A New Path Forward: Using the Frailty Trajectory Model to Navigate Healthcare Decisions
Published on October 22, 2025
Updated on December 19, 2025
Published on October 22, 2025
Updated on December 19, 2025
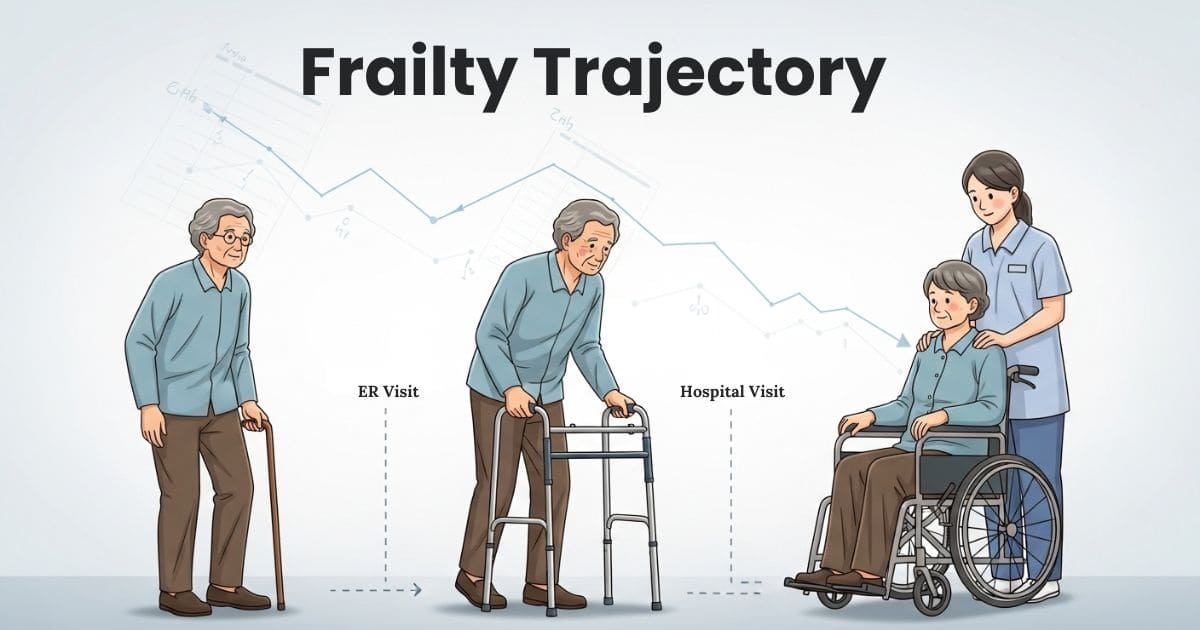
Table of Contents
Have you ever noticed how your parent or grandparent seemed to bounce back a little less after each hospital stay? Maybe they recovered from pneumonia, but suddenly needed a walker. Or they fell and broke a hip, and now they’re not quite themselves. These experiences aren’t random—they’re part of a pattern called frailty, and understanding this pattern can change how we approach healthcare decisions.
The Frailty Trajectory Model helps patients, families, and healthcare providers see the bigger picture. Instead of treating each health crisis separately, this model shows how they connect. Understanding these connections empowers everyone involved to make choices that honor what matters most.
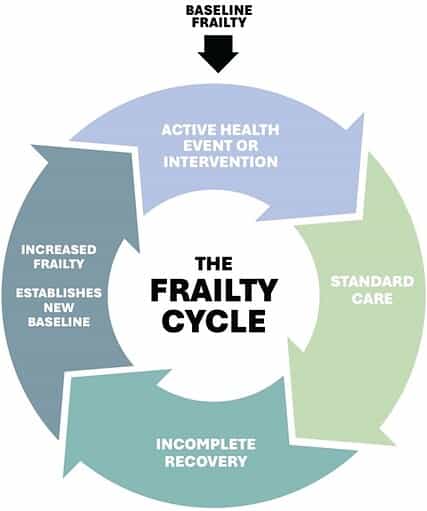
The Frailty Trajectory Model describes a pattern many older adults experience as they age. Think of it as a staircase going down, where each health event creates a new step. The model starts with baseline frailty—a person’s current level of vulnerability to health problems. When someone who is already frail experiences a health crisis or a medical procedure, they enter what’s called the frailty cycle.
This model is different because it recognizes that recovery often isn’t complete. After each event, a person might regain most of their strength and independence, but rarely all of them. This creates a pattern of stepwise decline, where each health crisis establishes a new, slightly lower baseline.
Research shows that frailty isn’t a straight line—it’s dynamic and can change in different directions. Some people’s frailty stays relatively stable for years. Others experience gradual increases that accelerate over time. Still others move between frail and less-frail states, though recovery becomes harder with each cycle.
The key insight is that vulnerability to future problems increases with each health event. A person who recovers from surgery at 70 might handle it well, but the same surgery at 75—after a few more health events—could lead to a significant decline. This isn’t failure; it’s a normal part of how our bodies’ reserve capacity diminishes over time.
For decades, healthcare has approached aging as either “healthy” or “sick.” You were either independent or you weren’t, and treatments either worked or they didn’t. This black-and-white view missed the gray zone where most older adults actually live.
The Frailty Trajectory Model offers a more accurate picture. It acknowledges that health exists on a spectrum and that spectrum shifts over time. This understanding helps healthcare providers and families make more realistic plans. Instead of expecting full recovery, they can plan for the most likely outcome and adjust care accordingly.
Perhaps the most crucial concept in this model is incomplete recovery. After each health crisis, most frail individuals don’t return to their previous baseline. They might improve from where they were in the hospital, but they don’t quite reach where they started.
Recognizing this pattern matters enormously for planning. If families understand that each hospitalization might mean their loved one needs more help afterward, they can prepare. They can arrange for additional support, modify the home environment, or reconsider treatment options with a high risk of decline.
Value-based care means making decisions that align with what matters most to the patient. The Frailty Trajectory Model provides a framework for these crucial conversations. When healthcare providers can show families the likely trajectory, everyone can discuss whether aggressive treatment fits with the patient’s goals.
For example, if an 85-year-old with moderate frailty faces major surgery, the model helps illustrate possible outcomes. Will surgery likely restore independence, or might it lead to nursing home placement? These aren’t easy questions, but the model makes them easier to explore honestly.
Knowledge reduces fear. Patients and families can make choices with open eyes when they understand the frailty cycle. They might decide aggressive treatment is worth the risks or choose comfort-focused care instead.
The model doesn’t prescribe what to choose—it simply clarifies what’s realistic. Some people want every intervention possible, regardless of the likelihood of full recovery. Others prefer quality of life over quantity, especially if each treatment means less independence. Both choices are valid when they reflect the patient’s values.
Early identification of frailty patterns allows for proactive planning. Instead of reacting to each crisis, healthcare teams can help patients and families think ahead. What supports might be needed in six months? Should advance directives be updated? Would palliative care services help manage symptoms and reduce hospital visits?
This forward-thinking approach reduces emergency decisions made in crisis moments. It gives families time to process, ask questions, and ensure care reflects the patient’s wishes.
Healthcare providers trained in frailty assessment can identify vulnerable patients before a crisis occurs. Simple screening tools can reveal who’s at risk for the frailty cycle. Early recognition means earlier conversations and better planning.
Practitioners can track changes over time, noting when someone’s baseline shifts. This ongoing monitoring helps predict future needs and adjust care plans accordingly.
Discussing frailty requires both honesty and gentleness. Healthcare providers must balance realism with hope, helping patients understand their situation without causing despair. The Frailty Trajectory Model provides a visual framework that clarifies these difficult conversations.
Effective practitioners listen to what patients value most—staying at home, avoiding pain, remaining independent, and spending time with family. They use this understanding to guide recommendations that fit the person, not just the disease.
No two people experience frailty identically. Some decline rapidly; others plateau for years. Personalized care plans account for individual patterns and preferences. They might include physical therapy to maintain strength, medication reviews to reduce harmful interactions, or palliative care to manage symptoms.
These plans evolve as the person’s trajectory becomes clearer. Regular reassessment ensures care stays aligned with current needs and goals.
Health and Life Navigation Specialists offer a unique perspective. Unlike medical providers who focus on disease, these professionals focus on the person’s entire life journey. They help clients navigate not just dying but living fully through decline.
These coaches understand that frailty affects more than physical health—it touches identity, relationships, and purpose. They provide emotional support while helping people maintain dignity and a sense of meaning.
The frailty trajectory is never completely predictable. Health and Life Navigation Specialists help people sit with this uncertainty without being paralyzed by it. They facilitate conversations about hopes and fears, helping families stay connected during difficult transitions.
Coaches also bridge the gap between medical appointments, providing continuity of support. They can help families understand and translate medical information into daily life decisions.
Health and Life Navigation Specialists excel at helping people identify what truly matters. They ask questions medical providers might not have time for: What makes life worth living? What would be unbearable? When would comfort become more important than cure?
These conversations prepare families for future medical decisions. When a crisis comes, they already know their loved one’s values, making difficult choices less agonizing.
The Frailty Trajectory Model gives families a shared language for discussing difficult topics. Instead of vague worry, they can point to specific patterns and plan accordingly. This clarity reduces conflict and helps everyone work toward common goals.
Family members often experience less guilt when they understand that decline is a natural pattern, not a personal failure. The model normalizes these changes, making them easier to accept and address.
Patients and families often choose less burdensome treatments when they understand the frailty trajectory. This doesn’t mean giving up—it means focusing on interventions most likely to improve quality of life. Studies show this approach can reduce unnecessary hospitalizations while maintaining or improving patient satisfaction.
Fewer emergency room visits mean more time at home, which most older adults prefer. It also reduces healthcare costs without sacrificing dignity or comfort.
Perhaps most importantly, using the Frailty Trajectory Model improves quality of life for patients and families. When care aligns with values, people report greater satisfaction. They feel heard, respected, and in control of their journey.
Physical frailty may progress, but proper support can improve psychological and social well-being. People live their remaining time more fully when they’re not constantly surprised by each decline.
Healthcare practitioners and Health and Life Navigation Specialists have an opportunity to transform how we approach aging and frailty. The first step is learning about the Frailty Trajectory Model and how to communicate it clearly. Training in frailty assessment tools provides the foundation for identifying at-risk patients early.
Next, routine frailty screening should be integrated into practice. Make it as standard as checking blood pressure. When identifying someone on the frailty trajectory, initiate compassionate conversations about the future. Use the model to illustrate patterns, not to predict doom, but to enable realistic planning.
Finally, connect patients and families with comprehensive support. This might include palliative care consultation, Health and Life Navigation Specialists, or community resources. Help them build a team that addresses physical, emotional, and spiritual needs.
By embracing the Fragile Trajectory Model, we can help people navigate aging with dignity, clarity, and peace. We can ensure that healthcare decisions reflect personal values, not just medical possibilities. This is the future of compassionate care—understanding the journey, supporting the person, and honoring what matters most.
Redefining Frailty: Planning Care Through the Frailty Trajectory Model
Frailty trajectories to identify end of life: a longitudinal population-based study
Holistic Nurse: Skills for Excellence book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying