As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we’ll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.
Understanding Patient Acuity
Patient acuity is a crucial concept that shapes the level of care and attention a patient needs based on their medical condition, symptoms, and overall health. In hospice care, assessing patient acuity is essential for determining the appropriate frequency of nurse visits. Let’s delve deeper into what patient acuity entails and how it guides the planning of nurse visits for terminally ill patients.
Patient acuity reflects the complexity and severity of a patient’s health condition. It encompasses numerous factors, including:
- Medical Condition: The nature and stage of the patient’s illness or disease. Some patients may have more advanced or aggressive forms of cancer, heart failure, dementia, or other terminal conditions that require more frequent monitoring and intervention. Other patients may have more stable or manageable diseases that do not pose immediate threats to their health or comfort.
- Symptom Severity: the intensity and extent of the patient’s physical and psychological symptoms. Some patients may suffer from severe pain, nausea, shortness of breath, anxiety, depression, or other distressing symptoms that affect their quality of life and comfort. Other patients may have mild or moderate symptoms that can be controlled with medication or non-pharmacological measures.
- Functional Status: The patient can perform daily activities and tasks independently. Some patients may have limited mobility, strength, or coordination that prevents them from caring for themselves or their environment. They may need assistance bathing, dressing, feeding, toileting, or transferring. Other patients may have more functional abilities that allow them to maintain some degree of autonomy and dignity.
- Psychosocial Needs: Emotional and social factors that impact the patient’s well-being and quality of life. Some patients may have complex or unresolved issues that affect their coping, such as grief, guilt, anger, fear, or spiritual distress. They may need more emotional support, counseling, or spiritual care. Other patients may have more positive or adaptive coping skills that help them accept their situation and find meaning and purpose. They may benefit from social interaction, leisure activities, or family involvement.
These factors are not static but dynamic and interrelated. They may change over time as the patient’s condition progresses or fluctuates. Therefore, nurses need to conduct regular and comprehensive assessments of the patient’s acuity and adjust the frequency of visits accordingly. The goal is to provide optimal care that meets patients’ needs and preferences while respecting their wishes and values.
Role of Patient Acuity in Nurse Visit Frequency
Determining the appropriate frequency of nurse visits in hospice care is a delicate balance that hinges on patient acuity. Here’s how patient acuity influences this decision-making process:
- Tailored Care: Patient acuity guides nurses in tailoring care plans to meet individualized needs. A patient with higher acuity may require more frequent visits to address complex symptoms and provide comfort. For example, a patient with uncontrolled pain may need daily visits to adjust their medication regimen and ensure optimal relief. Patients with lower acuity may require less frequent visits to maintain their comfort and well-being. For example, patients with stable symptoms may need weekly visits to monitor their condition and provide education and support.
- Symptom Management: Acuity helps nurses identify the level of symptom management required. Patients with severe symptoms may benefit from more frequent monitoring and interventions. For example, patients with dyspnea may need more frequent visits to administer oxygen therapy, nebulizers, or other treatments to ease their breathing. Patients with mild or moderate symptoms may benefit from less frequent monitoring and interventions. For example, patients with mild nausea may need less frequent visits to administer antiemetics or other remedies to prevent vomiting.
- Proactive Care: Monitoring patient acuity allows nurses to proactively address any deterioration in the patient’s condition. Regular assessments can lead to timely interventions and improved quality of care. For example, a patient with a sudden increase in acuity may need more frequent visits to prevent complications or crises. Patients with a gradual decrease in acuity may require less frequent visits to respect their wishes and preferences. For example, a patient nearing the end of life may prefer fewer visits to spend more time with their loved ones.
- Resource Allocation: Patient acuity assists in allocating resources effectively. High-acuity patients may require more nursing hours, whereas “well-managed” patients can receive appropriate care without unnecessary disruptions. For example, patients with multiple comorbidities may require more nursing hours to coordinate care with other providers and services. A patient with a simple diagnosis may require fewer nursing hours to provide consistent and adequate care.
Suggested Starting Scheduled Nurse Visit Frequencies
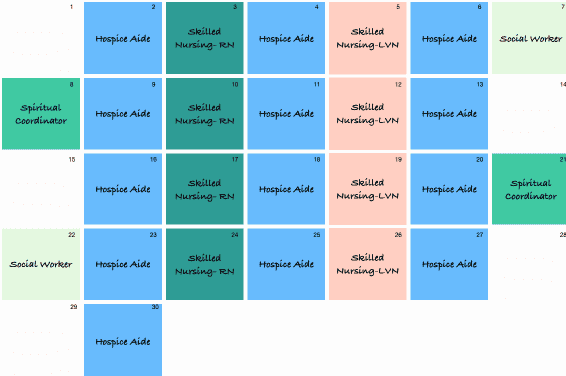
For most hospice patients, a suggested starting point for nurse visit frequencies is as follows:
- Initial Assessment: A comprehensive assessment upon admission to establish a baseline. This assessment includes a thorough evaluation of the patient’s medical history, current condition, symptoms, medications, functional status, psychosocial needs, goals of care, and preferences. The initial assessment also involves developing a care plan with the patient and their family and coordinating care with other interdisciplinary team members. The initial assessment usually takes one to two hours and is conducted within 48 hours of admission.
