Category: Tips and Tricks
Articles about tips and tricks for caregivers and nurses caring for the terminally ill.
Articles about tips and tricks for caregivers and nurses caring for the terminally ill.

Caring for terminally ill patients in denial can be challenging. This article explores why understanding denial is crucial and offers strategies for compassionate care. Techniques like Naomi Feil's validation therapy and motivational interviewing are highlighted to support patients respectfully, maintaining their dignity and emotional well-being.
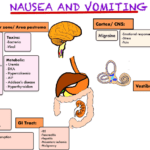
Nausea and vomiting are common and distressing symptoms in terminally ill patients. This comprehensive guide offers practical advice for caregivers and healthcare professionals on managing these symptoms, including pharmacological and non-pharmacological approaches, diet and lifestyle changes, and when to seek additional help.
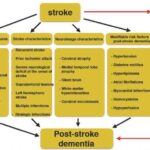
Stroke-induced dementia is a complex condition that affects both patients and their caregivers. In this guide, we’ll explore the impact of strokes on cognitive function, practical caregiving strategies, and considerations for maintaining quality of life.

Unveiling the pivotal events that may fast-track dementia progression. This article delves into how fractures, ulcers, infections, dietary habits, and certain medications like statins play a role in accelerating the onset and severity of dementia symptoms.

Living with dementia brings unpredictable days. This guide delves into the factors that influence the good and bad, offering insights and practical tips for caregivers to navigate the ever-changing landscape of dementia care, ensuring every day counts.

Discover critical approaches for hospice nurses and staff to identify and address factors leading to unnecessary discharges. This guide offers practical steps to maintain quality end-of-life care for terminal patients, fostering a stable care environment.

Discover the critical role of trauma-informed care in hospice. This guide provides nurses and staff with the knowledge to support traumatized patients while educating caregivers and family members on providing empathetic end-of-life care.

Discover the top twenty dermatologic conditions prevalent among the elderly. This guide covers symptoms, treatments, and tips for maintaining healthy skin in the golden years. It is perfect for caregivers and healthcare professionals.

Discover how acuity impacts hospice care. From assessment tools to real-world examples, this guide helps nurses and families navigate acuity levels.

Explore five essential strategies for maintaining hospice GIP compliance, including documentation best practices, staff preparedness, and emerging technological solutions. This guide helps hospice organizations navigate complex regulatory requirements while ensuring quality patient care.

This comprehensive guide provides essential insights into recognizing and addressing delirium in terminally ill individuals. It’s an invaluable resource for nurses, caregivers, and families, offering practical advice and empathetic support.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

This guide offers practical advice for caregivers handling the challenges of undiagnosed dementia. Learn to create a supportive environment, recognize early signs, and navigate healthcare options.

This article delves into the challenges faced by family caregivers in hospice and palliative care, offering practical strategies and resources to support them in their indispensable roles.

This article offers insight into the complexities of dementia’s progression, providing families and caregivers with the knowledge to differentiate between everyday fluctuations and actual advancements in stages.

This article delves into the transformative role of caregiver training in boosting Hospice CAHPS scores. Drawing on recent studies and expert insights, we explore practical strategies for enhancing caregiver education, ultimately leading to improved patient care and higher satisfaction ratings.

This comprehensive guide simplifies Medicare Hospice Benefits for caregivers and family members. Learn about eligibility, services, finding providers, and more. Empower yourself with the knowledge to make informed decisions about hospice care.

Discover how to manage wandering in dementia with practical strategies. Learn to create a safe environment and prevent risks effectively.

Creating a safe space for dementia patients involves innovative techniques like camouflage to prevent wandering. By disguising doors as walls or windows, caregivers can reduce elopement risk and ensure a secure, comforting environment. Learn how these methods can enhance safety and dignity.

Discover Bullosis Diabeticorum, a rare skin condition in people with diabetes causing painless blisters. Learn how to identify, treat, and care for loved ones with BD and a terminal illness.
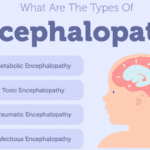
Caring for a loved one with terminal metabolic encephalopathy requires compassion and understanding. This guide provides insights into recognizing symptoms, adapting care strategies, and supporting the patient and caregiver through this challenging journey.

Understanding hospice recertification is crucial for ensuring your loved one receives the necessary care. Learn about the process, what to expect, and how to prepare.
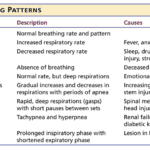
Understanding breathing patterns in end-of-life care is crucial for providing comfort to your loved one. Learn about regular vs. irregular breathing rhythms and when to contact hospice for additional support.
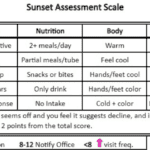
Discover how the Sunset Assessment Scale guides hospice nurses in determining visit frequencies, ensuring compassionate, patient-centered care during the final journey.