Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.
As an experienced hospice visiting registered nurse, today offered me profound insights from two interconnected perspectives. The first highlights the blind trust we often place in facility nurses and doctors when caring for our loved ones. The second involves the challenges I encountered while advocating for proper end-of-life care for a patient with Alzheimer's.

In the realm of hospice care, compassion and comfort take precedence. A team of skilled professionals comes together to offer comprehensive support to patients, their families, and caregivers. Among these essential contributors, Certified Nursing Assistants (CNAs) stand out as unsung heroes, bringing immeasurable value to the field of hospice care. This article delves into the distinctive role CNAs play in hospice, their frequent and meaningful interactions, and their leadership within the hospice team.
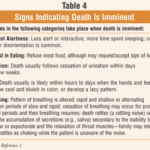
For a non-healthcare professional who has never witnessed death before, it can be unsettling to be present with someone who is nearing the end of their life. However, there are certain signs and observations that you can make using your senses that may indicate that the person you are with may pass away within seconds, minutes, or hours. Understanding these signs can help you provide support and comfort to the individual and their loved ones during this grim time.
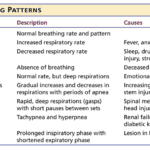
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.
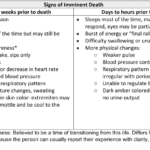
Losing a loved one is an incredibly challenging and emotional experience. If you find yourself in the presence of someone in the transitioning phase of the dying process, knowing what signs to look for can be helpful. Although every individual's experience may vary, some common observations may indicate someone is in the transitioning phase. Here's a guide to help you recognize these signs and provide support during this grim time.

It's common in nursing to be told by others that you shouldn't be a nurse, and some may even call you a "fake nurse" if you don't meet their standards of what they think is required to be a nurse. The first time I was told I could not be a nurse was by an elderly woman who believed only women could be nurses.
Dying doesn’t always hurt. The amount and type of pain there is at the end of life can differ. The specific diagnosis and cause of pain are factors.
Is it Too Early to Start Hospice?
It's crucial to remember that hospice care is about improving the quality of life for the patient and their family, regardless of the time left. Hospice care can be initiated when the patient's condition is declining and they require comfort-focused care rather than life-prolonging treatments. Starting hospice care early can provide ample time for the patient and their family to benefit from the support and services offered.
If you're unsure when to consider hospice care, consult the patient's primary physician or a hospice care provider. They can guide you through the process and help you make an informed decision based on the patient's needs and circumstances.

Explore the delicate balance of IV fluid use at life’s end. This article discusses the hospice approach, potential risks, and prioritizing comfort over invasive measures. A must-read for families facing tough decisions in palliative care.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.

Caring for a terminally ill loved one can be challenging. Still, with the proper support and understanding, you can help ensure they experience a comfortable and dignified end of life. Hospice care offers specialized medical and emotional support during this time. This guide aims to empower families new to hospice services by providing essential information on what to expect from a hospice provider and how to manage the journey towards a good death.
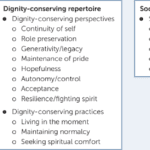
Educating nursing home staff on hospice care priorities like shifting focus from vital signs to comfort, managing symptoms like pain/breathlessness, providing psychosocial support, end-of-life planning, and bereavement care is crucial. Hospice emphasizes quality of life over curative treatments. Effective symptom management through medications and non-pharmacological approaches enhances patient comfort. Open communication, empathy, and respecting patient autonomy are essential. Hospice prepares families for the dying process and grief counseling.

The longer I work in hospice, the more I'm reminded about two critical pieces of wisdom: 1) Hospice is about living, and 2) we should all do our best to live a life of least regrets.
While this article is geared towards family members with a terminally ill loved one, as well as my fellow workers in the fields of palliative and hospice care, I believe the thoughts that I will share apply to everyone alive near and far.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

Considering tube feeding for a loved one who is in the last year of life. This intervention may not improve quality of life and can lead to discomfort, reduced mobility, and complications. Learn about the risks and make informed decisions for their end-of-life care.

When it comes to hospice care, one common question that arises is whether terminally ill patients should continue seeing their regular doctor or specialists. As an experienced hospice nurse, I have witnessed the benefits and challenges of maintaining these relationships. In this article, we’ll explore the pros and cons of hospice patients still visiting their general practitioners and specialists from the perspective of patients and their families.

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?
As a hospice registered nurse, I have encountered numerous heartwarming and challenging experiences throughout my career. One of the most memorable encounters was with a dementia patient, Miss Norma Jean Smith, who affectionately called me "Jack." This endearing nickname, born out of her unique perception, became a symbol of the special bond we shared. In the following account, I will share the poignant journey of building trust, providing compassionate care, and embracing the unexpected moments of joy and sorrow in the life of Miss Norma. This story is a testament to the profound impact of person-centered care and the invaluable lessons learned from the patients we are privileged to serve.

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.

There is a spiritual connection in hospice, dealing with death and dying forty-plus hours per week. We who are in the field see it often, but there are times when we hear it firmly from the patients and families whom we serve. Let me share the most recent event on Memorial Day, 5/29/2023, week.

One of the most important roles is detecting and managing infections in terminally ill geriatric patients with dementia. These patients are often at higher risk for infections due to their weakened immune systems, underlying health conditions, and limited mobility. Detecting infections in these patients can be challenging due to their limited communication abilities and other cognitive and physical impairments. However, early detection and management of infections can significantly improve the patient’s quality of life and potentially prolong their life.
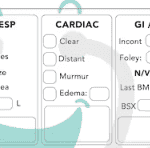
Hospice nurses play a vital role in providing quality care and comfort to terminally ill patients and their families. They must make accurate and timely assessments of the patient’s condition, needs, and preferences every visit. This article will outline the key aspects that hospice nurses should assess every visit, in addition to the standard physical assessment.

As a hospice RN case manager, I have seen many ethical dilemmas arise in end-of-life situations. Hospice care is unique because it focuses on providing comfort care to patients no longer seeking curative treatment for their illnesses. As a result, the ethical concerns in hospice care differ from those in other healthcare settings. This article will explore some ethical dilemmas that can arise in hospice care and how they can be addressed.
Before I review several case studies gathered from the sources in the resource section below, please allow me to share a current one of mine that is ongoing as this article is being published.