Understanding AL Amyloidosis: A Family’s Guide to Care, Comfort, and Hope
Published on June 2, 2025
Updated on June 2, 2025
Published on June 2, 2025
Updated on June 2, 2025
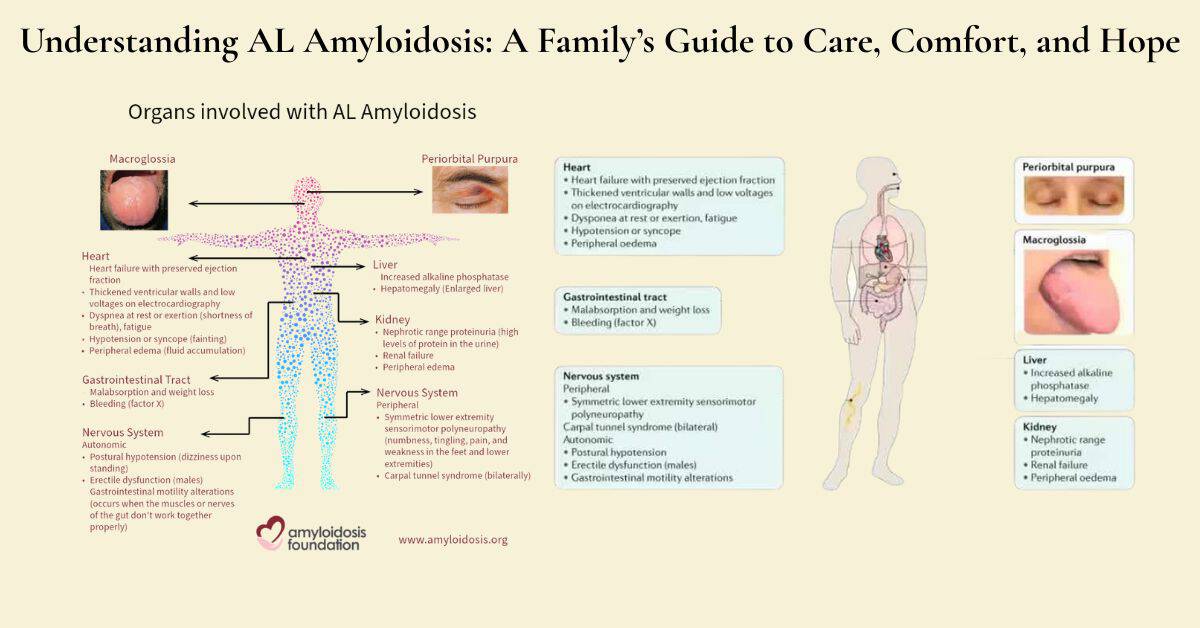
Table of Contents
If you or someone you love has been diagnosed with AL amyloidosis, you’re probably feeling overwhelmed and have many questions. This article is written specifically for patients with AL amyloidosis, their caregivers, and family members who want to understand this condition better.
This comprehensive guide will help you understand:
This article is designed for individuals without a medical background who seek clear and honest information about AL amyloidosis. Whether you’re:
You’ll find practical information you can use right away.
Knowledge brings power and a sense of peace of mind. When you understand what’s happening with AL amyloidosis, you can:
Understanding this condition helps families work together as a team during a challenging time.
AL amyloidosis is a condition in which your body produces abnormal proteins that clump together and accumulate in your organs. Think of it like having sticky clumps that don’t belong there, making it harder for your organs to work properly.
How is AL amyloidosis different from other types? There are several types of amyloidosis, but AL amyloidosis comes from problems with your plasma cells (a type of white blood cell). Other types might be caused by:
Why is it called a “rare disease?” AL amyloidosis affects only about 8-12 people out of every million each year. To put this in perspective, it’s much rarer than diabetes or heart disease.
Which organs are commonly involved?
Why do symptoms vary so much between patients?
Every person’s AL amyloidosis is unique because the abnormal proteins can deposit in different organs and at different rates. One person might have mostly heart problems, while another has kidney issues.
The role of abnormal proteins:
Your plasma cells normally make helpful antibodies to fight infection. In AL amyloidosis, they produce misfolded proteins that clump together, much like tangled yarn, thereby interfering with normal organ function.
Symptoms that often bring people to the doctor:
Many people with AL amyloidosis first visit their doctor because they feel unusually tired or short of breath. You might notice:
Why diagnosis can take time:
AL amyloidosis is often called a “great mimicker” because its symptoms look like many other conditions. Your doctor might first think you have heart problems, kidney disease, or nerve issues. Getting the correct diagnosis can take months because:
Questions to ask your healthcare team:
Blood and urine tests explained simply:
Your doctor will look for abnormal proteins in your blood and urine. These tests check for light chains – the faulty proteins that cause AL amyloidosis. You’ll give blood samples and collect urine over a 24-hour period.
