Navigating the Minefield: Potentially Inappropriate Medications in Geriatric and End-of-Life Care
Published on September 5, 2025
Updated on August 31, 2025
Published on September 5, 2025
Updated on August 31, 2025
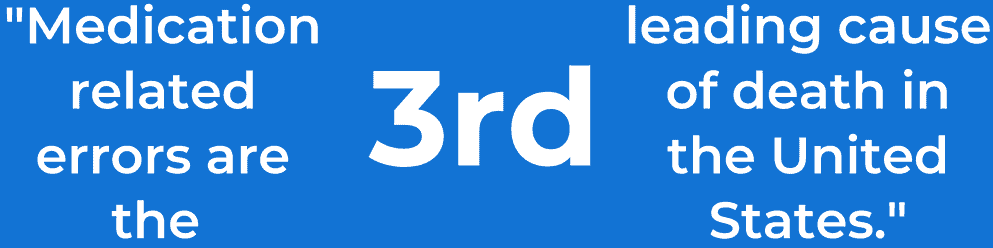
Table of Contents
As we care for our loved ones in their golden years, especially those receiving hospice care, it’s crucial to understand the medications they’re taking. Some medicines that might be safe for younger adults can pose risks to older individuals. These are called Potentially Inappropriate Medications (PIMs).
Potentially Inappropriate Medications (PIMs) are drugs that carry more risks than benefits for older adults, particularly those in hospice care. Understanding PIMs is vital because:
PIMs become significant in geriatric care due to the following:
To better understand the concept of PIMs, let’s look at a comparison between appropriate and potentially inappropriate medications for older adults:
| Medication Category | Appropriate for Older Adults | Potentially Inappropriate (PIM) |
|---|---|---|
| Pain Relief | Acetaminophen | Long-term use of NSAIDs (e.g., ibuprofen) |
| Sleep Aid | Melatonin | Long-acting benzodiazepines (e.g., diazepam) |
| Anxiety Treatment | Short-term, low-dose anti-anxiety medication | Long-term use of high-dose anti-anxiety drugs |
The use of PIMs can have significant impacts on the health and well-being of our older loved ones, especially those in hospice care. Here are some key areas affected:
It’s important to note that the impact of PIMs can vary from person to person. Depending on their specific health conditions and care goals, what might be inappropriate for one individual could be necessary for another.
Here’s a breakdown of how PIMs can affect different aspects of geriatric health:
| Health Aspect | Potential Impact of PIMs | Why It Matters in Hospice Care |
|---|---|---|
| Physical Function | Reduced mobility, increased risk of falls | Can limit comfort and independence in final days |
| Cognitive Function | Confusion, memory problems, delirium | May interfere with the primary goal of comfort in hospice care |
| Emotional Well-being | Mood swings, increased anxiety or depression | It can impact quality of life and relationships with loved ones |
| Symptom Management | Inadequate pain control, increased side effects | May interfere with the primary goal of comfort in hospice care |
As caregivers and family members, it’s essential to:
Remember, hospice care aims to enhance comfort and quality of life. By being aware of PIMs and their potential impacts, we can work with healthcare providers to ensure our loved ones receive the most appropriate and compassionate care possible.
As we care for our elderly loved ones, especially those in hospice care, it’s crucial to be aware of the medications they’re taking. Some medications that are safe for younger adults can pose risks to older individuals. Let’s explore how to identify these Potentially Inappropriate Medications (PIMs) and understand the tools healthcare professionals use to make safe medication choices.
Several types of medications are more likely to be inappropriate for older adults. Here are some common classes of PIMs to be aware of:
Here’s a table summarizing these common PIMs and their potential risks:
| Medication Class | Examples | Potential Risks in Older Adults |
|---|---|---|
| Anticholinergics | Diphenhydramine, Oxybutynin | Confusion, Falls, Constipation |
| Benzodiazepines | Diazepam, Alprazolam | Falls, Cognitive Impairment |
| NSAIDs | Ibuprofen, Naproxen | Stomach Ulcers, Kidney Problems |
| Certain Diabetes Medications | Glyburide | Severe Low Blood Sugar |
| Some Antidepressants | Amitriptyline | Severe Side Effects, Falls |
The Beers Criteria is a valuable tool for healthcare professionals to identify PIMs in older adults. Named after Dr. Mark Beers, who created the first version in 1991, the American Geriatrics Society regularly updates this guide.
