the importance of quarterly medication reconciliation for terminal patients and their families. It explains the benefits, such as improving patient safety, quality of life, symptom management, and the challenges and solutions. It also addresses the need to re-evaluate certain medications, like donepezil and memantine, for patients with dementia as their disease progresses.
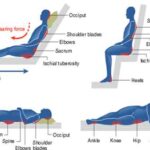
This guide provides practical strategies for preventing and managing pressure injuries in terminally ill patients. Learn how to assess risk, optimize nutrition, reposition properly, choose support surfaces, and care for the skin. Get recommendations for home, hospice, and hospital settings, as well as pain management and infection control. Empower yourself with evidence-based tips to improve your loved one's comfort and quality of life.

Lymphedema is a chronic condition that affects millions of people worldwide, especially those who have undergone cancer treatment or have other lymphatic disorders. It occurs when the lymphatic system, which drains excess fluid and waste from the tissues, is damaged or blocked. The most common symptom of lymphedema is swelling of the affected limb, which can range from mild to severe. Lymphedema can have a significant impact on the quality of life of patients with serious illnesses, such as cancer, heart failure, or chronic kidney disease. In this article, we will discuss hospice best practices for the management of lymphedema, with a focus on the needs and preferences of terminally ill patients, family members, and caregivers.
Dementia affects memory, thinking, and behavior, presenting challenges for patients and caregivers. This article discusses the best products for managing these challenges, enhancing quality of life for those with dementia.