Trigger Words for Hospice Nurses: Assessing End-of-Life in Two Weeks or Less
Published on September 27, 2023
Updated on November 6, 2024
Published on September 27, 2023
Updated on November 6, 2024
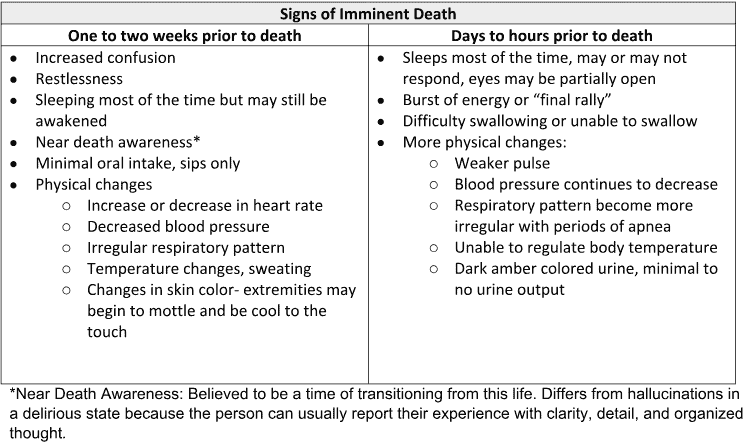
Table of Contents

Hospice visits by a nurse should always include a discussion with the caregiver and family members or facility staff about any changes since the last nursing visit. This interviewing process is critical because vital signs do not always provide clear indications when a patient is two weeks or less away from death. Suppose we hear or read certain words or phrases in the notes. In that case, we should be on high alert for the possibility that the patient is either transitioning towards actively dying or is otherwise close to transitioning.
Communicating any observed changes to the hospice team is essential, as they can provide guidance and support based on their professional experience. However, the specific signs and timeline can vary from person to person. Hospice nurses and caregivers work together to ensure the patient’s comfort and dignity during this stage of life.
When a patient begins to sleep for extended periods, it can be a sign that their body is conserving energy as it approaches the end of life. The body’s systems gradually slow down, increasing the need for rest. Hospice nurses often observe that patients in their final weeks experience drowsiness and fatigue, leading to prolonged periods of sleep. Decreased physical activity is a natural response as the body shifts focus from sustaining everyday functions to preparing for the final stages.
The phrase “eating bites and sips” resonates deeply in hospice care. As patients approach the end of life, their appetite and interest in food diminish. This can be attributed to the body’s declining metabolic needs and the redirection of energy from digestion to more vital functions. Consuming only insignificant amounts of food symbolizes the body’s transition from nourishment to acceptance of its impending journey. Caregivers and family members might notice their loved ones taking fewer bites and sips as the body’s energy requirements decrease, providing an opportunity for them to offer comfort through companionship rather than insisting on food intake.
During the advanced stages of a patient’s life-limiting illness, changes in consciousness can become apparent, offering insights into their physiological and neurological state. Confusion and disorientation may arise as the body redirects its resources towards vital functions, leaving less energy for cognitive processes. This cognitive fog can lead to patients becoming increasingly unaware of their surroundings, disoriented about time and place, and struggling to recognize familiar faces. Another significant change is the potential for a patient to become non-responsive. This state is often described as a deep sleep-like condition where the patient is difficult to rouse, responds minimally to external stimuli, and might have extended periods of unresponsiveness. These changes reflect the body’s natural progression towards the end of life, as it reallocates resources to focus on essential functions while allowing the patient to retreat from the external world. For caregivers and hospice professionals, recognizing these shifts in consciousness is vital for providing appropriate care and ensuring the patient’s comfort during their final journey.
A patient’s breathing pattern can change significantly as the body’s systems gradually shut down. Breathing might become irregular, shallow, or labored. This can be distressing for both caregivers and family members to observe. Still, it’s crucial to understand that changes in breathing are a part of the body’s natural progression toward the end of life. Additionally, patients might exhibit behaviors like “picking at things not present.” This can be attributed to altered mental states and a shifting focus of attention. Hospice nurses, caregivers, and family members must offer a serene and calming environment, ensuring the patient’s comfort throughout this process.