- Regular Visits: One to two weekly visits for patients with “well-managed” conditions. These visits involve monitoring the patient’s condition, managing symptoms, providing education and support, administering medications and treatments, documenting care, and communicating with other providers and services. The regular visits usually take 30 to 60 minutes and are scheduled according to the patient’s needs and availability. The frequency of regular visits may vary depending on the patient’s acuity, as discussed in the previous section.
Initial Assessment
The first step in providing exceptional hospice care is conducting an initial assessment upon admission. This comprehensive evaluation helps establish a baseline understanding of the patient’s medical condition, symptoms, and overall health. By gaining insights into the patient’s unique needs from the outset, you’ll be better equipped to develop a tailored care plan that ensures comfort and quality of life. It is important to note that your initial assessment may be after the patient is admitted; consider your first visit with the patient at the start of your initial assessment.
The initial assessment consists of several components, including:
- Physical Assessment: A thorough examination of the patient’s vital signs, body systems, pain level, medication regimen, and other relevant physical aspects. The physical assessment helps identify the patient’s current condition, symptom severity, and treatment effectiveness. It also helps detect potential complications or risks requiring immediate attention or intervention.
- Psychosocial Assessment: This is a holistic assessment of the patient’s emotional, mental, social, and spiritual well-being. It helps understand the patient’s coping skills, support system, cultural background, values, beliefs, and preferences. It also helps identify any psychosocial issues or needs that may affect the patient’s quality of life or comfort, such as anxiety, depression, grief, guilt, anger, fear, or spiritual distress.
- Functional Assessment: This evaluation of the patient’s ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs) helps determine the patient’s level of independence, mobility, strength, and coordination. It also helps identify functional limitations or needs that may require assistance or adaptation, such as bathing, dressing, feeding, toileting, transferring, or managing household tasks.
- Care Plan Development is a collaborative process of developing a care plan for the patient and their family based on the initial assessment findings. The care plan outlines the goals of care, the interventions and services to be provided, the frequency and duration of visits, and the roles and responsibilities of the interdisciplinary team. It is individualized, patient-centered, flexible, and reflects the patient’s wishes and values.
The initial assessment is critical in establishing a trusting and supportive relationship with the patient and their family. It is also an opportunity to educate and empower them about hospice care and their role in the care process. You can provide the best care for your hospice patients by conducting a comprehensive and empathic initial assessment.
Regular Visits
Planning one to two weekly nurse visits is a suggested starting point for patients with “well-managed” conditions. These regular visits serve several important purposes:
- Symptom Monitoring: Regular check-ins allow you to closely monitor the patient’s symptoms and overall condition. This proactive approach enables early identification of any changes that may require adjustments in the care plan. For example, a patient developing a new symptom, such as constipation, may need frequent visits to provide laxatives, fluids, or dietary changes. A patient who experiences a decrease in symptom severity, such as pain, may require less frequent visits to reduce medication dosage or frequency.
- Medication Management: Ensuring medication is administered correctly and effectively is critical to hospice care. Regular visits offer opportunities to assess medication needs and address any concerns. For example, a patient who has difficulty swallowing pills may need more frequent visits to provide alternative forms of medication, such as liquids, patches, or injections. A patient who has adverse reactions to medication, such as nausea, may need less frequent visits to provide antiemetics or other remedies.
- Emotional Support: Beyond physical care, hospice nurses provide vital emotional support. Regular visits create a consistent presence, fostering trust and rapport between you, the patient, and their family. For example, a patient who feels lonely or isolated may need more frequent visits to provide companionship, listening or validation. Patients who think peacefully or are content may require less frequent visits to respect their privacy and autonomy.
As discussed in the previous section, the frequency of regular visits may vary depending on the patient’s acuity. It is essential to communicate with the patient and their family about the rationale and expectations for the visit frequency and solicit their feedback and preferences. By providing regular visits that are appropriate and responsive to the patient’s needs, you can enhance their comfort and quality of life.
Tailoring Frequencies to Individual Needs
It’s important to note that while these suggested frequencies provide a starting point, every patient’s journey is unique. Patient acuity, symptom severity, and family dynamics all determine the optimal nurse visit schedule. As you gain familiarity with each patient’s situation, you’ll have the flexibility to adjust visit frequencies accordingly.
