Category: Compliance
Articles about maintaining compliance in the field of hospice.
Articles about maintaining compliance in the field of hospice.

This guide covers critical aspects of Hospice GIP discharge planning. From initial evaluation to managing symptoms and effective discharge strategies, this article equips hospice nurses and families with the necessary knowledge for optimal care transitions.

Explore the challenges of hospice General Inpatient (GIP) care, including inappropriate billing and fraud risks. Discover how hospice RN case managers can ensure compliance and quality care through diligent oversight and documentation from admission to discharge.

Explore why and when Hospice General Inpatient Care (GIP) is appropriate, Medicare compliance, eligibility, and what to do if a patient is ineligible.

This comprehensive article delves into Hospice General Inpatient Care, debunks common misconceptions, and explains its importance in end-of-life care.
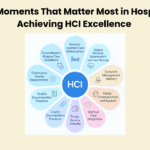
Transform your hospice's quality outcomes with Jose Escobar's proven Polaris 10/10 HCI Execution Framework. This comprehensive guide reveals the ten critical moments that drive hospice excellence and offers practical strategies for executives and clinicians to achieve perfect HCI scores.
Learn about the essential elements of a comprehensive hospice admission note. This guide helps registered nurses document crucial patient information, from diagnoses to physical assessments, ensuring the delivery of quality end-of-life care and proper eligibility documentation.
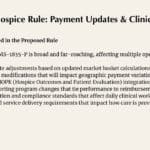
The FY2026 Hospice Proposed Rule (CMS-1835-P) introduces critical payment rate adjustments and wage index modifications that will reshape hospice operations. This comprehensive analysis examines the financial implications for providers and the direct impact on clinical managers and frontline staff delivering end-of-life care.

Explore the essential regulatory timeline requirements for hospice providers, covering everything from initial certifications to recertifications, nurse visits, and face-to-face encounters. This comprehensive guide helps ensure compliance and proper billing practices for hospice services.

Learn about the diagnosis codes not allowed as primary diagnoses on hospice claims. This guide helps hospice agencies ensure accurate billing and optimal patient care.

Discover critical approaches for hospice nurses and staff to identify and address factors leading to unnecessary discharges. This guide offers practical steps to maintain quality end-of-life care for terminal patients, fostering a stable care environment.

Explore five essential strategies for maintaining hospice GIP compliance, including documentation best practices, staff preparedness, and emerging technological solutions. This guide helps hospice organizations navigate complex regulatory requirements while ensuring quality patient care.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

This comprehensive guide explores the Hospice Outcome and Patient Evaluation (HOPE) tool and its impact on the hospice journey. It provides insights into compliance strategies, the roles of hospice team members, and the tool’s use in interdisciplinary group meetings.

Understanding hospice recertification is crucial for ensuring your loved one receives the necessary care. Learn about the process, what to expect, and how to prepare.

Hospice care is often seen as the final chapter, but sometimes, it leads to unexpected recoveries. This article explores stories of resilience and healing in hospice care, reminding us that hope and recovery can still be part of the journey.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
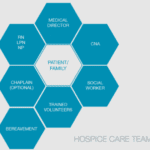
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
Compliance-based, Eligibility Driven Hospice Documentation: Tips for Hospice Nurses" offers comprehensive guidance for hospice professionals. This valuable resource provides practical examples for various aspects of hospice care documentation, including admissions, recertifications, IDG/IDT notes, continuous care, and GIP records. Enhance your documentation skills while ensuring regulatory compliance.

Hospice General Inpatient Care (GIP) provides short-term, intensive care for patients experiencing severe pain or symptoms that can't be managed at home. Learn about GIP eligibility, benefits, and how it helps both patients and families during challenging times. Discover key details and important considerations for this essential hospice service.
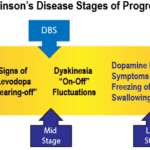
Identifying end-stage Parkinson's for hospice admission can be challenging. This article explores key criteria, including decline in function, weight loss, swallowing difficulties, and mobility issues. Learn how hospice professionals assess patients and utilize guidelines to ensure appropriate and timely hospice care for those with advanced Parkinson's disease.

This guide covers how to write effective hospice nursing narratives, key documentation areas, and the importance of detailed and negative-based wording to support continued hospice eligibility.

As a hospice admission nurse, asking the right questions is crucial for assessing patients' eligibility and providing compassionate care. This article explores critical questions to understand the patient's condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a "good death" for patients and families.
As a nurse who has cared for many terminally ill individuals with Alzheimer's disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer's disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.
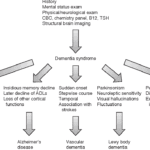
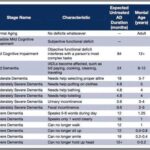
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care