Key aspects of the Beers Criteria:
Here’s how the Beers Criteria can be used in practice:
Remember, the Beers Criteria is a guide, not a rule. Each patient’s situation is unique, and decisions should be made individually.
While the Beers Criteria is widely used in the United States, the STOPP/START Criteria offer another valuable approach prevalent in Europe. STOPP stands for “Screening Tool of Older Person’s Prescriptions,” and START stands for “Screening Tool to Alert doctors to Right Treatment.”
Key features of STOPP/START:
Here’s a comparison of the Beers Criteria and STOPP/START:
| Feature | Beers Criteria | STOPP/START Criteria |
|---|---|---|
| Origin | United States | Europe |
| Focus | Primarily on inappropriate medications | Both inappropriate and underused medications |
| Organization | By drug class and disease | By body system |
| Unique Strength | Detailed explanations and rationales | Includes potentially beneficial treatments |
How to Use This Information:
As caregivers or family members, you can:
Remember, while these criteria are invaluable tools, they don’t replace individualized medical judgment. Every person’s situation is unique, especially in hospice care. The goal is to find the right balance of medications that provides your loved one the most comfort and quality of life.
As we care for our elderly loved ones, especially those in hospice care, it’s crucial to understand the potential risks and consequences of Potentially Inappropriate Medications (PIMs). While medications are often necessary for managing symptoms and improving quality of life, some can pose significant risks to older adults. Let’s explore these risks in detail.
Adverse drug reactions (ADRs) are unwanted or harmful effects that occur when taking medications. In older adults, particularly those in hospice care, these reactions can be more frequent and severe due to:
Common types of adverse drug reactions in the elderly include:
Here’s a table summarizing some common PIMs and their potential adverse reactions:
| Medication Class | Examples | Potential Adverse Reactions |
|---|---|---|
| Anticholinergics | Diphenhydramine, Oxybutynin | Confusion, Dry mouth, Constipation, Blurred vision |
| Benzodiazepines | Diazepam, Alprazolam | Drowsiness, Falls, Cognitive impairment |
| NSAIDs | Ibuprofen, Naproxen | Stomach ulcers, Kidney problems, Increased blood pressure |
| Antipsychotics | Haloperidol, Risperidone | Parkinsonism, Increased risk of stroke in dementia patients |
Drug-drug interactions occur when one medication affects the activity of another when taken together. These interactions are particularly concerning in older adults because:
Types of drug-drug interactions include:
Here are some examples of common drug-drug interactions in the elderly:
| Drug Combination | Potential Interaction | Risk |
|---|---|---|
| Warfarin + NSAIDs | Increased bleeding risk | Severe bleeding |
| ACE inhibitors + Potassium supplements | Increased potassium levels | Dangerous heart rhythms |
| Calcium channel blockers + Certain antibiotics | Increased drug levels | Severe low blood pressure |
| SSRIs + NSAIDs | Increased bleeding risk | Gastrointestinal bleeding |
The use of PIMs in the elderly, particularly those in hospice care, can lead to severe consequences, including:
Research has shown that:
What Caregivers and Family Members Can Do:
Remember, while these risks are substantial, decisions about medication use should always be made in consultation with healthcare providers. In hospice care, the focus is on comfort and quality of life; sometimes, a medication’s benefits may outweigh its risks. The key is to have open, informed discussions to ensure the best care for your loved one.
When caring for loved ones in hospice or palliative care, medication management takes on a new dimension. The focus shifts from long-term health outcomes to comfort and quality of life, requiring a unique approach to medication use and balancing immediate needs with potential risks.
Medication needs differ significantly from standard medical care in hospice and palliative care. The primary goals are:
Common medication needs in end-of-life care include:
Here’s a table outlining some common symptoms and medication approaches in hospice care:
| Symptom | Common Medication Approaches | Special Considerations |
|---|---|---|
| Pain | Opioids, NSAIDs, and Adjuvant medications | It may require higher doses or alternative delivery methods (e.g., patches, pumps). |
| Breathlessness | Opioids, Benzodiazepines, Oxygen therapy | Focus on comfort rather than oxygen saturation levels. |
| Nausea/Vomiting | Antiemetics, Anticholinergics | May need to try multiple options to find the most effective. |
| Anxiety/Agitation | Benzodiazepines, Antipsychotics | Balance symptom relief with potential sedation. |
| Terminal Secretions | Anticholinergics | Focus on family comfort, as the patient may be unaware. |
In hospice care, the balance between symptom relief and medication safety requires careful consideration. Here are key points to remember:
Strategies for balancing symptom management and safety:
Deprescribing is the process of tapering or stopping medications that may no longer be beneficial or may be causing harm. In hospice and palliative care, deprescribing is crucial for several reasons:
The deprescribing process involves:
Here’s a guide to help identify medications that might be considered for deprescribing in hospice care:
| Medication Category | Examples | Considerations for Deprescribing |
|---|---|---|
| Preventive Medications | Statins, Aspirin for primary prevention | Limited benefit in limited life expectancy |
| Vitamins and Supplements | Multivitamins, Calcium supplements | Often unnecessary unless treating as specific deficiency |
| Chronic Disease Medications | Diabetes medications, Antihypertensives | May be reduced or stopped if not contributing to comfort |
| Cognitive Enhancers | Cholinesterase inhibitors | Limited benefits in advanced dementia, and may cause side effects |
Important Considerations for Caregivers and Family Members:
Remember, every patient’s journey is unique. What works best for one person may not be ideal for another. The key is maintaining an open dialogue with the hospice team, always keeping the patient’s comfort and wishes at the forefront of care decisions. Your role as a caregiver or family member is invaluable in this process, providing insights into the patient’s responses and preferences that guide medication management in this crucial time.
As we care for our loved ones in hospice or palliative care, it’s crucial to ensure they’re receiving the most appropriate medications. Reducing Potentially Inappropriate Medications (PIMs) can significantly improve comfort and quality of life. Let’s explore some practical strategies to achieve this goal.
A Comprehensive Geriatric Assessment (CGA) is a multidimensional, interdisciplinary diagnostic process designed to determine an older person’s medical, psychosocial, and functional capabilities and limitations. This assessment is precious in hospice care, providing a holistic view of the patient’s needs.
Key components of a CGA include:
Benefits of CGA in reducing PIM use:
| CGA Component | Relevance to PIM Reduction | Example |
|---|---|---|
| Medical Assessment | Identifies conditions that may be exacerbated by certain medications | Avoiding NSAIDs in a patient with a history of gastrointestinal bleeding |
| Cognitive Evaluation | Guides the choice of medications that won’t worsen cognitive function | Avoiding anticholinergics in a patient with dementia |
| Functional Assessment | Informs decisions about medications that may increase fall risk | Reconsidering benzodiazepines in a patient with poor mobility |
| Nutritional Assessment | It helps in choosing medications that won’t interfere with nutrition | Avoid medications that cause severe nausea in a patient with a poor appetite |
Medication reconciliation is creating the most accurate list of all medications a patient takes and comparing that list against the physician’s admission, transfer, and discharge orders. This process is crucial in hospice care to ensure medication safety and appropriateness.
Steps in medication reconciliation:
Importance of regular medication review:
Here’s a checklist for conducting a thorough medication review:
| Review Aspect | Questions to Consider |
|---|---|
| Indication | Is each medication still necessary? Does it align with care goals? |
| Effectiveness | Is the medication achieving its intended purpose? |
| Dosage | Is the current dose appropriate, considering age and organ function? |
| Side Effects | Are there any adverse effects impacting the quality of life? |
| Interactions | Are there potential drug-drug or drug-disease interactions? |
| Adherence | Are there any difficulties in taking the medication as prescribed? |
| Cost-Benefit | Does the benefit of the medication outweigh its cost and potential risks? |
Effective medication management in hospice care requires a team approach. Interdisciplinary collaboration ensures that all aspects of patient care are considered when making medication decisions.
