Category: Palliative Care
Articles about palliative care including the differences between palliative care and hospice care which is palliative care at end-of-life.
Articles about palliative care including the differences between palliative care and hospice care which is palliative care at end-of-life.
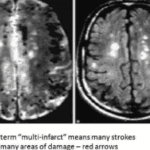
Multi-infarct dementia is a challenging condition that affects not only patients but also their families and caregivers. This comprehensive guide explores the disease's progression, common symptoms, and effective care strategies. Learn what to expect and how to provide the best support for your loved one from diagnosis through end-of-life care.

Posterior cortical atrophy (PCA), also known as Benson's syndrome, is a rare form of dementia affecting visual processing. This article explores PCA's symptoms, progression, and impact on daily life. Learn how to provide effective care, recognize when to seek help, and navigate the challenges of this complex condition.
Dementia is a challenging journey for both patients and caregivers. This comprehensive guide explores the stages of dementia progression and offers practical advice on care strategies, treatment options, and support resources. Learn how to navigate the changes and provide compassionate care throughout the journey.

This article delves into Utilization Behavior in dementia, offering practical advice for families and caregivers to create a safe environment and mitigate the challenges associated with this condition.
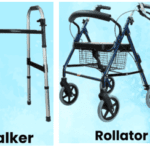
Discover practical and compassionate strategies for encouraging a loved one with dementia to use a cane, walker, or wheelchair. Enhance their safety and quality of life with these tips.
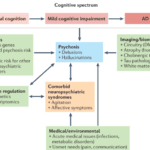
This guide provides hospice nurses, caregivers, and family members with essential information on dementia-induced psychosis, including its signs, symptoms, differentiation from other conditions, and effective management strategies.

This article provides practical tips and strategies for caregivers and family members to prevent dementia patients from removing their oxygen nasal cannula. Ensuring continuous oxygen use is essential for their health and well-being.
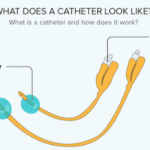
Discover how to provide expert care for a loved one with a Foley catheter. This comprehensive guide, written by a hospice nurse, covers essential steps, common problems, and medication tips. Learn to change tubing, prevent clogging, and ensure comfort during end-of-life care. Empower yourself with the knowledge to support your loved one effectively.

Learn about the diagnosis codes not allowed as primary diagnoses on hospice claims. This guide helps hospice agencies ensure accurate billing and optimal patient care.
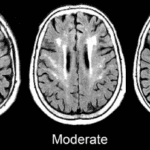
Caring for someone with Chronic Small Vessel Disease (CSVD) can be challenging, but with the proper knowledge and strategies, you can make a significant difference. This guide offers practical advice on creating a supportive environment, managing symptoms, and improving the quality of life for your loved one with CSVD.
Explore the powerful combination of hospice services and end-of-life doulas in providing holistic care for those facing terminal illness. Learn how these two approaches complement each other to support patients and families through the end-of-life journey.

Discover the essentials of hiring caregivers for terminally ill patients. This guide covers caregiver qualifications, assessing understanding of terminal care, and practical hiring tips.

This comprehensive guide explores blood work for common terminal diseases. Learn which lab tests are necessary for different conditions and how they assist in managing disease progression and treatment. Ideal for caregivers, nurses, and family members.

Navigating hospice coverage and payment in the USA can be complex. This article breaks down the key aspects of Medicare, Medicaid, and private insurance coverage for hospice care, helping you understand eligibility, benefits, and costs.
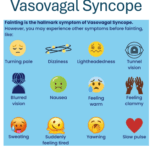
This article explores vasovagal syncope in terminally ill geriatric patients, especially those with cognitive impairments like dementia or brain cancer. It covers prevention, event handling, post-event care, and support for caregivers and family members.

Navigating the process of obtaining a dementia diagnosis for a loved one in denial involves understanding symptoms, preparing for doctor's visits, and participating in testing. This guide offers practical steps for family members to ensure proper treatment and care.

Recognizing when a loved one with dementia can no longer live safely alone is crucial for their well-being. This article helps families identify signs and offers practical steps for ensuring safety and care.

This guide helps hospice teams, caregivers, and families support loved ones with immunotherapy-induced tremors. Explore adaptive tools, tremor-reducing therapies, medication options, and practical care strategies to improve quality of life during hospice transitions.
This comprehensive guide provides valuable insights on how to report and prevent elderly abuse in nursing homes. It serves as a resource for families, guardians, and loved ones to understand their roles and responsibilities in advocating for the elderly. Learn how to empower yourself and ensure the safety and well-being of your loved ones.
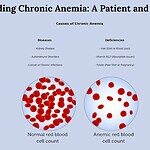
This guide explains chronic anemia in simple terms, covering symptoms, diagnosis, and treatments. Helps patients and families recognize signs and work with healthcare providers.
This article delves into the relationship between vertigo and dementia, offering insights for nurses, caregivers, and families to manage dizzy spells and provide compassionate care for those with cognitive challenges.

This article delves into the common medications that can lead to swelling in geriatric patients, with a focus on those receiving end-of-life care. It provides insights into prevention, management, and the importance of informed healthcare decisions.
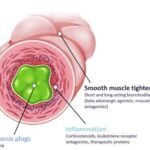
Understanding respiratory mucus plugs is crucial, especially for those navigating the challenges of caring for terminally ill patients. As an experienced hospice nurse, I recognize the significance of addressing respiratory issues with empathy and clarity. This article aims to provide valuable insights into respiratory mucus plugs, their causes, diagnosis, treatment, prevention, and practical techniques to enhance lung function.

Caring for a loved one with dementia can be challenging, especially when it comes to preventing falls. One innovative and inexpensive solution is using pool noodles as bed bumpers. This article provides a comprehensive guide on effectively utilizing pool noodles to create a safe and secure sleeping environment, reducing the risk of falls and injuries. From selecting the right noodles to proper installation techniques, we cover everything you need to know to ensure your loved one's safety and peace of mind.