Category: Hospice
Article pertaining to Hospice to help the patient, caregivers, facility staff members, and hospice care team members prepare the patient for a “good death.”
Article pertaining to Hospice to help the patient, caregivers, facility staff members, and hospice care team members prepare the patient for a “good death.”
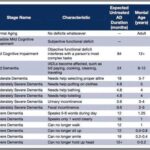
As a nurse who has cared for many terminally ill individuals with Alzheimer's disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer's disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.
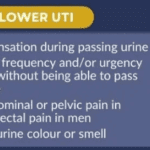
This comprehensive guide helps caregivers understand why urinary tract infections (UTIs) are prevalent in dementia patients. It provides practical advice on prevention, early detection, and effective treatment strategies. Empower yourself with the knowledge to provide the best care for your loved ones.

This article delves into the growing importance of End-of-Life Doulas in hospice care. It provides insights into their role, their support to patients and families, and their impact on the quality of end-of-life care.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
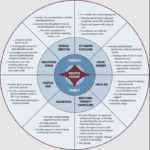
The end-of-life journey can be challenging and emotional for patients and their loved ones. A dedicated team of professionals provides comfort, support, and holistic care in hospice care. Each team member has a unique role, ensuring the patient's physical, emotional, and spiritual needs are met. Let's explore the roles of different hospice team members and how they contribute to your care journey.
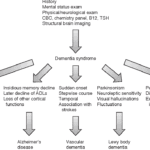
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care
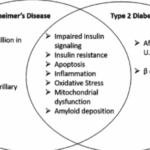
Type Three Diabetes (T3D) may hold clues to dementia. Explore the role of insulin resistance, the APOE4 gene, and personalized treatments.

This guide delves into Logopenic Primary Progressive Aphasia, a unique form of dementia. It provides crucial insights for family members and caregivers, helping them understand the condition and provide adequate care.
In the realm of nursing, the spirit of Florence Nightingale, the pioneer of modern nursing, continues to illuminate the path for nurses across various specialties. Her legacy, rooted in compassion, patient-centered care, and unwavering dedication, resonates deeply with nurses from all walks of life. However, we discover a profound connection to Florence Nightingale's nursing model within hospice nursing. This article will explore the distinctive qualities that set hospice nurses apart, including their remarkable autonomy, acute assessment skills, problem-solving abilities, and holistic approach to patient care.

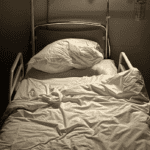
Hospice is very different from other kinds of nursing and health care. Most of us know that doctors and nurses in hospitals, clinics, nursing homes, and other places care a lot about numbers. They check your heartbeat, blood, and other things to see if they are normal. Sometimes, they do things that make you uncomfortable, like putting a tube in your nose, because they want to fix the numbers. But they don’t always think about how you feel. They are trying to fix the numbers, not you, the person. This short story shows you how non-hospice and hospice nurses are different. A hospice nurse cares more about you, the person.
Hospice care in facilities can face challenges due to facility policies, staffing issues, and lack of coordination with hospice providers. This article sheds light on the struggles patients, families, and hospice nurses face in ensuring timely, appropriate care.

This article is crafted with heartfelt understanding and care, recognizing the challenges you face as caregivers and family members of terminally ill loved ones. Our goal is to empower you with knowledge and practical advice to manage the risk of aspiration pneumonia, a common yet often preventable complication in hospice care.
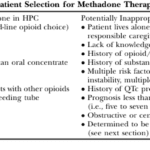
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

Deciding on a dementia care facility is crucial. This guide compares personal care homes, assisted living, memory care units, and nursing facilities, detailing Medicaid eligibility, pros and cons, and essential questions to ensure the best care for your family member.

As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.
Uncover the importance of regular care plan meetings at healthcare facilities. This guide details participants, goals, benefits, and risks of non-participation.
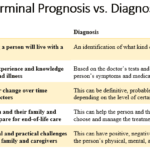
When a loved one is diagnosed with a terminal illness or a progressive disease, it can be a daunting and overwhelming experience for families and caregivers. Understanding the terms and concepts associated with these conditions is essential to providing the best possible care and support. This article aims to clarify the complex journey of terminal illnesses and progressive diseases, offering guidance and compassion to those navigating this challenging path.

Discover the essentials of Mild Cognitive Impairment (MCI) with our guide. Understand the signs, diagnosis, and ways to support loved ones facing the risk of dementia. This article provides valuable insights for patients, families, and caregivers to navigate the journey confidently.

If you or someone you love has a serious illness that cannot be cured, you may have heard of hospice care. Hospice care is a special kind that focuses on making the patient comfortable and peaceful in their final days. Hospice care also supports the family and caregivers emotionally and spiritually.
When a patient joins hospice care, they will have a special meeting with a hospice nurse. This meeting is called the post-admission visit. It is an especially important visit because it will help the patient and the family get to know the hospice team and learn more about the care they will receive.
This article will explain what to expect and what to ask during the post-admission visit. We will also provide tips and resources to help you and your loved one make the most of this time. We hope this article will help you feel more prepared and confident about the hospice journey.
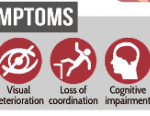
Facing Creutzfeldt-Jakob Disease (CJD) can be overwhelming, but with the right information and compassionate care, you can navigate this journey with your loved one. This guide is designed to help families new to CJD understand what to expect, recognize changes in their loved one, and provide the best care from onset
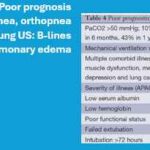
Dive into our in-depth analysis of CHF and COPD exacerbations. These critical events shape patient outcomes through expert insights and compelling case studies. Discover strategies for managing expectations and improving quality of life in the face of chronic illness.

If you or someone you love is facing a terminal illness, you may feel overwhelmed by the physical, emotional, and spiritual challenges that come with it. You may wonder how to cope with the pain, the fear, the grief, and the loss of control. You may also want to find ways to make the most of the time you have left and to leave a lasting legacy for your loved ones.
Music therapy is a form of therapy that can help you and your family deal with these issues. It involves using music and musical activities to improve the health and well-being of people of all ages and backgrounds. Music therapy can help you express your feelings, communicate with others, relax your body and mind, cope with pain and stress, enhance your spiritual connection, and create a meaningful life story.

Dive into the contrasting philosophies of purist and non-purist hospice nurses and doctors. Understand how their views on medication and patient care differ, shaping the terminal phase of a patient’s journey. This article highlights the delicate balance between medical intervention and quality of life in hospice care.

Discover practical ways to show compassion in hospice care. Learn how small gestures like active listening, gentle touch, and respecting personal space can make a significant difference. Explore the importance of empathy, cultural sensitivity, and self-care for caregivers in providing compassionate end-of-life support.