Category: Nurse Skills
Articles involving nursing skills and techniques.
Articles involving nursing skills and techniques.
Identifying end-stage Parkinson's for hospice admission can be challenging. This article explores key criteria, including decline in function, weight loss, swallowing difficulties, and mobility issues. Learn how hospice professionals assess patients and utilize guidelines to ensure appropriate and timely hospice care for those with advanced Parkinson's disease.

Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.
This guide covers the essentials of palliative sedation for hospice patients, including ethical dilemmas, timing, recommended medications, and monitoring effectiveness, ensuring comfort during the end-of-life journey.

Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients' better quality of life.

This guide covers how to write effective hospice nursing narratives, key documentation areas, and the importance of detailed and negative-based wording to support continued hospice eligibility.
As a hospice nurse, you are vital in providing compassionate care to terminally ill patients and their families. To ensure the best possible outcomes, you rely on a systematic approach known as ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation. This process guides you in delivering holistic and individualized care, addressing not only the physical needs of patients but also their emotional, spiritual, and psychosocial well-being.

As a hospice admission nurse, asking the right questions is crucial for assessing patients' eligibility and providing compassionate care. This article explores critical questions to understand the patient's condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a "good death" for patients and families.
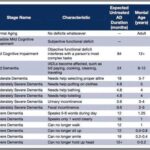
As a nurse who has cared for many terminally ill individuals with Alzheimer's disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer's disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
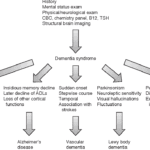
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care
Hospice care in facilities can face challenges due to facility policies, staffing issues, and lack of coordination with hospice providers. This article sheds light on the struggles patients, families, and hospice nurses face in ensuring timely, appropriate care.
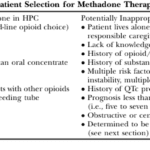
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.

If you or someone you love has a serious illness that cannot be cured, you may have heard of hospice care. Hospice care is a special kind that focuses on making the patient comfortable and peaceful in their final days. Hospice care also supports the family and caregivers emotionally and spiritually.
When a patient joins hospice care, they will have a special meeting with a hospice nurse. This meeting is called the post-admission visit. It is an especially important visit because it will help the patient and the family get to know the hospice team and learn more about the care they will receive.
This article will explain what to expect and what to ask during the post-admission visit. We will also provide tips and resources to help you and your loved one make the most of this time. We hope this article will help you feel more prepared and confident about the hospice journey.

Discover practical ways to show compassion in hospice care. Learn how small gestures like active listening, gentle touch, and respecting personal space can make a significant difference. Explore the importance of empathy, cultural sensitivity, and self-care for caregivers in providing compassionate end-of-life support.

Discover essential educational topics for hospice nurses during admission and follow-up visits. Learn how to effectively communicate with patients and families, manage symptoms, provide emotional support, and navigate end-of-life care. Enhance your skills to deliver compassionate, comprehensive hospice care.
In the world of healthcare, when a provider writes an order to "Eval and Treat" for hospice, they are asking for a thorough evaluation and a tailored treatment plan. This is specifically meant for patients who are being considered for hospice care. Let's delve into what this means and why it's crucial.
What Does "Eval and Treat" for Hospice Mean?
As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we'll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.
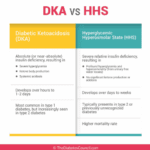
As an experienced hospice nurse, I understand that managing diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) at end of life can be challenging, especially when patients choose to stop taking their diabetic medications or when those medications are no longer an option. In this article, I will provide information on recognizing the signs and symptoms of hyperglycemic crises and outline comfort-based treatment options that align with hospice goals of care.

I know that the journey you and your loved one are on can be challenging, especially when facing a terminal illness. As an experienced hospice nurse caring for terminally ill patients, I want to provide you with some valuable insights on a common issue that may arise during this time: contractures.

Discover effective non-pharmacological methods to manage shortness of breath in hospice care. Learn about positioning techniques, breathing exercises, and environmental adjustments that can comfort and relieve patients experiencing dyspnea, enhancing their quality of life during end-of-life care.
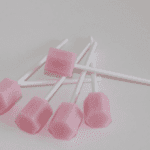
Caring for a comatose loved one during their hospice journey requires special attention, particularly when it comes to oral care. In this guide, we'll explore best practices for oral care, considering the unique needs of comatose patients, and provide you with valuable resources for further guidance.

Navigating hospice eligibility for non-Alzheimer's dementia patients demands a personalized approach. Unlike Alzheimer's, there's no definitive scale, necessitating assessments of functional decline, mobility, communication, incontinence, weight loss, overall condition, and comorbidities. Effective documentation, clinical judgment, and compassionate care are crucial for supporting these patients and families.

Caring for a loved one with dementia can be both rewarding and challenging. If your loved one has been restless throughout their life, this restlessness may continue as a symptom of their dementia. As an experienced hospice nurse, I understand the difficulties you may face in managing habitual restlessness while ensuring the safety and welfare of your loved one. In this article, I'll provide you with practical tips and evidence-based practices to create a calming environment for your loved one, even if they have trouble with fine motor control due to arthritis or other factors.