Breathing Support Decisions at End-of-Life: When Comfort Matters More Than Time
Published on October 6, 2025
Updated on October 19, 2025
Published on October 6, 2025
Updated on October 19, 2025
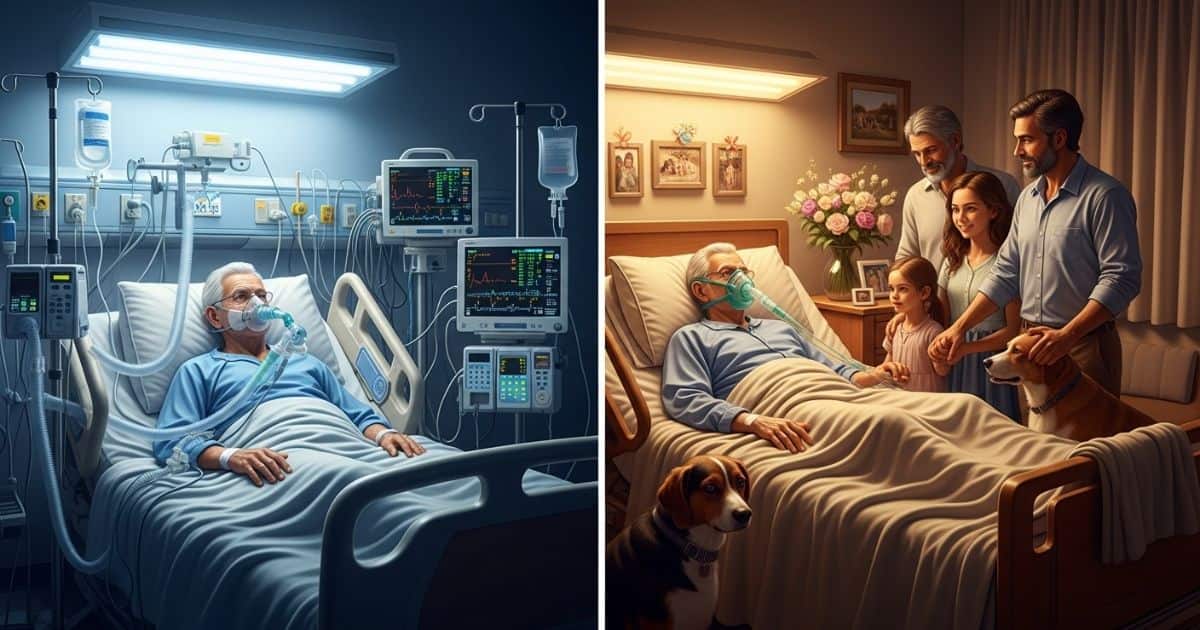
Table of Contents
When someone we love is facing the end of life, decisions about breathing support become deeply personal and emotionally challenging. Every breath becomes precious, and we find ourselves navigating complex medical choices that balance comfort, dignity, and our deepest values about what makes life meaningful.
These decisions don’t happen in isolation. We make them surrounded by family members, healthcare providers, and the weight of wanting to do what’s right for someone we care about deeply. Understanding our options helps transform fear into knowledge and gives us the tools to make choices that truly honor our loved one’s wishes.
BIPAP (Bilevel Positive Airway Pressure) represents a gentler approach to breathing support that works like having a helpful wind at your back. This machine delivers pressurized air through a tightly fitting mask, helping move air in and out of the lungs without requiring any tubes or invasive procedures.
Think of BIPAP as temporary assistance rather than life support. The person can still speak, eat, and interact with family members while receiving breathing help. Most importantly, BIPAP can be started or stopped at any time without complex medical procedures, giving families the flexibility to try this comfort measure and discontinue it if it doesn’t improve quality of life.
For many people with breathing difficulties, BIPAP provides meaningful relief from the work of breathing while allowing them to remain alert and present with their loved ones. This approach focuses on comfort and quality rather than simply extending time.
Intubation involves placing a breathing tube through the mouth or directly through the neck, connecting the person to a mechanical ventilator that breathes for them. This represents a significant medical intervention that fundamentally changes how someone experiences their final period of life.
Once intubated, the person cannot speak, eat, or interact normally with family members. They typically require sedation to tolerate the tube, and physical restraints may be necessary to prevent them from removing it. The focus shifts from comfort and connection to medical management and life extension.
Mechanical ventilation often leads to what healthcare providers call “prolonging the dying process” rather than extending meaningful life. While the heart continues beating and the machines keep the body functioning, the person may be unable to experience the peaceful closure that comes with natural death.
