Tag: RN Case Manager
Articles about the Hospice Registered Nurse Case Manager (RNCM) as part of the hospice care team.
Articles about the Hospice Registered Nurse Case Manager (RNCM) as part of the hospice care team.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
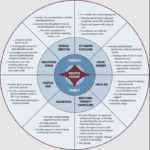
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
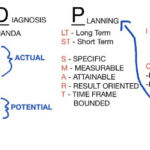
As a hospice nurse, you are vital in providing compassionate care to terminally ill patients and their families. To ensure the best possible outcomes, you rely on a systematic approach known as ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation. This process guides you in delivering holistic and individualized care, addressing not only the physical needs of patients but also their emotional, spiritual, and psychosocial well-being.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
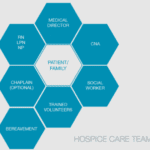
The end-of-life journey can be challenging and emotional for patients and their loved ones. A dedicated team of professionals provides comfort, support, and holistic care in hospice care. Each team member has a unique role, ensuring the patient's physical, emotional, and spiritual needs are met. Let's explore the roles of different hospice team members and how they contribute to your care journey.

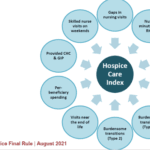
As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.

If you or someone you love has a serious illness that cannot be cured, you may have heard of hospice care. Hospice care is a special kind that focuses on making the patient comfortable and peaceful in their final days. Hospice care also supports the family and caregivers emotionally and spiritually.
When a patient joins hospice care, they will have a special meeting with a hospice nurse. This meeting is called the post-admission visit. It is an especially important visit because it will help the patient and the family get to know the hospice team and learn more about the care they will receive.
This article will explain what to expect and what to ask during the post-admission visit. We will also provide tips and resources to help you and your loved one make the most of this time. We hope this article will help you feel more prepared and confident about the hospice journey.

Discover essential educational topics for hospice nurses during admission and follow-up visits. Learn how to effectively communicate with patients and families, manage symptoms, provide emotional support, and navigate end-of-life care. Enhance your skills to deliver compassionate, comprehensive hospice care.
As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we'll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.

It's common in nursing to be told by others that you shouldn't be a nurse, and some may even call you a "fake nurse" if you don't meet their standards of what they think is required to be a nurse. The first time I was told I could not be a nurse was by an elderly woman who believed only women could be nurses.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.
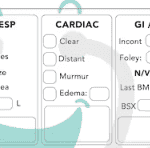
Hospice nurses play a vital role in providing quality care and comfort to terminally ill patients and their families. They must make accurate and timely assessments of the patient’s condition, needs, and preferences every visit. This article will outline the key aspects that hospice nurses should assess every visit, in addition to the standard physical assessment.

This article offers guidance for new visiting hospice nurses struggling with work-life balance. It covers strategies like maintaining a recertification journal, pre-charting before visits, assessing end-of-life status, educating families, and preparing for a "good death." By following these tips, nurses can take less work home while delivering focused, compassionate care.
Hospice care is focused on symptom management, pain relief, emotional support, and spiritual care. It is a privilege to be a part of a patient’s end-of-life journey, and as a new hospice nurse, you may feel overwhelmed, but you can make a difference in a patient’s life. One of the essential skills you need to learn as a hospice nurse is to recognize when to increase the scheduled visit frequency for a terminally ill patient under hospice care.

Our primary focus for our patients is comfort at the end of life as hospice nurses. We work tirelessly to ensure that our patients receive the best possible care during their end-of-life journey. An aspect of that care that is often overlooked, but incredibly important is timely documentation.
Documenting hospice visits at the bedside is crucial for several reasons. Not only does it help ensure that our patients are receiving the best possible care, but it also helps the hospice team as a whole and reduces issues when the caregiver must be involved in triage services. Here are just a few reasons why documenting hospice visits at the bedside is so important:
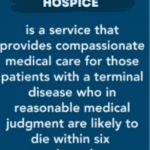
As an experienced hospice nurse, I understand how overwhelming and emotional it can be for terminally ill patients and their loved ones to navigate the hospice process. Hospice care is a compassionate and comprehensive approach to end-of-life care, designed to provide comfort, pain management, and emotional support to patients and their families. However, many people have questions about hospice eligibility and hospice recertification. In this article, I will provide a generalized guide to help you understand these important aspects of hospice care.
One of the hardest lessons to learn as a nurse, in my experience and opinion, is the psychosocial skills necessary to help patients and their families work towards their healthcare goals. These skills are applicable to every field. While I, myself, am still growing as a registered nurse (heading towards my 5th year at the time of writing this article), I would like to share with you some of the lessons learned. These lessons are based on real-life cases where I will present the scenario, what I did that worked, and what I internally thought of opposite scenarios.

If you are a new nurse to hospice, one of the tasks you probably dread is doing an admission especially if you have scheduled visits the same day as the admission.
I would like to share with you some tips that when applied may help lower your stress level, and help you remain on time even in cases where you have three to four visits including recertification to do the same day.
Here are some ideas that may be beneficial to those of you who are relatively new visiting hospice nurses:

As an INFJ, I’m almost constantly introspective. Today, I was helping with an emergency where one of our wonderful on-call nurses was in a car accident. During my visit with a patient I admitted yesterday who is transitioning towards actively dying, I was in bewilderment in my mind about how comfortable and peacefully patient I am when I’m around the terminally ill and their family.