Key team members and their roles:
Benefits of interdisciplinary collaboration:
Strategies for effective interdisciplinary collaboration:
For Caregivers and Family Members:
Your role in this interdisciplinary team is crucial. Here’s how you can contribute:
Remember, reducing PIM use in hospice care is a collaborative effort to enhance comfort and quality of life. By working together – healthcare professionals, caregivers, and family members – we can ensure that medication use is optimized to meet the unique needs of each individual in hospice care. Your involvement and insights are invaluable in this process, helping to create a medication plan that genuinely supports your loved one’s comfort and dignity in their final journey.
In hospice and palliative care, our primary goal is to ensure comfort and quality of life for our loved ones. While medications play a crucial role, alternative approaches and safer options often complement or sometimes replace potentially inappropriate medications (PIMs). Let’s explore how these alternatives can be tailored to individual needs.
Non-pharmacological interventions are treatments that don’t involve medications. These approaches can be highly effective in managing symptoms and improving quality of life, often with fewer side effects than medications.
Common non-pharmacological interventions include:
Here’s a table summarizing some non-pharmacological interventions and their potential benefits:
| Intervention | Potential Benefits | Considerations |
|---|---|---|
| Massage Therapy | Pain relief, Anxiety reduction, and improved sleep | Gentle touch may be preferable; avoid areas of skin breakdown |
| Music Therapy | Mood improvement, Pain distraction, Anxiety reduction | Choose familiar, preferred music; consider volume sensitivity |
| Aromatherapy | Nausea relief, Anxiety reduction, and improved sleep | Use caution with respiratory conditions; personal scent preferences vary |
| Positioning | Pain relief, Improved breathing, and pressure ulcer prevention | Regular position changes may be necessary; use pillows for support |
When medications are necessary, choosing age-appropriate alternatives to PIMs can help reduce risks while managing symptoms effectively. Here are some considerations for safer medication options:
Here’s a table comparing some common PIMs with safer alternatives:
| Condition | Potentially Inappropriate Medication | Safer Alternative |
|---|---|---|
| Insomnia | Long-acting benzodiazepines (e.g., diazepam) | Short-acting non-benzodiazepine (e.g., low-dose zolpidem) or melatonin |
| Chronic Pain | Long-term high-dose NSAIDs | Acetaminophen, topical analgesics, or low-dose opioids if necessary |
| Nausea | Promethazine (high anticholinergic burden) | Ondansetron or metoclopramide (with monitoring) |
| Anxiety | Long-term use of high-dose benzodiazepines | Short-term, low-dose anxiolytics or non-pharmacological approaches |
Every patient in hospice care has unique needs, preferences, and responses to treatments. Tailoring interventions to each individual is crucial for effective symptom management and improved quality of life.
Key considerations for personalized care:
Strategies for tailoring treatments:
Here’s a framework for tailoring treatments:
| Step | Action | Considerations |
|---|---|---|
| Assess | Evaluate symptoms, preferences, and current treatments | Use standardized assessment tools when possible |
| Plan | Develop a personalized treatment plan | Include both pharmacological and non-pharmacological approaches |
| Implement | Begin interventions, starting with safer options | Provide education to patients and families on new treatments |
| Evaluate | Regularly assess effectiveness and side effects | Be prepared to adjust the plan based on the response |
| Adjust | Modify treatments as needed | Involve the interdisciplinary team in decision-making |
For Caregivers and Family Members:
Your role in tailoring treatments is invaluable. Here’s how you can contribute:
Remember, tailoring treatments in hospice care aims to provide your loved one the most comfortable and dignified experience possible. By combining safer medication options with non-pharmacological interventions and personalizing the approach, we can often achieve better symptom management with fewer side effects. Your involvement and observations are crucial in this process, helping to ensure that care remains aligned with your loved one’s needs and wishes throughout their hospice journey.
In hospice care, educating patients and caregivers about medications is crucial for ensuring safe and effective treatment. This knowledge empowers everyone involved to make informed decisions and actively participate in the care process. Let’s explore the key aspects of this vital topic.