The fundamental difference between these approaches lies in their goals and reversibility. BIPAP aims to provide comfort and improve breathing ease while allowing natural disease progression. It can be used intermittently – perhaps during sleep or periods of increased breathing difficulty – without committing to long-term artificial support.
Intubation and mechanical ventilation, however, often begin a cascade of medical interventions that become increasingly difficult to withdraw. Once someone is placed on a ventilator, the decision to remove it becomes what families call “pulling the plug” – a traumatic choice that places the burden of ending life support on grieving loved ones.
Research shows that mechanical ventilation in end-of-life situations rarely leads to meaningful recovery. Instead, it frequently extends suffering, prevents natural death, and places families in the impossible position of deciding when enough medical intervention is enough.
Understanding these differences empowers families to make informed choices about breathing support that align with their values and goals for end-of-life care. When we focus on comfort rather than simply extending time, we often discover that gentler approaches like BIPAP provide the relief our loved ones need while preserving dignity and allowing for meaningful connections during their final journey.
When someone we love faces end-of-life decisions about breathing support, we often find ourselves at the heart of profound questions about what makes life meaningful. These decisions challenge us to examine our deepest values and consider what truly matters when time becomes precious.
Making values-based decisions means looking beyond medical procedures to focus on what brings dignity, comfort, and peace to someone’s final journey. This approach transforms difficult choices from overwhelming burdens into opportunities to honor someone we love.
Quality of life encompasses far more than just medical measurements or the ability to breathe independently. When we talk about quality in end-of-life care, we’re discussing the things that make someone feel like themselves: the ability to connect with loved ones, experience moments of peace, maintain dignity, and find meaning in their remaining time.
For some people, quality means being alert enough to recognize family members and share final conversations. For others, it’s about being comfortable and free from pain, even if that means sleeping more peacefully. Quality can mean staying at home surrounded by familiar sounds and smells or having spiritual practices honored during this sacred transition.
The key is understanding that quality isn’t a one-size-fits-all concept. What feels meaningful to one person might not matter to another. Some individuals value mental clarity above all else, while others prioritize physical comfort. Some want every moment possible with family, regardless of their condition, while others prefer a shorter but more comfortable experience.
The phrase “pulling the plug” often carries heavy emotional weight, making families feel like they’re abandoning someone they love. However, when families understand the reality of prolonged life support, this decision often transforms from something that feels like giving up into an act of profound love and respect.
When someone is on mechanical ventilation, they cannot speak, eat, or interact naturally with their loved ones. They typically require sedation to tolerate the tubes, and restraints may be necessary to prevent them from removing the equipment. Instead of extending meaningful life, these interventions often extend the dying process while preventing the peaceful closure that families and patients both need.
Families who choose to stop life support often discover they’re not “pulling the plug” on life – they’re removing barriers that prevent natural death from occurring with dignity. This choice allows focus to shift from medical procedures to what truly matters: being present, sharing love, and creating space for a peaceful goodbye.
Research consistently shows that comfort-focused care at the end of life doesn’t shorten survival time. Instead, it often allows people to feel better during their remaining days, leading to more meaningful connections with family and greater peace for everyone involved.
When families face decisions about breathing support, they often experience a complex mix of emotions that can feel overwhelming and confusing. Guilt frequently emerges – guilt about considering comfort care, guilt about wanting their loved one’s suffering to end, or guilt about feeling exhausted by the caregiving journey.
Fear plays a significant role, too. Families worry about making the wrong choice, about their loved one experiencing pain or distress, or about facing criticism from others who might not understand their decisions. Some family members fear that choosing comfort over life extension means they’re not fighting hard enough or loving deeply enough.
These emotions become even more complex when family members disagree about the best path forward. One person might push for every possible intervention while another advocates for comfort care. These disagreements often stem from different ways of expressing love and different beliefs about what honoring someone means.
The emotional burden intensifies when families must make these decisions under time pressure during medical crises. Without prior discussions about values and preferences, families find themselves trying to guess what their loved one would want while managing their own intense feelings about letting go.
Understanding that these emotional reactions are completely normal helps families navigate them with greater self-compassion. When families prepare for these decisions through advance care planning conversations, they can process emotions gradually rather than all at once during a crisis. This preparation transforms overwhelming choices into opportunities to honor their loved one’s values while supporting each other through grief.
Taking time now to discuss breathing support options, quality of life priorities, and end-of-life values creates a foundation that supports families when these decisions become necessary. These conversations don’t eliminate difficult emotions but provide clarity and confidence that help families focus on love and connection during their most challenging moments.
