Category: Case Studies
Articles about two or more studies to explore a given topic.
Articles about two or more studies to explore a given topic.
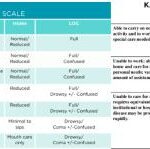
Explore the crucial roles of Karnofsky Performance Status (KPS) and Palliative Performance Score (PPS) in palliative and hospice care. This comprehensive guide helps nurses and caregivers understand these assessment tools, their applications, and critical differences, empowering them to provide more effective, patient-centered care.

Explore why side effects from medications can emerge after initial use and understand the critical need for vigilant monitoring and regular medication reconciliation to ensure patient safety and efficacy.

Discover how to use the CUS tool and Caring Feedback Model to advocate for your loved one's health. This guide empowers caregivers to communicate effectively with healthcare providers, ensuring their concerns are heard and addressed.

Explore comprehensive approaches to managing hallucinations in loved ones with dementia. This article covers pharmacological methods, focusing on Seroquel and non-drug strategies such as Naomi Feil's validation therapy. Learn how to validate feelings, de-escalate fear, and improve the quality of life for those experiencing cognitive impairment.
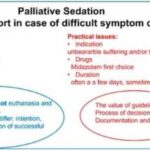
This guide covers the essentials of palliative sedation for hospice patients, including ethical dilemmas, timing, recommended medications, and monitoring effectiveness, ensuring comfort during the end-of-life journey.
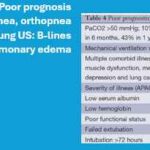
Dive into our in-depth analysis of CHF and COPD exacerbations. These critical events shape patient outcomes through expert insights and compelling case studies. Discover strategies for managing expectations and improving quality of life in the face of chronic illness.

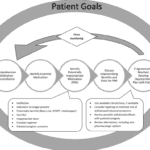
If you or someone you love is facing a terminal illness, you may feel overwhelmed by the physical, emotional, and spiritual challenges that come with it. You may wonder how to cope with the pain, the fear, the grief, and the loss of control. You may also want to find ways to make the most of the time you have left and to leave a lasting legacy for your loved ones.
Music therapy is a form of therapy that can help you and your family deal with these issues. It involves using music and musical activities to improve the health and well-being of people of all ages and backgrounds. Music therapy can help you express your feelings, communicate with others, relax your body and mind, cope with pain and stress, enhance your spiritual connection, and create a meaningful life story.

Welcome to our discussion on a topic close to many hearts: the care of our loved ones with dementia. When a family member is diagnosed with dementia, it feels like a part of them slowly fades away. But as they lose parts of themselves, your role in their life becomes even more crucial. This article isn’t just words on a page; it’s a beacon of hope and understanding, shining a light on why your voice, as a family member, is vital in the care of your loved one.

One of the tools doctors uses is called an FDG PET scan. It’s a special kind of test that takes pictures of the brain. FDG is a type of sugar, and PET stands for Positron Emission Tomography. When someone has a PET scan, they get a tiny amount of this sugar injected into their body. Because the brain uses sugar as fuel, the scan can show which parts are working well and which parts aren’t.
This is super helpful because in people with dementia, some parts of the brain don’t use sugar the same way healthy parts do. So, the scan can show doctors these changes and help them understand what’s going on.
In this article, we will discuss how to use the Beers Criteria to identify PIMs and potential prescribing omissions (PPOs) in hospice patients. PPOs are medications that are indicated but not prescribed for a specific patient or population, or that are prescribed at a suboptimal dose or duration. We will also present 10 case studies to illustrate the medication reconciliation and deprescribing process and the outcomes of medication changes in different scenarios.
If you are caring for a terminally ill patient in hospice, you know how challenging it can be to manage their medications. You want to make sure they are getting the best possible care, but you also want to avoid unnecessary or harmful drugs that may worsen their quality of life or cause adverse effects.
That’s where medication reconciliation and deprescribing come in. Medication reconciliation is the process of reviewing and updating the patient’s medication list to ensure accuracy and completeness. Deprescribing is the process of reducing or stopping medications that are no longer needed, effective, or appropriate for the patient’s condition and goals of care.

Losing a loved one to a terminal illness is an incredibly challenging experience. It's a journey filled with emotions, uncertainties, and the need for profound empathy. One crucial aspect of this journey is saying goodbye to your dying loved one and permitting them to pass peacefully. In this article, we'll explore the significance of these acts, which bring comfort to the terminally ill and aid in the grieving process for those left behind. We'll also share three case studies to illustrate the importance of these actions.

It is common for family members and caregivers who are not trained in end-of-life topics to be concerned about their loved one's oxygen concentration (SpO2 and sometimes also abbreviated SPaO2) reading from a pulse oximeter. Suppose their loved one refuses external oxygen or takes off the external oxygen. In that case, this often causes distress to the family and caregivers because they are focused on the numbers vs. the patients themselves. Hospice is about patient-centered care, and I would like to present four case studies to demonstrate how hospice manages this situation with compassion.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.

In the realm of hospice care, where empathy and compassion are paramount, a remarkable approach called Validation Therapy has emerged as a beacon of hope and comfort for individuals facing dementia and cognitive disorders in their final journey. As an experienced hospice registered nurse case manager, I've witnessed the transformative impact of Validation Therapy on patients, allowing them to find solace, regain their self-worth, and experience a sense of dignity during their end-of-life phase.

As a hospice RN case manager, I have seen many ethical dilemmas arise in end-of-life situations. Hospice care is unique because it focuses on providing comfort care to patients no longer seeking curative treatment for their illnesses. As a result, the ethical concerns in hospice care differ from those in other healthcare settings. This article will explore some ethical dilemmas that can arise in hospice care and how they can be addressed.
Before I review several case studies gathered from the sources in the resource section below, please allow me to share a current one of mine that is ongoing as this article is being published.

Dying is an inevitable facet of life, a natural progression that touches us all. This journey towards the end of life can unfold in diverse ways—peaceful and graceful or turbulent and fraught with stress. Amid this journey, there exists a phase known as the "rally." It occurs just before the final moments of a person's life. This rally phase often shrouds itself in misunderstanding and misconceptions. It's imperative to unravel what it truly signifies.
As nurses, when we see an acute change of condition, part of what we should be doing in our assessment is determining if there are reversible or treatable elements that are causing the change. In RN school, Dr. Dagen taught the students about using the D.O.G. mnemonic to help us remember that if a patient has an acute change of condition to check whether there were new medications the patient is taking, their O2 saturation level and their glucose level.
I would further add that as a hospice nurse dealing with mainly geriatric patients that if there is an altered level of consciousness (LOC)/personality change, to also consider the patient may have an infection. For any of you dealing with geriatric patients add “I” for infection, hence “D.O.G.I.” While this mnemonic is typically used for acute changes of level of consciousness, the thought process behind it can be used for other acute change of patient condition as well.
Falls among the elderly can have severe consequences, including hip fractures, which can be life-threatening. As an experienced hospice registered nurse case manager, I understand the importance of fall prevention, especially in private homes, personal care homes, and assisted living facilities. This article aims to provide practical tips for reducing falls in these settings by following the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it's readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor's orders, care plans, documentation, and education. We'll conclude with two real-life cases to illustrate these points.