Category: Hospice Eligibility
Articles about hospice eligibility often including Medicare compliance.
Articles about hospice eligibility often including Medicare compliance.

Explore why and when Hospice General Inpatient Care (GIP) is appropriate, Medicare compliance, eligibility, and what to do if a patient is ineligible.

This comprehensive article delves into Hospice General Inpatient Care, debunks common misconceptions, and explains its importance in end-of-life care.
Learn about the essential elements of a comprehensive hospice admission note. This guide helps registered nurses document crucial patient information, from diagnoses to physical assessments, ensuring the delivery of quality end-of-life care and proper eligibility documentation.

Explore five essential strategies for maintaining hospice GIP compliance, including documentation best practices, staff preparedness, and emerging technological solutions. This guide helps hospice organizations navigate complex regulatory requirements while ensuring quality patient care.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

Understanding hospice recertification is crucial for ensuring your loved one receives the necessary care. Learn about the process, what to expect, and how to prepare.
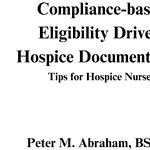
Compliance-based, Eligibility Driven Hospice Documentation: Tips for Hospice Nurses" offers comprehensive guidance for hospice professionals. This valuable resource provides practical examples for various aspects of hospice care documentation, including admissions, recertifications, IDG/IDT notes, continuous care, and GIP records. Enhance your documentation skills while ensuring regulatory compliance.

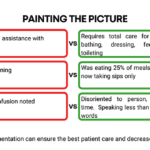
This guide covers how to write effective hospice nursing narratives, key documentation areas, and the importance of detailed and negative-based wording to support continued hospice eligibility.

As a hospice admission nurse, asking the right questions is crucial for assessing patients' eligibility and providing compassionate care. This article explores critical questions to understand the patient's condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a "good death" for patients and families.
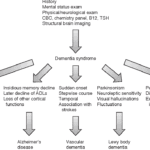
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care
In the world of healthcare, when a provider writes an order to "Eval and Treat" for hospice, they are asking for a thorough evaluation and a tailored treatment plan. This is specifically meant for patients who are being considered for hospice care. Let's delve into what this means and why it's crucial.
What Does "Eval and Treat" for Hospice Mean?

Navigating hospice eligibility for non-Alzheimer's dementia patients demands a personalized approach. Unlike Alzheimer's, there's no definitive scale, necessitating assessments of functional decline, mobility, communication, incontinence, weight loss, overall condition, and comorbidities. Effective documentation, clinical judgment, and compassionate care are crucial for supporting these patients and families.

Explore the complexities of hospice care for terminally ill patients with multiple diagnoses. Learn how to distinguish between related and unrelated conditions, understand Medicare coverage, and navigate the challenges of providing comprehensive care while adhering to hospice regulations and ethical standards.
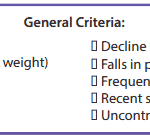
It’s essential to familiarize yourself with the key local coverage determination (LCD) facts for different terminal illnesses to avoid admitting patients who are not eligible for services only to be required to refund the money back to Medicare; otherwise, only have the patient on for one benefit period then discharged for failure to decline. These determinations provide guidelines on the coverage of hospice services for specific conditions. If you are the admitting nurse, please do not just admit because you were told to admit by someone, regardless of the position or standing of the person or party that told you to admit. Use your critical thinking and clinical judgment skills to evaluate the patient for admission. Most doctors will write "evaluate and treat" or something to that effect; never lose sight of the "evaluate" portion of the doctor's order.
Based on the provided PDF files, as noted in the resources section below, let’s explore some essential information for each terminal illness.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.
As an experienced hospice nurse, I understand how overwhelming and emotional it can be for terminally ill patients and their loved ones to navigate the hospice process. Hospice care is a compassionate and comprehensive approach to end-of-life care, designed to provide comfort, pain management, and emotional support to patients and their families. However, many people have questions about hospice eligibility and hospice recertification. In this article, I will provide a generalized guide to help you understand these important aspects of hospice care.

Hospice care focuses on providing comfort and quality of life for people with terminal illnesses and life expectancies of six months or less. While hospice care can be a difficult decision for families, it can also be a source of support and relief during a challenging time. In this article, we will explain the process of getting your loved one into hospice care and answer some common questions.
Hospice recertification is a crucial step in which the registered nurse case manager can help make the case for continued hospice eligibility. May I encourage my fellow hospice nurses to start using a template to ensure your recertification visits are consistent and that you are leading early in the documentation portion regarding what declines have occurred since admission and last recertification?
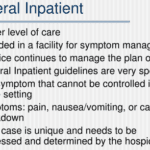
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it's readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor's orders, care plans, documentation, and education. We'll conclude with two real-life cases to illustrate these points.

If you are a new nurse to hospice, one of the tasks you probably dread is doing an admission especially if you have scheduled visits the same day as the admission.
I would like to share with you some tips that when applied may help lower your stress level, and help you remain on time even in cases where you have three to four visits including recertification to do the same day.