Medication literacy refers to the ability to understand and act on information about medications. In hospice care, this knowledge is vital for several reasons:
Key components of medication literacy include:
Here’s a table summarizing key medication information that patients and caregivers should understand:
| Medication Aspect | What to Know | Why It’s Important |
|---|---|---|
| Name and Purpose | Both brand and generic names; why the medication is prescribed | Prevents confusion; ensures understanding of treatment goals |
| Dosage and Timing | How much to take and when; what to do if a dose is missed | Ensures proper administration for effectiveness and safety |
| Side Effects | Common and severe side effects to watch for | Allows for early recognition and reporting of issues |
| Administration Method | How to take or give the medication (with food, water, etc.) | Ensures proper absorption and effectiveness |
| Storage | Proper storage conditions (temperature, light exposure, etc.) | Maintains medication effectiveness and safety |
Empowering patients to participate in medication-related decisions is a crucial aspect of person-centered hospice care. This involvement can lead to better outcomes and increased satisfaction with care.
Strategies for empowering patients:
Here’s a framework for shared decision-making about medications:
| Step | Action | Example |
|---|---|---|
| Introduce the decision | Clearly state that a decision needs to be made | “We need to decide on the best way to manage your pain.” |
| Present options | Describe available choices, including no treatment | “We could try a stronger pain medication, or we could explore non-drug options like massage.” |
| Discuss the pros and cons | Explain the potential benefits and risks of each option | “The medication might provide more relief, but it could make you drowsy. Massage has no side effects but might not be as effective.” |
| Explore preferences | Ask about the patient’s values and priorities | “What’s most important to you now – pain relief or staying alert?” |
| Facilitate decision | Help the patient make a choice based on their preferences | “Based on what you’ve said, it sounds like you’d prefer to try massage first. Is that correct?” |
In hospice care, it’s crucial to recognize and address cultural and linguistic differences that may affect medication understanding and use. These barriers can significantly impact patient care and outcomes if not properly managed.
Key considerations for addressing cultural and linguistic barriers:
Strategies for overcoming cultural and linguistic barriers:
Here’s a table outlining potential cultural considerations and strategies for addressing them:
| Cultural Consideration | Potential Impact | Strategies for Addressing |
|---|---|---|
| Language differences | Misunderstanding of medication instructions | Use professional interpreters; provide translated materials |
| Traditional healing practices | Reluctance to use prescribed medications | Discuss how to integrate traditional and Western approaches safely |
| Family-centered decision making | Patients may defer decisions to family members | Include family in discussions; respect family dynamics |
| Religious dietary restrictions | Refusal of medications containing certain ingredients | Explore alternative formulations; discuss with religious leaders if needed |
| Stigma around certain conditions or treatments | Reluctance to use or discuss certain medications | Provide private, culturally sensitive counseling; use neutral language |
For Caregivers and Family Members:
Your role in medication education and decision-making is crucial. Here are some ways you can contribute:
Remember, effective medication management in hospice care is a collaborative effort. By working together to overcome barriers and ensure clear understanding, we can provide the best possible care for your loved one. Your insights, cultural knowledge, and active participation are invaluable in this process, helping to ensure that medication use aligns with your loved one’s values, beliefs, and care goals throughout their hospice journey.
As we care for our geriatric hospice patients, it’s crucial to understand and implement effective strategies to reduce the use of potentially inappropriate medications (PIMs). This improves our patients’ quality of life and ensures their comfort and dignity during their final days.
Creating clear, comprehensive policies and guidelines is the foundation of any successful PIM reduction program. Here’s how healthcare institutions can approach this:
Remember, these policies should be living documents, regularly reviewed and updated to reflect the latest research and best practices in geriatric hospice care.
Technology can be a powerful ally in reducing PIM use in our digital age. Here’s how electronic health records (EHRs) and decision support systems can help:
By leveraging these technological tools, we can help healthcare providers make informed decisions and reduce the use of PIMs in our geriatric hospice patients.
To ensure the effectiveness of our PIM reduction programs, we need to establish clear quality indicators and monitoring processes. Here’s how we can approach this:
To help visualize and track these quality indicators, consider using a table like this:
| Quality Indicator | Baseline | Target | Current | Progress |
|---|---|---|---|---|
| % of patients on PIMs | 45% | 25% | 35% | ⬇️ 10% |
| Avg. number of PIMs per patient | 3.2 | 1.5 | 2.4 | ⬇️ 0.8 |
| % of patients with medication review in the last 30 days | 60% | 95% | 80% | ⬆️ 20% |
| Successful deprescribing rate | 30% | 70% | 55% | ⬆️ 25% |
By consistently measuring and monitoring these indicators, we can track our progress, identify areas for improvement, and ultimately provide better care for our geriatric hospice patients.
Implementing PIM reduction programs requires dedication, teamwork, and a commitment to continuous improvement. As hospice nurses, caregivers, and family members, your role in this process is invaluable. By working together to reduce PIMs, we can enhance the quality of life for our patients and ensure they receive the most appropriate and compassionate care during their final journey.
Remember, every medication review, every thoughtful prescription, and every careful monitoring of symptoms contributes to the comfort and dignity of our patients. Your efforts make a profound difference in their lives and the lives of their loved ones.
As we care for our geriatric hospice patients, we often face complex ethical dilemmas, particularly when it comes to medication management. These decisions can profoundly impact our patients’ quality of life and dignity during their final days. Let’s explore some of these ethical considerations with empathy and thoughtfulness.
One of the most challenging aspects of geriatric medication management is finding the right balance between respecting our patients’ autonomy and ensuring their safety. This delicate balance requires careful consideration and open communication.
Autonomy refers to an individual’s right to decide about their care. For our geriatric patients, this might include:
While we respect our patients’ autonomy, we also must ensure their safety. This might involve:
Strategies for Balancing Autonomy and Safety
Remember, there’s rarely a one-size-fits-all solution. Each patient’s situation is unique, and our approach should be tailored to their needs, values, and circumstances.
As our patients approach the end of life, decisions about medication management become even more crucial. The focus shifts from curative treatments to comfort care, but determining which medications to continue or discontinue can be challenging.
When making decisions about continuing or discontinuing medications, consider the following:
To help visualize the decision-making process, consider using a table like this:
| Medication Category | Continue? | Considerations |
|---|---|---|
| Pain Management | Yes | Adjust dosage as needed for comfort |
| Anti-anxiety/Sleep Aids | Yes | Monitor for effectiveness and side effects |
| Blood Pressure Medications | Maybe | Consider discontinuing if causing side effects |
| Cholesterol-lowering Drugs | No | Limited benefit in end-of-life care |
| Vitamins/Supplements | No | Unless providing specific symptom relief |
As we navigate these complex ethical considerations, we must remember that our primary goal is to provide compassionate, dignified care that aligns with our patients’ wishes and values. Every decision should be made with careful thought, open discussion, and a deep respect for the individual we care for.
These decisions can be emotionally challenging for hospice nurses, caregivers, and family members. It’s important to support each other through this process, seek guidance when needed, and remember that you’re doing your best to honor and care for your loved one or patient during this significant time in their life.
By approaching medication management with empathy, ethical consideration, and focusing on the patient’s well-being, we can ensure that our geriatric hospice patients receive the most appropriate and compassionate care possible during their final journey.
As we continue to care for our geriatric hospice patients, it’s essential to stay informed about emerging trends and innovations in medication management. These advancements hold the potential to significantly improve the quality of care we provide, making our patients’ final days more comfortable and dignified.
The field of geriatric pharmacotherapy is constantly evolving, with new research shedding light on the impact of PIMs and how to manage them better. Here are some key areas of emerging research:
As hospice caregivers, staying informed about this emerging research can help us make more informed decisions and provide better patient care.
Personalized medicine, also known as precision medicine, is an exciting frontier in healthcare that holds particular promise for geriatric patients. This approach tailors medical treatment to each patient’s characteristics.
