Category: Dying Process
Articles on the dying process covering the transitioning stage and the active stage of dying including the last hours of life.
Articles on the dying process covering the transitioning stage and the active stage of dying including the last hours of life.

I have cared for many terminally ill patients over the years. One question that comes up frequently is should the dying patient be on oxygen at the end of life?
I see it from both sides, from hospice intake personnel as well as the admitting nurse — all had it drilled into them over the years that low oxygen saturation must be treated — to families who see how hospital and nursing home staff rush to put someone on oxygen because of low oxygen saturation.
Contrary to widespread belief, most dying patients do not need oxygen. Here’s why:

Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.
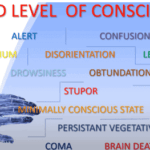
Understanding drowsiness, lethargy, and obtundation is crucial in hospice care. Drowsiness is a normal sleepiness, lethargy is more profound tiredness, and obtundation indicates severe unresponsiveness. Recognizing these levels helps in providing the right care and comfort for terminally ill patients.

I have worked with countless terminally ill patients and their families. One of the most important aspects of hospice care is ensuring that the patient and their loved ones are prepared for the end of life.
In this article, I will cover the topics that hospice nurses should discuss with patients and caregivers to ensure a good death.
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.

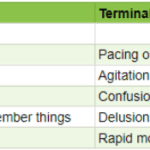
Terminal restlessness is a common phenomenon that occurs in the final stages of life. It is characterized by agitation, confusion, and distress. It can be challenging to recognize and manage, especially in patients who cannot communicate verbally. This article aims to share insights and tips from a hospice worker who learned how terminal restlessness can manifest differently in nonverbal patients and how to cope.
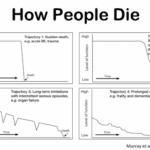
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.

Dying is an inevitable facet of life, a natural progression that touches us all. This journey towards the end of life can unfold in diverse ways—peaceful and graceful or turbulent and fraught with stress. Amid this journey, there exists a phase known as the "rally." It occurs just before the final moments of a person's life. This rally phase often shrouds itself in misunderstanding and misconceptions. It's imperative to unravel what it truly signifies.

LUnderstanding the physical and emotional changes can be crucial as a loved one nears the end of life. This guide explores common signs of approaching death, offering insights on breathing changes, skin mottling, and decreased consciousness. Learn how to provide comfort and support during this final journey.

This article explores the delicate balance of providing food and liquids to the dying and navigating the complexities of end-of-life care. It addresses the emotional and ethical considerations, offering guidance for caregivers during this profound phase.

The dying process involves physical and emotional changes as the body shuts down. As the heart weakens, circulation slows, leading to cold hands and feet, pale skin, and drowsiness. Breathing becomes irregular and shallow. The patient may experience delirium or visions. Providing comfort through pain management, emotional support, and spiritual care is crucial.

When a loved one nears the end of life, it’s natural to worry about their nutrition and hydration. This article explains why they may not need food or water and how you can provide comfort during this time.

When I first started working in the field of hospice, my clinical manager told me (I’m paraphrasing), one day you will be able to walk into the room, and without getting a single vital sign, just by visual observation, be able to tell that the person is dying or will be shortly dying. That was about three years ago. Today, it’s almost chilling for me (as it is both a blessing and tremendous responsibility) to be able to share she told the truth, and that over time — if you give yourself patience and grace and take the time to listen, observe, and remember — you too will learn how to tell when someone is close to or otherwise is dying.
Please allow me to share some of my insight as to how I know a person has less than a month left to live, and often far less. First off, let’s go into the important discussion you should have with the family, friends, and the patient themselves that provides an overall background to the prognosis. That discussion should be centered around what types of decline (downward, negative) changes have been taking place in the patient’s life over the last six months making note as to whether the decline is minor, medium, or major and the frequency (once a month, once a week, etc.) of those changes.

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.