Biopsy procedures and what to expect:
A biopsy takes a tiny piece of tissue to examine under a microscope. The doctor might take samples from your fat pad (near your belly button), bone marrow, or affected organs. Most biopsies use local numbing medicine, which feels like a pinch.
Understanding your test results:
Your doctor will explain if abnormal proteins are present and which organs they’re affecting. Request written copies of the results and don’t hesitate to ask questions if anything is unclear.
AL amyloidosis affects everyone differently, making it impossible to predict exactly how your journey will unfold. No two people have identical experiences with this condition, which can feel frustrating but is entirely normal.
Why each person’s experience is different:
Your body is unique, and AL amyloidosis deposits abnormal proteins in different organs at different rates. One person might have mostly heart problems, while another experiences kidney issues first. Your age, overall health, and the speed at which you receive treatment all play essential roles in your individual experience.
Factors that influence disease progression:
Understanding “good days” and “difficult days”:
You’ll likely notice some days feel better than others. Good days might include increased energy, improved appetite, and reduced shortness of breath. Difficult days often bring increased fatigue, breathing problems, or swelling. This pattern is normal and doesn’t mean your treatment isn’t working.
Early stage – what to expect:
You might feel tired more often and notice mild swelling in your legs. Many people can still do most daily activities with some adjustments.
Progressive stage – changing needs:
Symptoms become more noticeable. You may need help with household tasks and experience more frequent medical appointments.
Advanced stage – focusing on comfort:
The focus shifts to managing symptoms and maintaining quality of life. Comfort becomes the primary goal rather than fighting the disease.
Shortness of breath and fatigue are often the first signs that AL amyloidosis is affecting your heart. You might notice feeling winded when climbing stairs or doing activities that used to be easy for you. This happens because abnormal proteins cause your heart muscle to become stiff and less effective at pumping blood.
Swelling in the legs and abdomen occurs when your heart can’t pump blood well enough to keep fluid from building up. You might notice:
When symptoms signal progression:
Changes in urination can include producing less urine than usual, urine that appears foamy or bubbly, or needing to urinate more frequently at night. These changes happen when protein deposits damage your kidneys’ filtering system.
Protein in urine makes your urine look foamy, like beaten egg whites. This means your kidneys aren’t working properly to keep important proteins in your blood where they belong.
Managing fluid balance becomes important as kidney function changes. Your doctor might recommend:
Nerve problems and numbness often begin in the hands and feet, causing tingling, burning, or loss of sensation. This can make it harder to button clothes or experience fluctuations in hot and cold temperatures.
Digestive issues include feeling full quickly, nausea, or changes in bowel movements. These happen when protein deposits affect your digestive system.
Skin changes and bruising occur because AL amyloidosis affects blood clotting. You might bruise easily, especially around your eyes, or notice small red spots on your skin.
Understanding these symptoms helps you know when to call your healthcare team and what changes to expect as the condition progresses.
Living with AL amyloidosis means working closely with your healthcare team to find the right combination of treatments. The good news is that several options are available to help slow the disease and manage your symptoms.
Medications that can help slow progression:
Your doctor may prescribe treatments that target the abnormal plasma cells causing AL amyloidosis. These might include:
Treatments for specific symptoms:
Different organs affected by AL amyloidosis need different approaches:
Working with your healthcare team:
Building a strong relationship with your medical team is essential. Here’s how to make the most of your appointments:
Managing AL amyloidosis symptoms at home requires practical strategies that you and your caregivers can use daily. These approaches focus on keeping you as comfortable as possible.
Managing shortness of breath:
Breathing problems can be frightening, but there are many ways to find relief:
Dealing with fatigue and weakness:
Extreme tiredness is common with AL amyloidosis, but you can learn to work with your energy levels:
Nutrition and eating challenges:
Eating problems are common, but small changes can make a big difference:
Pain management strategies:
Pain doesn’t have to control your life. There are many ways to find relief:
AL amyloidosis affects more than just your body – it impacts your emotions, relationships, and daily life. Taking care of your mental and social well-being is just as crucial as managing physical symptoms.