Key aspects of personalized medicine in geriatric care:
Here’s a table that illustrates how personalized medicine might impact medication management for a hypothetical geriatric patient:
| Aspect | Traditional Approach | Personalized Medicine Approach |
|---|---|---|
| Pain Management | Standard opioid dosage | Dosage adjusted based on genetic metabolism factors |
| Antidepressant Selection | Trial and error | Guided by genetic markers of drug response |
| Anticoagulation Therapy | Standard protocol | Tailored based on genetic clotting factors |
| Alzheimer’s Treatment | Symptom-based approach | Guided by biomarkers of disease progression |
| Polypharmacy Management | General guidelines | Individualized based on a comprehensive assessment |
Artificial Intelligence (AI) is poised to revolutionize many aspects of healthcare, including medication management for geriatric patients. Here’s how AI could transform our approach to pharmacotherapy:
While these AI applications hold great promise, it’s important to remember that they are tools to augment, not replace, human judgment. The compassionate care hospice nurses, caregivers, and family members provide will always be at the heart of geriatric care.
As we look to the future of geriatric pharmacotherapy, it’s exciting to consider how these advancements might improve the care we provide. However, it’s equally important to approach these new technologies and approaches with a critical eye, always considering how they align with our patients’ needs, preferences, and values.
Stay informed about these developments for hospice nurses, caregivers, and family members, which can help you advocate for the best possible care for your patients or loved ones. Don’t hesitate to ask healthcare providers about new approaches or technologies that might benefit your patient.
Remember, while science and technology continue to advance, the core of hospice care remains unchanged: providing compassionate, dignified care that respects each patient’s individual needs and wishes. These new directions in geriatric pharmacotherapy are tools to help us achieve that goal more effectively, ensuring that our patients’ final days are as comfortable and meaningful as possible.
As we conclude our exploration of medication risks and management strategies for geriatric hospice patients, we must reflect on our efforts’ overarching goal: improving our patients’ quality of life during their final journey. Appropriate medication use is a cornerstone of this mission, balancing the need for symptom relief with the risks associated with polypharmacy and potentially inappropriate medications (PIMs).
For family members and caregivers, your role in medication management is invaluable. Here are some ways you can contribute to improving your loved one’s quality of life through appropriate medication use:
As we look to the future of geriatric pharmacotherapy, we see promising developments that could further enhance our ability to provide optimal medication management:
While these advancements hold great promise, the core principles of compassionate, patient-centered care will always remain at the heart of geriatric hospice care. The following table summarizes how we can combine current best practices with future innovations to improve medication management:
| Aspect of Care | Current Best Practice | Future Innovation |
|---|---|---|
| Medication Selection | Based on clinical guidelines and patient factors | Guided by pharmacogenomic testing |
| Dosing | Adjusted for age, weight, and organ function | Personalized based on genetic metabolism factors |
| Monitoring | Regular clinical assessments and lab tests | Continuous monitoring with wearable devices |
| Deprescribing | Based on clinical judgment and established protocols | Guided by AI prediction models |
| Patient Education | Verbal instructions and written materials | Interactive digital tools and personalized apps |
To the dedicated hospice nurses, compassionate caregivers, and loving family members, your commitment to improving the lives of geriatric hospice patients is truly admirable. Navigating the complex world of medication management can be challenging, but your efforts make a profound difference in the comfort and dignity of those in your care.
Remember that each patient’s journey is unique, and there’s no one-size-fits-all approach to medication management. By staying informed, remaining vigilant, and always keeping the patient’s wishes and quality of life at the forefront, you can help ensure that medications are a source of comfort rather than concern.
As we continue to learn and grow in our understanding of geriatric pharmacotherapy, let’s carry forward the fundamental principles that guide our care:
By adhering to these principles and embracing current best practices and future innovations, we can continue improving the quality of life for our geriatric hospice patients through appropriate medication use.
Thank you for being so dedicated to this vital aspect of end-of-life care. Your compassion, attention to detail, and willingness to advocate for your patients make a difference. Together, we can ensure that our patients’ final days are marked by comfort, dignity, and the highest quality of life possible.
Potentially inappropriate medication in palliative care patients according to STOPP-Frail criteria
Potentially inappropriate medication in older adults with palliative care at home
Importance of Medication Reconciliation in Hospice Care
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.