When someone you love faces breathing difficulties at the end of life, having a complete living will becomes a lifeline for your family. This legal document transforms from a piece of paper into your loved one’s voice when they can no longer speak for themselves, guiding every decision about BIPAP, ventilators, and other life-sustaining treatments.
A thorough living will eliminates the devastating burden of families guessing what someone would want during medical crises. Instead of facing impossible “pulling the plug” decisions under pressure, families can find peace knowing they’re honoring clearly expressed wishes.
Most people complete basic living will forms that cover general situations, but these generic documents often fail families when specific decisions arise. A simple checkbox for “life-sustaining treatments” doesn’t provide guidance about the crucial differences between BIPAP and mechanical ventilation.
Generic forms typically ask whether someone wants “artificial breathing support” without distinguishing between temporary comfort measures and long-term life extension. This vague language leaves families struggling to interpret what their loved one meant when facing specific choices like BIPAP for comfort versus intubation for prolonged support.
Real-life situations demand detailed guidance. When a family member develops breathing difficulties, medical teams need to know whether someone would want BIPAP to ease discomfort while remaining alert, or if they’d prefer natural death without any breathing assistance. Generic documents rarely address these nuanced preferences clearly.
Complete living wills explain personal values about the quality versus quantity of life. They specify what conditions would make life-sustaining treatments worthwhile and what circumstances would make comfort care more appropriate. This detailed guidance prevents families from making agonizing decisions based on guesswork during emotionally charged moments.
Effective advance directives go beyond basic forms to capture someone’s unique values, fears, and hopes for end-of-life care. They provide specific guidance for breathing support decisions while addressing the emotional and spiritual aspects of serious illness.
Complete documents explain personal definitions of quality of life and meaningful existence. They might specify that someone values mental clarity above physical comfort, or that maintaining connection with family matters more than extending time. This personalized guidance helps families make decisions that truly honor their loved one’s values.
Detailed directives address specific scenarios that commonly arise. They distinguish between accepting BIPAP for comfort during reversible illness versus declining mechanical ventilation for terminal conditions. They explain preferences for different stages of illness progression and clarify when shifting from curative to comfort care becomes appropriate.
The most effective advance directives include conversations with healthcare agents about real situations. Rather than simply naming someone to make decisions, complete planning involves discussing specific examples and helping agents understand the reasoning behind preferences. This preparation enables agents to make confident decisions that align with their loved ones’ values, even in unexpected situations.
Working with an end-of-life doula during advance care planning ensures nothing important gets overlooked. These professionals understand the complex decisions families face and help create comprehensive documents that address both medical preferences and emotional needs. Their expertise in navigating difficult conversations makes the planning process more thorough and less overwhelming than attempting to complete generic forms alone.
When families haven’t discussed specific end-of-life preferences, medical crises become breeding grounds for disagreement and guilt. One family member might push for every possible intervention while another advocates for comfort care, each believing they know what their loved one would want.
Complete advance planning eliminates this guesswork by providing clear guidance that reflects the person’s actual values rather than family members’ assumptions. When everyone understands someone’s documented wishes about breathing support, disagreements shift from arguing about unknown preferences to supporting clearly expressed choices.
Thorough planning also addresses the emotional burden that falls on healthcare agents. Without detailed guidance, agents often carry tremendous guilt about “pulling the plug” or feel uncertain about major decisions. Complete directives provide confidence that agents are following their loved one’s wishes rather than making independent choices about life and death.
Detailed documents prevent families from facing decisions during crisis moments. When someone experiences sudden breathing difficulties, having pre-established preferences about BIPAP versus mechanical ventilation allows medical teams to provide appropriate care immediately rather than forcing stressed family members to make urgent decisions without adequate information or emotional preparation.
The planning process itself strengthens family relationships by encouraging honest conversations about values and fears. Families who complete thorough advance directives together often discover a deeper understanding of each other’s perspectives and develop stronger communication skills for handling difficult situations. This foundation of trust and understanding supports families throughout the entire end-of-life journey, not just during medical decision-making moments.
Taking time now to create complete advance directives prevents crisis decision-making later and gives families the precious gift of confidence during their most challenging times.
Many families discover that working with an end-of-life doula creates a more thorough and meaningful advance care planning experience than they ever expected. End-of-life doulas bring unique expertise, personalized attention, and affordability that make comprehensive planning accessible to families who want more than generic forms can provide.