Coping with uncertainty:
Living with a rare disease like AL amyloidosis means dealing with many unknowns, which can feel overwhelming:
Maintaining relationships and activities:
AL amyloidosis may change your abilities, but it doesn’t have to end meaningful connections and activities:
Finding support groups and resources:
You don’t have to face AL amyloidosis alone. Many resources are available to help:
Remember, asking for help is a sign of strength, not weakness. Building a strong support network will help you navigate this journey with greater confidence and peace of mind.
When someone you love has AL amyloidosis, the word “hospice” might feel scary or overwhelming. Many people think hospice means giving up, but that’s not true at all. Understanding what hospice really offers can help you make the best decisions for your loved one.
What hospice care really means:
Hospice is a specialized type of medical care that focuses on comfort, dignity, and quality of life, rather than attempting to cure the disease. It’s provided by a team of healthcare professionals who understand how to manage symptoms and support both patients and families during difficult times.
Hospice care includes:
How is it different from giving up hope?
Choosing hospice care is not giving up hope – it’s changing what you hope for. Instead of hoping for a cure, you’re hoping for:
Many families find that hospice care actually gives them more control over their situation, not less. You get to focus on what matters most instead of spending time in hospitals or dealing with treatments that aren’t helping anymore.
The focus on comfort and quality of life:
Hospice care prioritizes your loved one’s comfort above all else. This means:
Deciding when to consider hospice care can be one of the hardest decisions families face. Here are some signs that might indicate it’s time to have this conversation.
Physical changes that indicate progression:
When treatments are no longer helping:
You might notice that:
Quality of life considerations:
Consider hospice when:
Deciding on hospice care is deeply personal and should involve everyone who matters to your loved one.
Having conversations with family:
Start by talking openly about:
Remember, it’s okay to have different opinions at first. Take time to listen to each other and focus on what would make your loved one most comfortable.
Questions to ask your doctor:
When talking with your healthcare team, ask:
What hospice eligibility looks like for AL amyloidosis:
For someone with AL amyloidosis to qualify for hospice care, doctors typically look for:
| Heart-Related Signs | Kidney-Related Signs | General Signs |
|---|---|---|
| Severe shortness of breath at rest | Significant protein in urine | Weight loss or poor appetite |
| Heart function is getting worse | Fluid buildup that won’t improve | Frequent infections |
| Needing oxygen most of the time | Kidney function declining | Multiple hospital visits |
| Chest pain that’s hard to control | Swelling that keeps getting worse | Sleeping most of the day |
The good news is that hospice eligibility doesn’t mean you have to stop all treatments. Some medications that help with comfort, like those for pain, breathing, or swelling, can often continue under hospice care.
Most importantly, remember that choosing hospice care means prioritizing what matters most: comfort, dignity, and spending quality time together as a family. It’s a decision made with love, not one that gives up on hope.
When your loved one with AL amyloidosis enters hospice care, they’ll receive comprehensive support from a dedicated team of professionals who understand how to provide comfort during this difficult time. Understanding what hospice care provides can help ease your worries and help you focus on what matters most: spending quality time together.
Nurses, doctors, and other specialists
Your hospice nurse will become your primary point of contact and will visit regularly to assess your loved one’s comfort and adjust care as needed. The hospice medical director or your family doctor will oversee medical care, prescribing medications and treatments focused on comfort rather than cure. You may also work with:
Social workers and chaplains
The social worker helps your family navigate practical concerns, such as insurance questions, advance directives, and community resources. They also provide emotional support and can help resolve family conflicts that sometimes arise during stressful times.
Chaplains provide spiritual care regardless of your religious beliefs or lack thereof. They’re trained to support people of all faiths and can help with life review, forgiveness work, or simply listening to concerns about what comes next.
How the team works together
The hospice team meets regularly, at least every 15 days, to discuss your loved one’s care and make adjustments as needed. Each team member brings their expertise to create a comprehensive plan that addresses physical symptoms, emotional needs, and spiritual concerns. Your family’s input is essential in these discussions, and the team will always respect your loved one’s wishes and values.
Medical equipment and supplies
Hospice provides all necessary medical equipment at no cost to your family, including:
All supplies related to your loved one’s care are also provided, such as wound care materials, incontinence products, and any other comfort items needed.
Medication management
Hospice covers all medications related to your loved one’s terminal diagnosis and comfort care1. This includes:
Your hospice team will teach you how to give medications safely and when to call for help.
