Understanding and Caring for Your Loved One with Lung Cancer
Published on March 18, 2024
Updated on June 26, 2024
Published on March 18, 2024
Updated on June 26, 2024
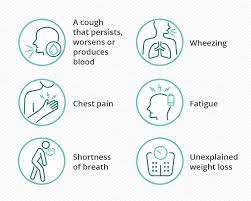
Table of Contents
Lung cancer presents a difficult path for both individuals facing illness and their loved ones. As a dedicated hospice registered nurse case manager specializing in end-of-life care, I aim to equip you with essential insights. This guide aims to enlighten you about the stages of the disease, detect crucial shifts in your dear one’s condition, and deliver optimal care from inception to closure. By sharing this knowledge, I intend to empower you to provide tender and considerate assistance throughout this profound journey.
Lung cancer is a severe disease that affects the lungs, the organs that help us breathe. Lung cancer can make it hard to breathe and cause other problems in the body. Lung cancer can also change over time and become more severe. This is called progression.
Progression means the cancer cells grow and spread to other parts of the lung or the body. Doctors use different stages to describe how far the cancer has progressed. Knowing the stage of lung cancer can help you and your loved one plan the best treatment and care.
Lung cancer has four main stages, from stage 1 to stage 4. Each stage has distinctive characteristics and needs several types of care. The stages are:
Stage 1: Cancer is confined to the lung. This means the cancer cells are only in one part of the lung and have not spread elsewhere. Stage 1 lung cancer is the earliest and easiest to treat. People with stage 1 lung cancer may have surgery to remove the cancerous part of the lung. They may also have radiation therapy or chemotherapy to kill any remaining cancer cells.
Stage 2: Cancer has spread to nearby areas. This means the cancer cells have moved to the nearby lymph nodes, the small glands that help fight infections. Stage 2 lung cancer is still treatable but may need more aggressive treatment. People with stage 2 lung cancer may have surgery, radiation therapy, chemotherapy, or a combination of these treatments.
Stage 3: Cancer has spread to lymph nodes and other organs. This means the cancer cells have reached the lymph nodes on the other side of the chest or neck. They may also have spread to other organs near the lungs, such as the heart, the esophagus, or the trachea. Stage 3 lung cancer is more challenging to treat and may not be curable. People with stage 3 lung cancer may have radiation therapy, chemotherapy, immunotherapy, or targeted therapy. These treatments use drugs or other substances to attack the cancer cells.
Stage 4: Cancer has spread extensively. This means that the cancer cells have spread to distant organs, such as the brain, the liver, the bones, and the adrenal glands. Stage 4 lung cancer is the most advanced and the hardest to treat. People with stage 4 lung cancer may have palliative care, which is care that focuses on relieving pain and improving quality of life. They may also have some of the treatments mentioned above to slow cancer growth or reduce symptoms.
Lung cancer can affect your loved one in many ways. As the cancer grows and spreads, it can cause different problems in the body. Some of these problems may be hard to deal with. You and your loved one may need to adjust to these changes and find ways to cope. Here are some common changes that your loved one may experience:
Breathing difficulties: Lung cancer can make it hard for your loved one to breathe. They may feel short of breath, wheeze, or gasp for air. This can make them feel scared or anxious. To help them breathe easier, you can:
Fatigue: Lung cancer can make your loved one feel tired and weak. They may not have the energy to do what they used to do. This can make them feel frustrated or depressed. To help them cope with fatigue, you can:
Coughing, sometimes with blood: Lung cancer can cause your loved one to cough a lot. Sometimes, they may cough up blood or mucus. This can be alarming and uncomfortable. To help them ease their cough, you can:
Loss of appetite and weight loss: Lung cancer can affect your loved one’s appetite and digestion. They may not feel hungry or enjoy food as much as before. They may also lose weight or have trouble swallowing. This can affect their nutrition and health. To help them maintain their weight and appetite, you can:
Pain or discomfort: Lung cancer can cause pain or discomfort in different body parts. The pain may be dull, sharp, or throbbing. It may be constant or come and go. Pain can affect your loved one’s mood and sleep. To help them relieve their pain, you can:
Changes in mood and energy levels: Lung cancer can affect your loved one’s emotions and mental health. They may feel sad, angry, scared, or hopeless. They may also have trouble concentrating, remembering, or sleeping. These changes can affect their quality of life and relationships. To help them cope with their emotions, you can:
Lung cancer can be hard to deal with, not only for the person who has it but also for the people who love them. If you are caring for someone with lung cancer, you may feel overwhelmed or stressed. You may wonder how to help them best and make them feel better. Caring for your loved one involves addressing their physical and emotional needs. Here are some tips on how to do that:
Your loved one may feel more comfortable if you create a calm and soothing environment for them. This can help them relax and cope with their symptoms. To create comfort, you can:
Your loved one may feel scared, sad, angry, or lonely because of their lung cancer. They may need your emotional support to cope with their feelings. To provide emotional support, you can:
Your loved one may experience various symptoms because of their lung cancer. These symptoms can affect their quality of life and well-being. To help them manage their symptoms, you can:
There may come a time when the cancer treatment is no longer working, and your loved one is nearing the end of life. This can be an exceedingly difficult and emotional time for both of you. You may feel sad, angry, scared, or numb. You may also have many questions and concerns about what will happen and how to help your loved one. This section will give tips on providing end-of-life care and ensuring comfort and peace for your loved one.
Hospice Care: Hospice care focuses on making your loved one as comfortable as possible in the last months, weeks, or days of life. Hospice care does not try to cure cancer or prolong life but rather to relieve pain and other symptoms, such as nausea, shortness of breath, or anxiety. Hospice care also provides emotional and spiritual support for your loved one and family. Hospice care can be given at home, in a hospital, or at a hospice facility, depending on your loved one’s needs and preferences. You can help your loved one by:
Emotional Well-being: The end of life can be a time of mixed emotions for your loved one and family. Your loved one may feel grateful, peaceful, or relieved but also sad, angry, or scared. They may also have regrets, unfinished business, or unfulfilled dreams. You can help your loved one by:
Lung cancer is a hard and long journey that can make you and your loved one feel many things. You may feel sad, scared, angry, or hopeful. You may also feel confused, overwhelmed, or helpless. These are normal feelings, and you are not alone.
As a hospice nurse, I want to help you and your loved one through this journey. I want to give you information and advice to make you feel more confident and prepared. I want to help you support your loved one as best as possible.
The most important thing you can do is understand lung cancer stages and what they mean. The stages tell you how far the cancer has spread and what kind of treatment and care your loved one needs. Knowing the stage can help you plan and make decisions with your loved one and their healthcare team.
Another important thing you can do is to communicate openly with your loved one and their healthcare team. You can talk to your loved one about their feelings, wishes, and goals. You can also ask questions, share concerns, and express your needs. Communication can help you and your loved one feel closer and more supported.
The last important thing you can do is to prioritize comfort for your loved one and yourself. You can create a comfortable and soothing environment for your loved one by using pillows, blankets, music, or aromatherapy. You can also provide emotional support by listening, hugging, or sharing memories. You can also help your loved one manage their symptoms by giving them medications, fluids, or foods. Comfort can help your loved one feel more relaxed and peaceful.
By doing these things, you can show your love and care for your loved one, make their journey more meaningful and dignified, take care of yourself and your well-being, and be a great caregiver and companion for your loved one.
Caring for a Loved One with Terminal Cancer: A Guide for Families
Understanding Cancer Metastasis: A Guide for Patients and Families
American Lung Association Lung Cancer Staging
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death