Category: Best Practice
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.

Hospice providers have proven strategies to reduce symptom burden and boost satisfaction scores. Discover how combining nurse practitioner telehealth visits, educational videos, and end-of-life doula support transforms caregiver confidence and patient comfort in home-based care.

Navigating the complexities of end-of-life care can be challenging. This article delves into the nuances of terminal agitation and terminal restlessness, providing caregivers and family members with the essential knowledge to better understand and support their loved ones during the final stages of life.

Recent University of Michigan research found that benzodiazepines and antipsychotics commonly prescribed in hospice care may significantly increase mortality risk for people with dementia. This article explores these findings and provides essential advocacy guidance for families, caregivers, and hospice professionals.

Discover the transformative role of Macy catheters in hospice and palliative care. This comprehensive guide explores how these innovative devices enhance patient comfort, simplify medication administration, and support caregivers. Learn about their benefits, proper use, and impact on the quality of life for those receiving end-of-life care.

Discover how the PIE method (Problem-Intervention-Evaluation) can transform your hospice IDT note writing. This simple framework helps nurses create focused, compliant documentation even when patients are stable and well-managed.

Delve into the complexities of potentially inappropriate medications (PIMs) for older adults, especially those in hospice and palliative care. This comprehensive guide explores identification, risks, and alternatives to PIMs, providing valuable insights for healthcare professionals to enhance medication safety and quality of life for geriatric patients.
Discover essential techniques for hospice and palliative care nurses to identify subtle changes in patients' level of consciousness. This comprehensive guide covers assessment methods, red flags, and best practices for enhancing patient care—valuable insights for neurological nursing specialists and those aspiring to specialize in this field.

Understanding the potential risks associated with certain medications in the geriatric population is crucial. This article explores the top five medication classes that require close monitoring to reduce the incidence of syncope, falls, and mortality events in older adults. Learn how to optimize medication management for safer patient care.

The BEERS Criteria is vital for improving medication safety in older adults. This article explores the importance of regularly reviewing these guidelines, discussing the frequency of reviews, the potential risks of inappropriate medications, and how healthcare providers can implement effective medication management strategies for geriatric patients.

This guide covers critical aspects of Hospice GIP discharge planning. From initial evaluation to managing symptoms and effective discharge strategies, this article equips hospice nurses and families with the necessary knowledge for optimal care transitions.
This comprehensive guide helps patients, families, and healthcare professionals confidently navigate POLST decisions. Learn the essential steps, understand your options, and ensure your end-of-life care wishes are honored through proper planning and communication.
Learn about the essential elements of a comprehensive hospice admission note. This guide helps registered nurses document crucial patient information, from diagnoses to physical assessments, ensuring the delivery of quality end-of-life care and proper eligibility documentation.

Explore the essential regulatory timeline requirements for hospice providers, covering everything from initial certifications to recertifications, nurse visits, and face-to-face encounters. This comprehensive guide helps ensure compliance and proper billing practices for hospice services.

Learn about the diagnosis codes not allowed as primary diagnoses on hospice claims. This guide helps hospice agencies ensure accurate billing and optimal patient care.

Discover how acuity impacts hospice care. From assessment tools to real-world examples, this guide helps nurses and families navigate acuity levels.

Explore five essential strategies for maintaining hospice GIP compliance, including documentation best practices, staff preparedness, and emerging technological solutions. This guide helps hospice organizations navigate complex regulatory requirements while ensuring quality patient care.

This guide helps families of terminally ill patients comprehend absolute vs. relative risk reduction. It’s a resource for making educated choices about medication continuation, tapering, or cessation in collaboration with healthcare professionals.

This article delves into the transformative role of caregiver training in boosting Hospice CAHPS scores. Drawing on recent studies and expert insights, we explore practical strategies for enhancing caregiver education, ultimately leading to improved patient care and higher satisfaction ratings.

This comprehensive guide explores the Hospice Outcome and Patient Evaluation (HOPE) tool and its impact on the hospice journey. It provides insights into compliance strategies, the roles of hospice team members, and the tool’s use in interdisciplinary group meetings.
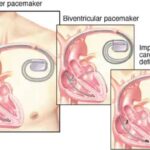
Learn about the differences between pacemakers and ICDs, their functions, and the implications for patients and caregivers. Discover why pacemakers should stay on, and ICDs should be turned off at the end of life for comfort and dignity.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
Dive into the world of Selective Serotonin Reuptake Inhibitors (SSRIs) and their role in treating depression. Discover the importance of medication half-life, the risks of serotonin syndrome, and why the chemical imbalance theory of depression is being challenged. Learn about the concerns of overprescription in older adults.

Medications like anticoagulants, antidepressants, and NSAIDs can cause harm to hospice patients. Learn how to balance comfort and safety with individualized care.