When families understand how end-of-life doulas approach advance care planning, they often realize this support offers exactly what they need to create living wills that truly work when difficult decisions arise. These professionals combine practical knowledge with compassionate guidance to help families navigate complex choices with confidence.
End-of-life doulas bring specialized knowledge to advance care planning that goes far beyond what generic legal forms can offer. We understand the real-world decisions families face because we work with people throughout their entire end-of-life journey, witnessing firsthand what happens when advance directives are clear versus when they’re vague.
Our experience with breathing support decisions makes us particularly valuable when families need to understand the differences between BIPAP, mechanical ventilation, and other life-sustaining treatments. While attorneys focus on legal requirements, end-of-life doulas help families understand what their choices actually mean in practice.
We excel at translating medical terminology into language families can understand and relate to their personal values. When someone says they don’t want to be “kept alive artificially,” we help them specify whether that includes BIPAP for comfort, feeding tubes for temporary support, or only long-term mechanical ventilation.
End-of-life doulas also understand family dynamics around difficult decisions in ways that legal professionals may not. We know how to facilitate conversations that prevent the “pulling the plug” burden from falling on unprepared family members during crisis moments.
Our training in advance care planning focuses on creating documents that actually work when families need them most. We help people think through specific scenarios rather than just checking boxes on forms, ensuring their directives provide clear guidance for real situations.
For families with straightforward advance care planning needs, end-of-life doulas offer a significantly more affordable option than working with attorneys, providing more personalized attention than generic online forms. Most uncomplicated advance directive planning falls well within our scope of practice and expertise.
Working with an end-of-life doula typically costs a fraction of legal fees while providing much more comprehensive support than filling out forms alone. We spend time understanding your values, walking through scenarios, and ensuring your documents reflect your actual wishes rather than just meeting legal requirements.
Our approach includes family education and discussion facilitation that attorneys rarely provide. We help families process the emotional aspects of advance care planning while ensuring everyone understands the practical implications of different choices.
End-of-life doulas also provide ongoing support that legal services typically don’t include. We can review and update advance directives as health conditions change, facilitate family conversations when conflicts arise, and provide guidance when medical situations require interpreting existing directives.
Cost-effectiveness becomes even more apparent when you consider that our advanced care planning often prevents expensive crisis decision-making later. Families with clear, comprehensive directives spend less on emergency interventions and have shorter hospital stays because everyone understands the patient’s actual wishes.
Certain situations particularly benefit from professional end-of-life doula guidance rather than attempting advance care planning alone. These circumstances often involve complex family dynamics, specific medical concerns, or when someone wants exceptionally thorough planning.
Families dealing with chronic illnesses like progressive neurological conditions, heart failure, or cancer benefit enormously from working with end-of-life doulas who understand how these conditions affect advance care planning decisions. We can help anticipate the specific choices these families may face and ensure their directives address relevant scenarios.
When family members disagree about end-of-life care approaches, professional facilitation prevents these discussions from becoming divisive conflicts. End-of-life doulas are trained to help families work through different perspectives while keeping the focus on the patient’s actual values and preferences.
Professional support becomes essential when someone has experienced traumatic medical situations or has strong feelings about specific interventions based on past experiences. We provide the emotional support and practical guidance needed to create advance directives that reflect wisdom gained from difficult experiences.
End-of-life doulas also excel when families want to explore less common options like home death, specific spiritual practices, or alternative approaches to end-of-life care. Our knowledge of available options helps families create comprehensive plans that honor unique preferences rather than defaulting to standard medical approaches.
The professional difference becomes most apparent when medical crises actually occur. Families who worked with end-of-life doulas to create their advance directives often report feeling much more confident during difficult moments because they know their documents truly reflect their loved one’s wishes rather than generic legal language.
Taking time to work with an end-of-life doula for advance care planning represents an investment in peace of mind that pays dividends when families need clear guidance most. This professional support transforms advance care planning from a legal requirement into a meaningful process that strengthens families and ensures wishes are truly honored.
Making decisions about breathing support and end-of-life care works best when families have time to think clearly and discuss options without pressure. Taking action now, before a medical crisis happens, gives families the gift of preparation and peace of mind that comes with knowing their wishes will be honored.
We often wait until we’re facing emergencies to think about advance directives or end-of-life support. Still, the most effective planning happens during calm moments when we can explore options thoughtfully. When families prepare ahead of time, difficult decisions become expressions of love rather than overwhelming burdens.
Many people completed basic advance directive forms years ago and haven’t looked at them since, but these documents need regular attention to remain useful when families need them most. Reviewing what you have now ensures your documents match your current values and medical realities.
