Why Anticoagulants Should Be Reviewed Regularly for Deprescribing for Those Who Are Terminally Ill
Published on September 16, 2024
Updated on September 15, 2024
Published on September 16, 2024
Updated on September 15, 2024
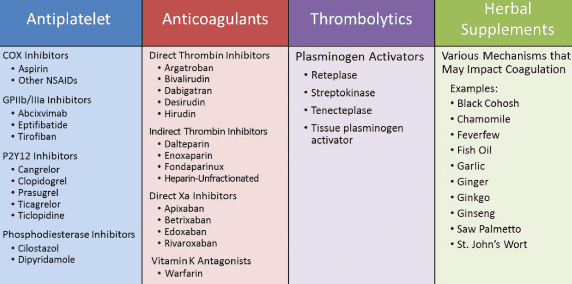
Table of Contents
If you are caring for someone who is terminally ill, you may have heard of anticoagulants. Anticoagulants are medicines that prevent blood clots from forming or growing. They are often prescribed to people who have conditions such as atrial fibrillation, deep vein thrombosis, pulmonary embolism, or heart valve problems. These conditions can increase the risk of stroke, heart attack, or other serious complications.
However, anticoagulants are not without risks or challenges. They can cause bleeding, which can be dangerous or even life-threatening. They can also interact with other medicines, foods, or supplements. They require regular blood tests and dose adjustments. They can be costly and inconvenient. They can affect the quality of life and comfort of the person taking them.
That is why it is important to review anticoagulants regularly and consider whether they are still needed or appropriate for the person who is terminally ill. This process is called deprescribing. Deprescribing means reducing or stopping medicines that are no longer beneficial or may cause harm. Deprescribing can help to avoid unnecessary side effects, simplify the medication regimen, reduce the burden of care, and focus on the person’s goals and preferences.
In this article, we will explain why anticoagulants should be reviewed regularly for deprescribing for those who are terminally ill. We will discuss the risks and benefits of anticoagulants in end-of-life care. We will outline the factors to consider when making decisions about anticoagulant deprescribing. We will suggest some strategies and resources to support anticoagulant deprescribing. We hope this article will help you make informed and compassionate choices about anticoagulant therapy for your loved one.
Anticoagulants can be helpful for some people who are terminally ill. They can prevent blood clots that can cause serious problems, such as stroke or heart attack. They can also reduce the symptoms and complications of some conditions, such as pain, swelling, or shortness of breath.
However, anticoagulants are not always effective or safe for terminally ill people. The evidence on the benefits and risks of anticoagulants in end-of-life care is limited and conflicting. Some studies have shown that anticoagulants can improve survival or quality of life for some patients with a life-limiting disease. Other studies have found no benefit or harm from anticoagulants in this population.
Anticoagulants can also cause many problems and challenges for people who are terminally ill and their caregivers. One of the most severe risks of anticoagulants is bleeding. Bleeding can occur in different body parts, such as the stomach, the brain, or the skin. Bleeding can be hard to stop and can lead to anemia, infection, or death. Bleeding can also affect the comfort and dignity of the person who is bleeding and the emotional well-being of the caregiver who is witnessing it.
Anticoagulants can also interact with other medicines, foods, or supplements that the person who is terminally ill may be taking. These interactions can increase or decrease the effect of anticoagulants, making them either too strong or too weak. This can increase the risk of bleeding or clotting. Therefore, anticoagulants require regular blood tests and dose adjustments to ensure they work properly. This can be stressful and inconvenient for the person who is terminally ill and the caregiver who has to arrange and attend the appointments.
The main risk of anticoagulants on hospice is internal bleeding caused by falls which are extremely common in the last few months of life. Often the internal bleeding is not caught timely, and this can result in dying faster than the terminally ill loved one or family anticipated.
Peter M. Abraham, BSN, RN — RN Case Manager
Anticoagulants can also be challenging to take or manage for people who are terminally ill and their caregivers. Anticoagulants come in different forms, such as pills, injections, or infusions. Some anticoagulants have to be taken at specific times or with specific foods. Some anticoagulants have to be stored or disposed of in a certain way. Some anticoagulants have to be monitored by a device or a nurse. These factors can make anticoagulants costly and complicated to use. They can also affect the adherence or compliance of the person taking them. Adherence means taking the medicine as prescribed. Poor adherence can reduce the effectiveness or safety of anticoagulants.
There is also a lot of uncertainty and variability in the clinical practice and guidelines regarding anticoagulant use in end-of-life care. Different doctors may have different opinions or recommendations about anticoagulants for terminally ill people. Different guidelines may have different criteria or evidence for anticoagulant use in this population. Countries or regions may have different policies or regulations for anticoagulant use in this setting. This can make it hard to know what is the best or most appropriate option for the terminally ill person.
Deciding whether to continue or stop anticoagulants for a terminally ill person is not easy. There is no one-size-fits-all answer. Each person’s situation is unique and may change over time. That is why it is crucial to make individualized and patient-centered decisions. This means considering the person’s medical condition, personal values, and wishes, as well as the best available evidence and expert advice.
There are several factors to consider when making decisions about anticoagulant deprescribing. Here are some of the key ones:
To illustrate how these factors can be applied in practice, let us look at some examples or case vignettes:
These cases show that anticoagulant deprescribing is not a one-time or a yes-or-no decision. It is a dynamic and ongoing process that requires regular review and reassessment. It also requires collaboration and communication among the person who is terminally ill, the caregiver, and the health care team. It is important to have honest and open discussions about the pros and cons of anticoagulants, the person’s values and preferences, and the available options and alternatives. By doing so, we can ensure that anticoagulant therapy is aligned with the person’s best interests and wishes.
You do not have to do anticoagulant deprescribing alone or without help. There are many ways to make anticoagulant deprescribing easier and safer for you and your loved one. Here are some tips and suggestions:
You can access reliable and relevant resources for more guidance and information on anticoagulant deprescribing. For example, you can check out the NHPCO Hospice Medication Deprescribing Toolkit, which provides practical tools and tips for hospice providers and caregivers to deprescribe medications, including anticoagulants, for patients who are terminally ill. You can also visit the Primary Health Tasmania guide to deprescribing anticoagulants, which offers a comprehensive and evidence-based approach to anticoagulant deprescribing for patients who are terminally ill. These resources can help you to make anticoagulant deprescribing more effective and appropriate for your loved one.
Anticoagulants are medicines that prevent blood clots. They can be helpful for some people who are terminally ill, but they can also cause problems and challenges for them and their caregivers. That is why anticoagulants should be reviewed regularly and carefully for deprescribing. Deprescribing means reducing or stopping medicines that are no longer beneficial or may cause harm. Deprescribing can help to avoid unnecessary side effects, simplify the medication regimen, reduce the burden of care, and focus on the person’s goals and preferences.
However, anticoagulant deprescribing is not a simple decision. It depends on many factors, such as the person’s medical condition, personal values, and wishes, as well as the best available evidence and expert advice. It also requires collaboration and communication among the terminally ill person, the caregiver, and the health care team. It also requires support and guidance from reliable and relevant resources and tools.
We hope this article has helped you understand why anticoagulant deprescribing is essential and how to do it safely and appropriately for your loved one. We also want to acknowledge that anticoagulant deprescribing is not a perfect or complete solution. There are still many limitations and gaps in the current evidence and practice. There is still a lot of uncertainty and variability in the outcomes and consequences of anticoagulant deprescribing. There is still a need for more research and education on anticoagulant deprescribing in end-of-life care. We encourage you to stay updated and informed on this topic and share your experiences and feedback with others. Together, we can make anticoagulant deprescribing more effective and compassionate for those who are terminally ill.
10 drugs to reconsider when a patient enrolls in hospice
Hospice Deprescribing and the Top Five Medications to Reevaluate
Inappropriate Medications in the Hospice Setting (geripal.org)
NHPCO_Deprescribing_Toolkit.pdf (PDF)
Primary Health Tasmania guide to deprescribing anticoagulants
Use of antithrombotics at the end of life: an in-depth chart review study
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series