One of the heartrending aspects of the end-of-life journey is the patient’s inclination to communicate with loved ones who have already passed away. This phenomenon is often seen as a way for patients to find solace and reassurance as they prepare to cross the threshold of life. The phrase “speaking to loved ones passed” signifies a deep emotional and spiritual process. As caregivers and family members witness this, it’s important to recognize it as a natural response to the transition, offering a chance to provide comfort and companionship during this time of reflection and connection.
Expressing farewells and closure takes on profound meaning as a patient nears the end of their life. Phrases such as “telling family members they will die very soon” might arise from a patient’s desire to prepare their loved ones emotionally. These conversations, while difficult, allow patients to find peace and resolution in their relationships. Simultaneously, caregivers and family members may notice increased physical weakness in their loved ones. This weakness is often a result of the body’s systems slowing down and the muscles gradually losing their strength. Physical support and reassurance can enhance the patient’s comfort during this time.
As a patient’s body approaches the end of life, various physiological changes occur, often manifesting through skin color and temperature alterations. A noticeable drop in body temperature can result from the gradual slowing of metabolic processes, and this cooling effect may be felt by caregivers when they touch the patient’s skin. Additionally, the skin might assume a pale or mottled appearance, indicative of reduced blood circulation as the body prioritizes vital organs. This change in skin color, coupled with the coolness, occurs as a natural response to the body’s focus on conserving energy for its essential functions during the final stages of life. While these shifts can be disconcerting to witness, they underline the body’s preparation for the imminent transition, signaling that the patient is moving toward the final moments of their journey.
The experience of pain and discomfort can take on unique dimensions as a patient nears the end of their life. While discomfort is common in serious illnesses, an escalation in pain that is no longer effectively managed by medication might signify that the patient is reaching a critical stage in their journey. The phrase “Hurts all over” can be particularly telling, indicating a widespread and intense level of discomfort transcending localized pain. This marked increase in pain might stem from a range of factors, including the body’s diminishing ability to respond to medication, shifting metabolic priorities, or the progression of the underlying condition. This sign is crucial for caregivers and hospice professionals, as it can provide insight into the patient’s overall condition and evolving needs. Addressing pain and discomfort at this stage becomes a matter of medical intervention and providing the patient with the highest possible quality of life during their last moments.
Understanding the trigger words that could signify a patient’s imminent passing is a profound aspect of providing compassionate end-of-life care. For hospice nurses, caregivers, and family members, these cues offer an opportunity to create an environment of love, support, and dignity. While these trigger words can provide insight into a patient’s condition, it’s important to remember that everyone’s journey is unique. Consulting with experienced hospice professionals and maintaining open communication can ensure that the patient’s needs are met in the most caring and empathetic manner possible. The focus remains on embracing the patient’s last moments with respect, comfort, and grace.
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
The Importance of Caregiver Journaling
Reporting Changes of Condition to Hospice
Interviewing and Observation as part of the Hospice Assessment
Breathing Patterns Before End of Life: Critical Clues for the Last Hours!
Signs that someone is in their last days or hours of life
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
On Grief and Grieving: Finding the Meaning of Grief Through the Five Stages of Loss
Finding Meaning: The Sixth Stage of Grief
It’s OK That You’re Not OK: Meeting Grief and Loss in a Culture That Doesn’t Understand
Need Help Dealing with Grief? GriefShare Grief & Loss Support Groups Are Here for You
Children’s Grief Resources
For Ages 4-6
For Ages 6-8
For Ages 8-10
For Ages 11-13
For Ages 13-18
Specialized Grief Resources
Young Adult Literature Exploring Grief:
Helpful Online Resources
Enhanced Online Resources for Teens
Specialized Teen Platforms
Comprehensive Teen Support Centers
Interactive Support Options
Educational Resources for Teens and Families