Understanding and Caring for Your Loved One with Liver Cancer
Published on February 19, 2024
Updated on November 19, 2025
Published on February 19, 2024
Updated on November 19, 2025
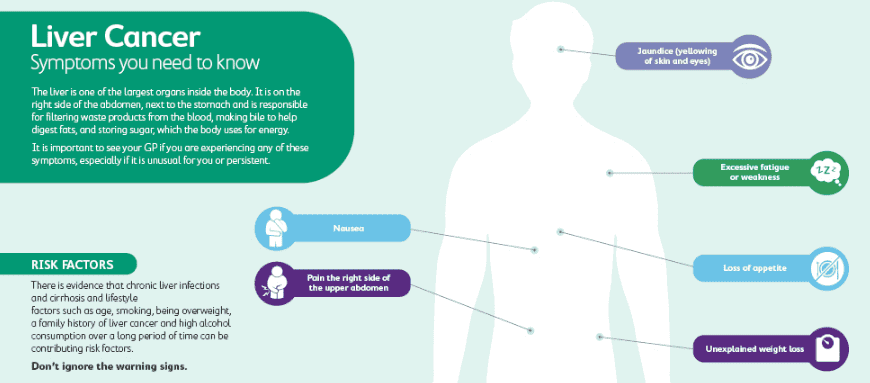
Table of Contents
Liver cancer can significantly affect your loved one’s health and well-being. As a hospice-registered nurse case manager, I’m here to help you understand what to expect during this journey and how to provide the best possible care. Remember, I’m here to offer guidance and support every step of the way.
Liver cancer is a severe disease that affects the organ that helps your body digest food and filter out toxins. Several factors, such as chronic infection, alcohol abuse, or genetic mutations, can cause it. Depending on the type and stage of the cancer, your loved one might have different treatment options and outcomes.
Early Stages: In the early stages of liver cancer, symptoms might not be very noticeable. Your loved one may experience fatigue, weight loss, and abdominal discomfort. They might also have jaundice, which causes their skin and eyes to turn yellow. These signs should prompt a visit to the doctor for proper diagnosis and treatment.
The doctor will perform some tests, such as blood tests, imaging tests, or biopsies, to confirm the presence and extent of the cancer. The doctor will also assign a stage to the cancer, ranging from stage I to stage IV, based on how large the tumor is and whether it has spread to other parts of the body. The stage will help determine the best treatment plan for your loved one.
The treatment options for early-stage liver cancer might include surgery, ablation, embolization, or targeted therapy. These treatments aim to remove or destroy the cancer cells while preserving as much healthy liver tissue as possible. Your loved one might need to undergo one or more of these treatments, depending on their situation. They might also need medications or supplements to support their liver function and overall health.
Progression: As the cancer progresses, symptoms might become more pronounced. Your loved one could experience pain in the upper abdomen, loss of appetite, and nausea. They might also feel weak and have difficulty concentrating. Communicating openly with their medical team about any changes in their condition is crucial.
The doctor will monitor the treatment’s response and side effects and adjust it as needed. The doctor might also suggest some palliative care options, such as pain management, nutrition support, or emotional counseling, to improve your loved one’s quality of life. These options can help your loved one cope with the physical and emotional challenges of living with liver cancer.
Advanced Stages: In the advanced stages of liver cancer, symptoms can become more severe. Your loved one might have swelling in the abdomen and legs due to fluid buildup. Fatigue and weakness might increase, making it hard for them to perform daily tasks.
The treatment options for advanced-stage liver cancer might include chemotherapy, immunotherapy, or clinical trials. These treatments aim to slow down the growth and spread of cancer cells and boost the immune system’s ability to fight the disease. However, these treatments might not be effective for everyone and might cause serious side effects. Your loved one might need to weigh the benefits and risks of these treatments with their doctor.
At this stage, it is essential to focus on your loved one’s comfort and dignity. You can help them by providing physical, emotional, and spiritual support. You can also seek help from hospice care, a specialized service that provides compassionate care for people with terminal illnesses and their families. Hospice care can help your loved one manage their symptoms, relieve pain, and fulfill their wishes.
Caring for a loved one with liver cancer can be challenging and stressful. You might feel overwhelmed, scared, or angry at times. You might also neglect your own needs and well-being. That’s why it’s essential to take care of yourself as well. You can get enough rest, eat well, exercise, and find healthy ways to cope with your emotions. Contact your family, friends, or support groups for help and comfort.
Liver cancer can cause many changes in your loved one’s physical and mental state. These changes can vary depending on the stage and type of cancer, the treatment they receive, and their response. Some of these changes might be subtle, while others might be more noticeable. It’s essential to observe these changes and report them to their medical team, as they may indicate a need to adjust treatment or care.
Physical Changes: Watch for changes in their appearance, such as jaundice, weight loss, and swelling. Jaundice is a condition that causes the skin and eyes to turn yellow due to the buildup of a substance called bilirubin in the blood. This can happen when the liver is not working well. Weight loss can occur when the cancer affects the appetite, metabolism, or digestion. Swelling can happen when the cancer blocks the blood flow in the liver, causing fluid to accumulate in the abdomen or legs. These changes can affect your loved one’s comfort and self-esteem, so it’s vital to help them feel as comfortable and confident as possible.
Energy Levels: Notice if your loved one becomes increasingly tired and has trouble staying active. Fatigue is a common symptom of liver cancer, as the cancer consumes energy and nutrients from the body. Fatigue can also be a side effect of some treatments, such as chemotherapy or radiation. Your loved one might need more rest and sleep and have difficulty doing their usual activities. It’s important to respect their energy limits and help them balance rest and activity. You can also encourage them to do gentle exercises, such as walking or stretching, to improve their blood circulation and mood.
Pain and Discomfort: Be attentive to signs of pain, discomfort, or changes in their pain pattern. They might express discomfort in the abdomen or other areas. Pain can be caused by the tumor pressing on nerves, organs, or bones or by the treatments that damage healthy cells. Pain can also affect your loved one’s mood, sleep, and appetite. It’s important to help your loved one manage their pain effectively by following their doctor’s instructions on pain medications and by using other methods, such as massage, heat, or relaxation techniques, to ease their discomfort.
Appetite and Hydration: Monitor their eating habits and fluid intake. If they struggle to eat or drink, discussing this with their medical team is important. Liver cancer can affect the appetite, digestion, and absorption of nutrients, making it hard for your loved one to eat enough and stay hydrated. Some treatments, such as chemotherapy or radiation, can also cause nausea, vomiting, or mouth sores, which can make eating and drinking unpleasant. Your loved one might need to eat smaller, more frequent meals and avoid spicy, fatty, or hard-to-digest foods. They might also need to drink more fluids, such as water, juice, or broth, to prevent dehydration. You can help your loved one by preparing nutritious and appetizing foods and offering them drinks and snacks throughout the day.
Liver cancer can be a stressful and challenging experience for both you and your loved one. You might feel overwhelmed, scared, or helpless at times. You might also wonder how best to care for your loved one and make them feel comfortable and supported. Here are some tips that might help you:
Open Communication: Maintain open and honest conversations with your loved one about their needs, fears, and wishes. This will help you provide care that aligns with their preferences. You can also use this opportunity to express your feelings and concerns and to strengthen your bond. You don’t have to talk about everything at once, but check in with your loved one regularly and listen to what they say. You can also ask them if they want to talk to anyone else, such as a counselor, a spiritual leader, or a support group.
Comfort Measures: Focus on keeping your loved one comfortable. Position changes, gentle massages, and pain management techniques can make a significant difference. You can help your loved one find a comfortable position that eases their breathing and reduces pressure. You can also give them a gentle massage on their back, shoulders, or feet to relax their muscles and improve their blood flow. You can also help them manage their pain by following their doctor’s instructions on pain medications and using other methods, such as heat, ice, or distraction, to ease their discomfort.
Nutrition: Offer small, frequent meals that are easy to digest. Include foods they enjoy and can tolerate. Hydration is essential, so encourage them to sip water throughout the day. Liver cancer can affect the appetite, digestion, and absorption of nutrients, making it hard for your loved one to eat enough and stay hydrated. Some treatments, such as chemotherapy or radiation, can also cause nausea, vomiting, or mouth sores, which can make eating and drinking unpleasant. Your loved one might need to eat smaller, more frequent meals and avoid spicy, fatty, or hard-to-digest foods. They might also need to drink more fluids, such as water, juice, or broth, to prevent dehydration. You can help your loved one by preparing nutritious, appetizing meals and offering drinks and snacks throughout the day.
Emotional Support: Emotions can run high during this time. Be a listening ear, offer reassurance, and let them express their feelings without judgment. Your loved one might experience a range of emotions, including anger, sadness, fear, and guilt. They might also feel isolated, depressed, or hopeless. Acknowledging their feelings and letting them know they are not alone is essential. You can also reassure them by reminding them of their strengths, their achievements, and their support network. You can also help them cope with their emotions by using positive affirmations, relaxation techniques, or humor.
Engage in Activities: Depending on their energy levels, engage in activities they enjoy. It could be as simple as reading a book, watching a movie, or spending time outdoors. Engaging in activities can help your loved one maintain their interest, sense of purpose, and connection with others. It can distract them from their pain and worries, boosting their mood and self-esteem. You can help your loved one by suggesting activities that suit their preferences and abilities and joining them in doing them. You can also respect their need for privacy and solitude and let them have some time for themselves.
There may come a time when the cancer treatment is no longer working, and your loved one is nearing the end of life. This can be an exceedingly difficult and emotional time for both of you. You may feel sad, angry, scared, or numb. You may also have many questions and concerns about what will happen and how to help your loved one. This section will give tips on providing end-of-life care and ensuring comfort and peace for your loved one.
Hospice Care: Hospice care focuses on making your loved one as comfortable as possible in the last months, weeks, or days of life. Hospice care does not try to cure cancer or prolong life but rather to relieve pain and other symptoms, such as nausea, shortness of breath, or anxiety. Hospice care also provides emotional and spiritual support for your loved one and family. Hospice care can be given at home, in a hospital, or at a hospice facility, depending on your loved one’s needs and preferences. You can help your loved one by:
Emotional Well-being: The end of life can be a time of mixed emotions for your loved one and family. Your loved one may feel grateful, peaceful, or relieved but also sad, angry, or scared. They may also have regrets, unfinished business, or unfulfilled dreams. You can help your loved one by:
Caring for a loved one with liver cancer can be challenging, but with knowledge and compassion, you can provide meaningful support throughout their journey. Remember, you’re not alone—contact medical professionals, support groups, and hospice services for assistance.
Caring for a Loved One with Terminal Cancer: A Guide for Families
Understanding Cancer Metastasis: A Guide for Patients and Families
Liver Cancer – Symptoms, Causes, Types, Complications and Prevention
American Cancer Society – Liver Cancer
American Society of Clinical Oncology – Liver Cancer
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death