Category: Advance Directives
Advance directives are legal documents that provide instructions for medical care and only go into effect if you cannot communicate your own wishes.
Advance directives are legal documents that provide instructions for medical care and only go into effect if you cannot communicate your own wishes.

Everyone 18 and older needs advance directives, but how do you choose between free forms, attorneys, or end-of-life doulas? We break down the costs, pros, and cons of each to help you ensure your medical wishes are honored.

As a nurse or doctor, you have the power to transform patient care through timely end-of-life conversations. This guide provides practical strategies to help you confidently discuss prognosis, encourage advance care planning, and introduce hospice care when appropriate—across hospitals, nursing facilities, and more.

A heartbreaking Facebook post reveals the devastating reality when families don't plan ahead for long-term care. Learn how Medicaid Asset Protection Trusts and working with life transition coaches years in advance can protect your home, savings, and dignity—and why the five-year lookback means you must act now.

After 15 years and 300 final breaths, nurse Laura M. discovered seven profound truths about what truly matters in life. Her patients didn't fear dying—they feared not having really lived. Learn these life-changing lessons and discover how life transition coaches can help you live with fewer regrets and ensure your wishes are honored.

A hospice nurse reflects on a powerful moment with a dying patient who painted "Three Wishes"—dandelions symbolizing childhood innocence and life's fleeting nature. This experience teaches us to examine how we're living, who we love, and what matters most. Learn why advance directives and living with fewer regrets matter for everyone.

A palliative care doctor shares people's three most common wishes at the end of life: mending relationships, expressing gratitude, and saying "I love you." Planning for a good death with the help of a life transition coach can help you accomplish more meaningful goals and ensure your final days reflect your values.

New research reveals that 37% of advanced cancer patients feel their treatment doesn't match their personal care goals—nearly twice the rate of other serious illnesses. This disconnect highlights our healthcare system's focus on fixing problems after they occur, without considering comfort or quality of life. Discover why planning your values and care preferences before illness strikes can prevent this misalignment and ensure you receive care that truly honors what matters most to you.

Facing difficult decisions about breathing support at the end of life? Understand the differences between BIPAP, intubation, and ventilators. Learn how complete advance directives guide families toward comfort-focused care and how end-of-life doulas provide affordable, compassionate support during these challenging choices.

Dialysis is a choice, not a requirement for end-stage kidney disease. While this life support treatment can extend life, it significantly impacts quality of life through fatigue, time constraints, and physical challenges. You have the right to choose comfort care and hospice instead. Learn why discussing dialysis preferences should be part of every living will and how end-of-life doulas can help navigate these important decisions.

Every year, thousands die in emergency departments unprepared for death. Sudden death in hospitals can be especially shocking for patients and families who haven't planned ahead. This guide highlights why preparation is important and describes how end-of-life doulas can assist.

If you're 18 or older without an advance directive, you're putting yourself and your loved ones at risk. This comprehensive guide explains why every adult—regardless of age—should prioritize creating a thorough living will reviewed every 3-6 months, and how end-of-life doulas can help.

When a family can't accept that their loved one is dying, it creates additional stress during an already challenging time. This article offers guidance on communicating with denial, supporting the patient, managing family dynamics, and finding professional help. Learn practical strategies to navigate this sensitive situation with compassion and understanding.
This comprehensive guide helps patients, families, and healthcare professionals confidently navigate POLST decisions. Learn the essential steps, understand your options, and ensure your end-of-life care wishes are honored through proper planning and communication.
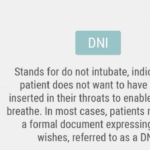
If you or your loved one has a severe illness, you may have heard about do not resuscitate (DNR) orders. This medical order tells the health care team what to do if the patient’s heart stops beating or they stop breathing. It is an incredibly crucial decision that can affect the quality and length of life. However, there are many myths and misunderstandings about DNR orders that can make it hard to choose what is best for you or your loved one. In this article, we will explain what DNR orders means and why it is important to understand it. We will also debunk the top ten myths about DNR orders and share the facts that can help you make an informed and respectful choice.

You may think that CPR is a miracle that can save anyone’s life, but that is not always the case. CPR is not practical for terminally ill patients, and it can cause more harm than good. In fact, studies show that only about 5% of terminally ill patients who receive CPR survive to leave the hospital. Many of them suffer from brain damage, broken ribs, or infections because of CPR.
This article aims to help you understand the truth about CPR for terminally ill patients. We will debunk ten common myths you may have heard or believed about CPR and provide you with accurate and reliable information. We will also help you make informed and respectful decisions about CPR for your loved one based on their wishes and values.
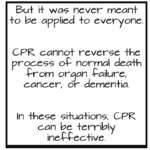
Choosing between full code and DNR for terminally ill patients can be challenging. This article explains the differences, benefits, and drawbacks of helping caregivers and families make informed decisions.
A review of the implications of each choice for the terminally ill patient as well as the loved ones of those who are terminally ill. This form comes into practice typically under two conditions… no pulse and is not breathing OR has a pulse and/or is breathing (but while not mentioned is typically in the last two weeks of life if no measures are taken with the understanding that any and all measures do not guarantee a longer time frame). Let’s review the form below:

Navigating conversations about Do Not Resuscitate (DNR) orders with terminally ill patients and their families can be challenging yet crucial for ensuring that the patient's wishes and comfort are prioritized. The decision between opting for DNR or full code often involves delicate emotions, medical considerations, and ethical concerns. In this article, we will delve into a methodology that has proven effective in facilitating these discussions, particularly in the context of hospice care. Drawing from years of experience and successful outcomes, we'll explore approaches that prioritize compassion, clarity, and patient-centered care. Additionally, we'll reference valuable resources to enhance understanding and guide these critical conversations.

Autonomy, the right to receive or refuse medical treatment is a crucial element of health care ethics (American Nurses Association (ANA), 2011; Plakovic, 2016). Nurses are involved in helping patients and families be aware of when end-of-life is occurring, and in educating the patient and family about end-of-life legislation that helps guide everyone committed to continue the right of patient autonomy when the patient is no longer able to express their wishes. Before the Patient Self Determination Act, we had the famous cases of Karen Ann Quinlan and Nancy Cruzan who were, from a point-of-view, forced to suffer for ten or more years of futile treatment (Miller, 2017). Now, we have advanced directives that allow patients to express their wishes while they are able, yet we still have ethical dilemmas when either those needs are expressed vaguely or not at all. It is in the best interest of the patient and the patient's loved ones for advanced directives to be utilized and kept up to date.