Start by gathering all your current documents – living will, healthcare power of attorney, and any POLST or medical orders. Read through each document carefully, asking yourself if these choices still reflect what you want. Pay special attention to sections about breathing support, since these decisions directly affect the BIPAP and ventilator choices we’ve discussed.
Look for vague language that might not provide clear guidance during specific situations. Generic statements like “no artificial life support” don’t help families understand whether you’d want BIPAP for comfort versus mechanical ventilation for life extension. Complete advance directives address these nuances specifically.
Check whether your chosen healthcare agent still feels comfortable with this responsibility and understands your current wishes. Life changes – moves, divorces, deaths, or changing relationships – might mean you need to update who speaks for you when you cannot. Schedule a conversation with your agent to review your preferences about breathing support and other medical decisions.
Consider whether your documents address your current health situation. If you’ve developed chronic conditions like heart disease, COPD, or other illnesses that affect breathing, your advance directives should reflect the specific decisions you might face. This specificity helps families avoid the “pulling the plug” burden during medical crises.
When looking for an end-of-life doula to help with advance care planning, start by understanding what makes someone qualified to guide you through these critical decisions. The best doulas combine knowledge about medical options with skills in facilitating family conversations and creating comprehensive care plans.
Look for doulas who specialize in advance care planning rather than only providing support during active dying. These professionals understand the differences between BIPAP, mechanical ventilation, and other breathing support options, and can help you think through scenarios before they become urgent. They should be able to explain medical terms in language you understand while helping you connect choices to your personal values.
Ask potential doulas about their training and experience with advance care planning. While the field isn’t regulated, look for someone who has completed comprehensive training and can demonstrate knowledge about advance directives, medical decision-making, and family dynamics. The right doula will spend time learning about your specific situation and values rather than providing generic advice.
Consider whether you want someone who can work with your entire family, especially if you have adult children or others who might be involved in future care decisions. Effective end-of-life doulas help families process emotions, resolve conflicts, and reach decisions that everyone can support. This skill becomes especially important when families have different views about breathing support or other medical interventions.
You can find qualified end-of-life doulas through the resources available at Compassion Crossing’s End-of-Life Doula Resources section, which includes a “Find a Doula” directory to help connect you with professionals in your area. When you contact potential doulas, ask about their approach to advance care planning and whether they offer initial consultations to determine if you’re a good match.
Peace of mind comes from knowing that your wishes are clearly documented, your family understands your values, and you have support systems in place for whatever comes next. This preparation transforms potentially frightening medical decisions into opportunities to honor what matters most to you.
Start by having honest conversations with your family about your values and preferences for end-of-life care. Discuss what quality of life means to you, how you feel about different types of breathing support, and what you hope for during your final journey. These conversations help your loved ones understand the reasoning behind your choices, making it easier for them to advocate for your wishes if needed.
Create a comprehensive advance care plan that goes beyond basic legal documents. Work with an end-of-life doula or other qualified professional to develop detailed preferences about comfort care, spiritual support, and family involvement. Include specific guidance about BIPAP versus mechanical ventilation, so your family knows exactly what you’d want in different scenarios.
Make sure your documents are easily accessible and that multiple people know where to find them. Keep copies in several locations, give them to your healthcare providers, and ensure your family members have current versions. Consider creating a summary card for your wallet that outlines your basic preferences about emergency care and breathing support.
Review and update your plans regularly, especially after health changes, major life events, or when your priorities shift. What feels right at age 50 might feel different at age 70, and your advance directives should reflect your current values and medical realities. Schedule annual reviews with your family and healthcare agent to keep everyone informed about your wishes.
Taking these steps now prevents crisis decision-making later and ensures that your end-of-life journey reflects your values and preferences rather than medical default options. When families feel prepared and supported, they can focus on love, connection, and meaningful moments rather than struggling with overwhelming medical decisions during their most difficult times.
The peace that comes from thorough preparation extends far beyond the technical aspects of advance care planning. When you know your wishes are clearly documented and your family feels prepared to honor them, you create space for the deeper work of end-of-life transitions – saying goodbye, sharing love, and finding meaning in life’s final chapter.
Using Non-Invasive Ventilation at the End-of-Life
Ventilator Support and Oxygen Therapy in Palliative and End-of-Life Care in the Elderly
Understanding Breathing at End-of-Life: A Family Guide to Comfort Care
Crucial End-of-Life Conversations: A Compassionate Guide for End-of-Life Professionals
The Adult Priority You Can’t Afford to Skip: Your Complete Advance Directive
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series