Respite care for families
Caring for someone with AL amyloidosis can be exhausting. Hospice provides several types of respite care:
Bereavement support
Hospice support doesn’t end when your loved one dies. Bereavement services continue for at least 13 months and include:
Managing breathing problems
Shortness of breath is common with AL amyloidosis, but hospice has many ways to help:
Controlling pain and discomfort
Pain management is a top priority in hospice care. Your team will:
Maintaining dignity and independence
Hospice care focuses on preserving your loved one’s dignity and supporting as much independence as possible:
Creating meaningful moments
Hospice understands that this time is precious, and they help families make the most of it:
The hospice team recognizes that every family is different, and they’ll work with you to create an environment where your loved one feels safe, comfortable, and surrounded by love. Their goal is to help you focus on being together rather than worrying about medical details or care logistics.
Remember, choosing hospice care means prioritizing comfort and quality time together. The comprehensive support provided by the hospice team allows families to concentrate on what truly matters during this critical time in their lives.
Being a caregiver for someone with AL amyloidosis is both a privilege and a challenge. You’re providing essential support during a difficult time, but it’s important to know that you don’t have to do this alone. With practical strategies and the right support, you can provide excellent care while also taking care of yourself.
Practical daily care tips
Caring for someone with AL amyloidosis requires attention to their changing needs while maintaining their dignity and comfort. Here are practical ways to help:
Managing daily activities:
Monitoring symptoms:
Safety considerations:
Recognizing when to call for help
Knowing when to contact your healthcare team can prevent emergencies and provide peace of mind. Call your doctor or hospice team when you notice:
Immediate concerns requiring same-day contact:
Concerns to report within 24 hours:
Taking care of yourself, too
Caregiver burnout is real and common. Your well-being matters not just for you, but for your ability to provide good care. Here’s how to stay healthy:
Physical self-care:
Emotional self-care:
Practical support:
Talking about difficult topics
Having meaningful conversations about AL amyloidosis and its impact can strengthen your relationship and help everyone feel more prepared. These conversations don’t have to happen all at once – they can unfold over time.
Starting difficult conversations:
Topics that might come up:
Communication tips:
Making memories and saying what matters
This time together is precious, and there are many ways to create meaningful moments and preserve important memories.
Simple memory-making activities:
Expressing important feelings:
Involving children and grandchildren appropriately
Children can be a valuable source of joy and connection, but they require age-appropriate guidance to understand what’s happening.
For young children (ages 3-7):
For school-age children (ages 8-12):
For teenagers:
Guidelines for all ages:
Remember that supporting your loved one with AL amyloidosis is a marathon, not a sprint. Take it one day at a time, celebrate small moments of joy, and don’t hesitate to ask for help when you need it. Your love and presence make a tremendous difference, even when the situation feels overwhelming.
Planning ahead when you or a loved one has AL amyloidosis can feel overwhelming, but taking these steps early can provide peace of mind and ensure your wishes are honored. Having these crucial conversations and organizing resources while you’re feeling well gives you more control over your future care.
Advance directives and healthcare wishes
Advance directives are legal documents that tell your healthcare team and family what kind of medical care you want if you become unable to speak for yourself. These documents become especially important with AL amyloidosis because the disease can sometimes affect thinking or make communication difficult.
Key documents you should consider:
Important topics to discuss and document:
Tips for these conversations:
Financial and legal considerations
AL amyloidosis can create significant financial challenges, so planning ahead can help protect your family’s financial security.
Important financial documents to organize:
Healthcare-related financial planning:
Legal considerations:
End-of-life preferences
Talking about end-of-life preferences isn’t about giving up hope – it’s about making sure your final days reflect what matters most to you.
Important topics to discuss:
Funeral and memorial planning:
National organizations and websites
Several national organizations provide excellent information and support for people with AL amyloidosis and their families.
| Organization | What They Offer | How to Find Them |
|---|---|---|
| Amyloidosis Foundation | Patient education, support groups, and research updates | Search online for “Amyloidosis Foundation” |
| International Myeloma Foundation | Information about plasma cell disorders, including AL amyloidosis | Look for “International Myeloma Foundation” |
| Leukemia & Lymphoma Society | Financial assistance, patient education, and support services | Search “Leukemia Lymphoma Society” |
| National Organization for Rare Disorders | Information about rare diseases and resources | Find “NORD rare diseases” online |
What these organizations typically provide:
Local support groups
Finding local support can make a huge difference in how you cope with AL amyloidosis.
Where to find local support:
Types of local support available:
Benefits of joining support groups:
Financial assistance programs
The cost of treating AL amyloidosis can be overwhelming; however, several programs are available to provide support.
Types of financial assistance available:
Medication assistance programs:
General financial assistance:
Healthcare-specific assistance:
How to apply for assistance:
Tips for managing healthcare costs:
Remember, asking for help is not a sign of weakness – it’s a smart way to ensure you and your family have the support you need during this challenging time. Many people find that planning ahead and connecting with resources actually reduces anxiety and helps them focus on what matters most: spending quality time with loved ones and maintaining the best possible quality of life.
The key is to start these conversations and research these resources while you’re feeling well enough to make thoughtful decisions. Your healthcare team, especially social workers, can be invaluable in helping you navigate these necessary planning steps.
Living with AL amyloidosis is undoubtedly challenging, but you don’t have to face this journey alone. Throughout this guide, we’ve covered essential information to help you understand the disease, manage symptoms, and make informed decisions about your care. As you move forward, remember that knowledge is power, and having the right support makes all the difference.
Key takeaways for families
As you navigate AL amyloidosis together, keep these important points in mind:
Understanding leads to better care: The more you know about AL amyloidosis, the better you can work with your healthcare team to manage symptoms and make treatment decisions. Don’t hesitate to ask questions – your medical team wants to help you understand what’s happening.
Every person’s journey is unique: AL amyloidosis affects everyone differently, so try not to compare your experience to others. Focus on your loved one’s specific needs and symptoms rather than worrying about what might happen based on someone else’s story.
Quality of life matters most: Whether you’re in the early stages of the disease or considering hospice care, the goal is always to maintain the best possible quality of life. This means managing symptoms effectively, staying connected with loved ones, and focusing on what brings comfort and joy.
Communication is essential: continue to talk with each other about your fears, hopes, and needs. These conversations may be difficult, but they help everyone feel more prepared and connected during challenging times.
It’s okay to ask for help: From medical professionals to family and friends, accepting support is not a sign of weakness. Building a strong support network helps individuals cope more effectively with the challenges ahead.
The importance of hope and comfort
Hope doesn’t disappear when someone has AL amyloidosis – it simply changes form. Initially, you may hope for effective treatments and a slowing of disease progression. As the condition advances, hope might shift toward comfortable days, meaningful conversations, and peaceful moments together.
Hope can look like:
Comfort becomes increasingly important as AL amyloidosis progresses. This doesn’t mean giving up – it means shifting focus to what matters most: reducing pain and breathing problems, staying connected with loved ones, and ensuring your family member feels safe and cared for.
Remember that choosing comfort care, including hospice when appropriate, is an act of love that honors your family member’s dignity and well-being. It’s about living as fully as possible for whatever time remains.
Moving forward with knowledge and support
As you continue this journey, you’re now equipped with necessary knowledge about AL amyloidosis, symptom management, and care options. Use this information to advocate for the best possible care and to make decisions that align with your family’s values and wishes.
Steps to take moving forward:
Stay connected with your healthcare team: Regular communication with doctors, nurses, and other specialists ensures that care plans can be adjusted as needs change. Don’t wait until problems become severe – reach out when you notice changes in symptoms or have concerns.
Build and maintain your support network: Whether through family, friends, support groups, or community organizations, having people who understand and care makes an enormous difference. Don’t be afraid to lean on others when you need help.
Take care of caregivers too: If you’re caring for someone with AL amyloidosis, remember that your well-being matters. Seek respite care, talk to counselors, and accept help from others so you can continue providing good care without burning out.
Plan ahead when possible: Having conversations about healthcare wishes, financial planning, and end-of-life preferences while everyone is feeling relatively well reduces stress and ensures important decisions reflect your loved one’s true wishes.
Focus on what you can control: While you can’t control AL amyloidosis itself, you can control how you respond to it. Choose to focus on comfort, connection, and making the most of each day rather than dwelling on uncertainties about the future.
Remember that this journey, while difficult, can also include moments of deep connection, love, and meaning. Many families find that facing AL amyloidosis together strengthens their relationships and helps them appreciate what truly matters in life.
You have the knowledge, resources, and support to navigate this path with dignity and hope. Take it one day at a time, celebrate small victories, and remember that love and care make all the difference in how this journey unfolds.
Your courage in facing AL amyloidosis, whether as a patient or caregiver, is remarkable. Trust in your ability to handle whatever comes next, knowing that you’re not alone and that help is always available when you need it.
Coping with Amyloidosis Webinar, April 17, 2021
Comprehensive Review of AL amyloidosis: some practical recommendations
The patient’s perspective on the symptom and everyday life impact of AL amyloidosis
Mastering Hospice Eligibility: An Essential Guide for RNs and Clinical Managers
Clinical Pathophysiology: A Reference for Hospice and Palliative Nurses
Clinical Practice Guidelines for Quality Palliative Care, 4th edition
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.