Some factors that may influence your decision to increase or decrease visit frequencies include:
- Changes in Patient Condition: As the patient’s condition progresses or fluctuates, their needs may also change. For example, a patient who experiences a sudden decline in health may need more frequent visits to provide comfort measures, symptom relief, and emotional support. Patients who stabilize or improve may require less frequent visits to respect their wishes and goals.
- Family Involvement: The level of family involvement may affect the amount of care and support the patient requires. For example, a patient who has a supportive and engaged family may need less frequent visits to allow the family to provide care and companionship. A patient with a distant or unavailable family may require more frequent visits to fill the gaps in care and provide social interaction.
- Patient Preferences: Ultimately, the patient’s preferences and values should guide the frequency of visits. For example, patients who prefer more contact and communication may need more frequent visits to meet their expectations and needs. Patients who prefer less intrusion and more privacy may need less frequent visits to honor their choices and dignity.
By tailoring the frequencies to individual needs, you can provide personalized and compassionate care for your hospice patients.
When to Decrease Nurse Visit Frequencies
As patients’ symptoms are well-managed, nurse visit frequencies can be decreased. This can help reduce unnecessary disruptions and respect patients’ wishes and values. Consider decreasing frequencies under the following circumstances:
- No unmanaged symptoms: When a patient’s symptoms are well controlled, they may not need as much nursing care and attention. For example, a patient who has mild or no pain, nausea, or anxiety may require less frequent visits to maintain their comfort and well-being. A patient who has severe or unrelieved symptoms may need more frequent visits to provide symptom relief and comfort measures.
- Caregiver Competence: When caregivers demonstrate the ability to manage their care effectively and the patient has no unmanaged symptoms, they may not need as much nursing support and guidance. For example, a caregiver who knows how to administer medications, monitor vital signs, and provide primary care may need less frequent visits to oversee the patient’s care. A caregiver who is unsure, inexperienced, or overwhelmed may require more frequent visits to provide education, assistance, and reassurance.
You can provide optimal care for your hospice patients by decreasing nurse visit frequencies when appropriate.
When to Increase Nurse Visit Frequencies
Increasing nurse visit frequencies may be necessary if a patient’s condition changes or deteriorates. This can help provide more intensive care and comfort for the patient and their family. Consider increasing frequencies under the following circumstances:
- Increased Symptoms: Patients with worsening symptoms may need more frequent visits to provide symptom relief and comfort measures. For example, a patient who develops severe pain, dyspnea, or agitation may need more frequent visits to adjust their medication regimen, administer treatments, or provide palliative sedation. Patients with mild or no symptoms may require less frequent visits to maintain comfort and well-being.
- Complex Care Needs: Patients who require more frequent monitoring due to complex care needs may need more frequent visits to provide coordinated and comprehensive care. For example, patients with multiple comorbidities, infections, or wounds may need more frequent visits to manage their condition, prevent complications, or provide wound care. Patients with simple or stable care needs may need less frequent visits to provide adequate and consistent care.
Increasing nurse visit frequencies allows you to provide optimal care for your hospice patients when necessary.
Continuously Adapting Care
Hospice care is a dynamic and evolving process. By remaining attentive to patient symptoms and changes in care needs, you can provide the support and compassion that define quality end-of-life care. Your dedication to adjusting nurse visit frequencies ensures that patients receive the personalized attention they deserve.
As a hospice nurse, you enhance patients’ and their families’ comfort and dignity. Understanding the factors influencing nurse visit frequencies allows you to tailor your care to meet individualized needs and preferences. By conducting regular and comprehensive assessments, you can monitor changes in patient acuity and adjust your care accordingly. You can coordinate and deliver optimal care by communicating and collaborating with the interdisciplinary team.
Nursing visit frequencies in hospice are not fixed or rigid but flexible and responsive. By continuously adapting your care, you can provide the best possible care for your hospice patients.
Conclusion
Determining the appropriate nurse visit frequencies in hospice care is not a one-size-fits-all approach but a personalized and flexible one. By carefully considering patient acuity, symptom management, and collaboration with interdisciplinary teams, you can tailor your care to meet each patient’s and their family’s unique needs and preferences. By starting with a suggested schedule, adjusting as needed, and always prioritizing patient comfort, you can provide the best possible care for your hospice patients. As a hospice nurse, you enhance patients’ and their families’ comfort and dignity. You can be proud of the compassionate and quality care you provide.
Resources
Considerations for increasing hospice visit frequencies
What Hospice Nurses should assess every visit
All hospice patients are not equal: development of a visit-based acuity index
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
The Last Hours of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles