Understanding the Importance of Quarterly Medication Reconciliation for Terminal Patients
Published on September 13, 2024
Updated on September 11, 2024
Published on September 13, 2024
Updated on September 11, 2024
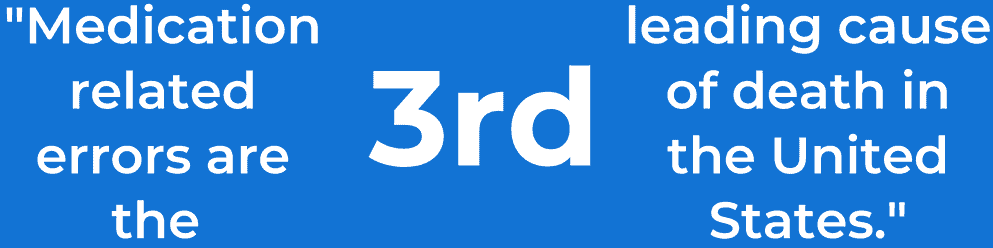
Table of Contents
If you are caring for a loved one who is terminally ill, you know how hard it is to keep track of all the medications they need to take. You may have multiple prescriptions, dosages, schedules, and side effects. You may also have to coordinate with doctors, nurses, pharmacists, and hospice workers. This can be overwhelming and stressful for both you and your loved one.
That is why it is important to reconcile medication. Medication reconciliation is checking and updating the list of medications your loved one is taking. It involves comparing the medications that your loved one takes with the medicines that their healthcare providers prescribe or recommend. It also involves making sure that the medications are safe, effective, and appropriate for your loved one’s condition and goals of care.
Medication reconciliation can help you and your loved one avoid many problems and complications that can arise from medication management. For example, it can prevent medication errors, such as taking the wrong drug, dose, or frequency. It can also prevent adverse drug events, such as allergic reactions, interactions, or overdoses. It can also prevent unnecessary treatments, such as continuing a medication that is no longer needed or beneficial.
In this article, we will explain why medication reconciliation is crucial for terminal patients and their families. We will also discuss the benefits, challenges, and solutions of regularly performing medication reconciliation. We will also discuss the need to reevaluate certain medications, such as donepezil and memantine, for patients with dementia as their disease progresses. We hope this article will help you and your loved one have a better and safer experience with medication management.
When your loved one is terminally ill, you want to make sure that they are comfortable and pain-free. You also want to respect their wishes and values. That is why it is important to review and update their medications every three months or more often if needed. This is called quarterly medication reconciliation.
Quarterly medication reconciliation can help you and your loved one achieve many benefits, such as:
Quarterly medication reconciliation is not something that you have to do alone. You can work with your loved one’s healthcare providers and other family members to make it easier and more effective. For example, you can:
Quarterly medication reconciliation is a valuable and helpful process for you and your loved one. It can help you improve your loved one’s safety, quality of life, and symptom management. It can also help you strengthen your relationship and trust with your loved one’s healthcare providers and other family members. By doing quarterly medication reconciliation, you can show your love and care for your loved one and make their final days more comfortable and meaningful.
While quarterly medication reconciliation can bring many benefits for you and your loved one, it can also pose many challenges and difficulties. You may encounter some obstacles and problems when you try to do medication reconciliation for your loved one who is terminally ill. Some of these challenges are:
These challenges can make medication reconciliation a complex and daunting task for you and your loved one. They can also affect the quality and safety of the medication management for your loved one. They can also cause you and your loved one to feel frustrated, stressed, or overwhelmed.
Besides these practical challenges, you may also face some emotional and ethical issues when you do medication reconciliation for your loved one who is terminally ill. Some of these issues are:
These issues can make medication reconciliation a challenging and painful process for you and your loved one. They can also affect the satisfaction and peace of mind of medication management for your loved one. They can also cause you and your loved one anxious, guilty, or sad.
Despite these challenges and issues, you can still do medication reconciliation for your loved one in a way that is effective and compassionate. You can overcome some of the obstacles and problems you may encounter and cope with some of the emotions and dilemmas you may face. Here are some strategies and solutions that can help you:
Quarterly medication reconciliation is not an easy or simple process for you and your loved one. It can involve many challenges and issues, making it hard and stressful. But it can also be a rewarding and meaningful process that can make it better and safer. Using some of the strategies and solutions we have suggested, you can do medication reconciliation for your loved one effectively and compassionately. You can also improve your relationship and trust with your loved one, their healthcare providers, and other family members. By doing quarterly medication reconciliation, you can show your love and care for your loved one and make their final days more comfortable and meaningful.
If your loved one has dementia, you may notice that their memory and thinking get worse over time. Dementia is a condition that affects the brain and causes problems with cognitive and functional abilities. Cognitive abilities are the mental skills that we use to learn, remember, and reason. Functional abilities are the physical skills used to do everyday activities, such as dressing, eating, and bathing.
As dementia progresses, your loved one’s cognitive and functional abilities decline. They may have more trouble remembering things, such as names, dates, or events. They may also have more difficulty understanding and expressing thoughts, such as following a conversation or finding the right words. They may also have more problems with planning and problem-solving, such as managing finances or making decisions.
As a result of these cognitive changes, your loved one’s functional abilities also deteriorate. They may need more help and supervision with daily tasks like cooking, cleaning, or taking medications. They may also lose interest or ability in hobbies, social activities, or work. They may also experience changes in their behavior, mood, and personality, such as becoming more agitated, depressed, or withdrawn.
Because of these changes, your loved one’s medication needs may also change. Some medications they take may not work as well as before or cause more side effects or interactions. Some medicines that they do not take may become more helpful or necessary. Therefore, it is essential to re-evaluate your loved one’s medications regularly, especially if they have dementia.
One type of medication that may need to be re-evaluated regularly for patients with dementia is donepezil and memantine. Donepezil (Aricept) and memantine (Namenda) are drugs that are used to treat the symptoms of Alzheimer’s disease, the most common cause of dementia. Donepezil belongs to a class of drugs called cholinesterase inhibitors, which increase a chemical in the brain called acetylcholine, which is involved in memory and learning. Memantine belongs to a class of drugs called NMDA receptor antagonists, which block a chemical in the brain called glutamate, which is involved in nerve cell communication.
Donepezil and memantine are not cures for Alzheimer’s disease, but they may help slow down the decline in cognitive and functional abilities. However, the effects of these drugs are not the same for everyone, and they may vary depending on the stage and severity of the disease. Therefore, it is essential to review the current evidence and guidelines for using donepezil and memantine for dementia, as well as their potential benefits and harms.
According to the National Institute for Health and Care Excellence (NICE), donepezil, galantamine, and rivastigmine (another cholinesterase inhibitor) are recommended to manage mild to moderate Alzheimer’s disease. Memantine is recommended as an option for managing moderate Alzheimer’s disease for people who cannot take cholinesterase inhibitors and for managing severe Alzheimer’s disease. However, these recommendations are based on the best available evidence, which is not very strong or consistent. Therefore, the decision to start, continue, or stop these drugs should be made individually, considering the person’s preferences, care goals, and clinical circumstances.
The evidence for the benefits and harms of donepezil and memantine for dementia is limited and mixed. Some studies have shown that these drugs can improve cognition, function, behavior, and global outcomes (such as overall health and quality of life) in some patients with dementia, compared with a placebo (a dummy pill) or best supportive care (without any drugs). However, these improvements are usually minor and may not be noticeable or meaningful for the person or their family. Other studies have shown that these drugs have no effect or even adverse effects on some outcomes in some patients with dementia. Moreover, these drugs can cause side effects, such as nausea, vomiting, diarrhea, headache, dizziness, confusion, or agitation. These side effects can be mild or severe and affect the person’s adherence, tolerance, and quality of life.
In the experience of the author, multiple hospice nurses, and hospice medical directors, these medications can cause significant harm to patients with dementia when they are in the last six months to a year of life. The severe side effects we often see in the field when these medications are not properly tapered off and discontinued include but are not limited to paranoia, delusions, agitation, violent physical outbursts, and anxiety, including severe, almost nonstop crying spells.
The consensus is to discontinue these medications (which may involve tapering — increasingly lower doses) under the guidance of a healthcare provider when the patient is in the last six to twelve months of life or otherwise determined to be in the terminal stage of the disease process.
This article discusses the importance of quarterly medication reconciliation for terminal patients and their families. We have explained what medication reconciliation is, and how it can help improve patient safety, quality of life, and symptom management. We have also explored the benefits, challenges, and solutions of doing medication reconciliation regularly. We have also talked about the need to re-evaluate certain medications, such as donepezil and memantine, for patients with dementia as their disease progresses.
Quarterly medication reconciliation is a valuable and helpful process for you and your loved one who is terminally ill. It can help you avoid many problems and complications from medication management. It can also help you make informed and respectful decisions about the medications that your loved one should take or stop taking. It can also help you strengthen your relationship and trust with your loved one’s healthcare providers and other family members.
However, quarterly medication reconciliation is not an easy or simple process. It can involve many challenges and issues, making it hard and stressful. It can also require a lot of communication, coordination, collaboration, and care from you and your loved one’s healthcare providers and other family members.
Therefore, we would like to offer you some practical tips and resources that can help you implement and improve medication reconciliation for your loved one. Some of these are:
We hope this article has helped you understand the importance of quarterly medication reconciliation for terminal patients and their families. We also hope it has inspired you to take action and improve your medication management for your loved one. We encourage you to talk to your loved one, their healthcare providers, and other family members about medication reconciliation and use the tips and resources that we have provided. Doing so can show your love and care for your loved one and make their final days more comfortable and meaningful.
The importance of medication reconciliation for patients and practitioners
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death