Comparing and Contrasting the Five Most Common Types of Dementia
Published on September 11, 2024
Updated on September 11, 2024
Published on September 11, 2024
Updated on September 11, 2024
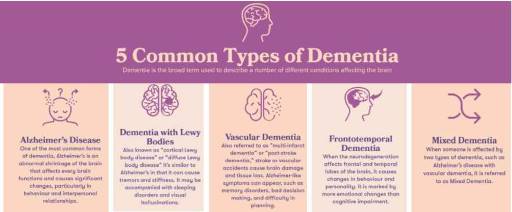
Table of Contents
If you have a loved one who has been diagnosed with dementia, you may feel confused, scared, or overwhelmed. You may wonder what dementia is, how it affects your loved one, and what you can do to help them. You are not alone. Millions of people around the world are living with dementia, and many more are caring for them.
Dementia is not a specific disease but a general term for a group of brain disorders that cause problems with thinking, memory, behavior, and daily activities. Dementia gets worse over time, and there is no cure for it. However, some treatments and strategies can help manage the symptoms and improve the quality of life for people with dementia and their caregivers.
There are many distinct types of dementia, each with its causes, features, and challenges. Some of the most common types are Alzheimer’s disease, Vascular dementia, Mixed dementia, Dementia with Lewy bodies, and Frontotemporal dementia. In this article, we will compare and contrast these five types of dementia and explain how they affect the brain, the body, and the person.
By learning more about the several types of dementia, you will be able to understand your loved one’s condition better and provide them with the best care and support possible. You will also be able to recognize the signs and symptoms of dementia and seek professional help when needed. You will also be able to find resources and tips that can help you cope with the challenges and stress of being a caregiver.
We hope this article will help you gain more knowledge and confidence in dealing with dementia and make you feel less alone and more hopeful. Remember, you and your loved one are not defined by dementia. You can still enjoy life and cherish the moments you have together.

Alzheimer’s disease is the most common type of dementia, affecting about 6 million people in the United States. It accounts for 60 to 80 percent of all dementia cases. Alzheimer’s disease is named after Dr. Alois Alzheimer, who first described the condition in 1906.
Alzheimer’s disease is a progressive brain disorder that causes problems with memory, thinking, and behavior. It usually starts with mild forgetfulness, such as misplaced keys or forgetting names. Over time, it affects more aspects of cognition, such as language, reasoning, judgment, and orientation. People with Alzheimer’s disease may also experience changes in personality, mood, and behavior, such as becoming more irritable, anxious, or depressed. They may also have trouble recognizing familiar people and places and performing daily tasks.
The damage and death of brain cells or neurons causes Alzheimer’s disease. This leads to the loss of connections between neurons and the shrinking of brain tissue, or atrophy. The exact cause of this process is not fully understood, but researchers have identified two main factors: amyloid plaques and tau tangles. Amyloid plaques are sticky deposits of protein fragments that build up between neurons and interfere with communication. Tau tangles are twisted fibers of another protein that accumulate inside neurons, impairing their function and structure.
The risk of developing Alzheimer’s disease increases with age, especially after 65. However, Alzheimer’s disease is not a normal part of aging and can affect younger people as well. Other risk factors include family history and genetics. Having a parent or sibling with Alzheimer’s disease increases the chance of developing it. Some genes, such as APOE-e4, are also associated with a higher risk of Alzheimer’s disease.
There is no single test for diagnosing Alzheimer’s disease. Doctors use a combination of methods, such as medical history, physical examination, cognitive tests, blood tests, and brain imaging, to rule out other plausible causes of dementia and assess the extent of brain damage. The diagnosis of Alzheimer’s disease is usually confirmed after death by examining the brain tissue for amyloid plaques and tau tangles.
There is no cure for Alzheimer’s disease, but there are treatments that can help manage the symptoms and slow down the progression. Some medications, such as cholinesterase inhibitors and memantine, can improve memory and cognition by enhancing the activity of certain brain chemicals. Other medications, such as antidepressants and antipsychotics, can help with mood and behavior problems. Cognitive stimulation, such as puzzles, games, and music, can help maintain mental function and well-being. Supportive care, such as home care, assisted living, or nursing home, can provide safety, comfort, and assistance for people with Alzheimer’s disease and their caregivers.
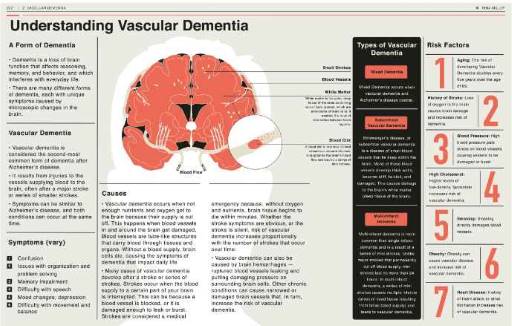
Vascular dementia is the second most common type of dementia, affecting about 1.5 million people in the United States. It accounts for 10 to 20 percent of all dementia cases. Vascular dementia is caused by a lack of blood flow to the brain, which deprives the brain cells of oxygen and nutrients and damages or kills them.
Vascular dementia can occur because of a stroke, a sudden interruption of blood flow to a part of the brain. It can also occur because of a series of small strokes or transient ischemic attacks, which may not cause noticeable symptoms but gradually damage the brain over time. Another cause of vascular dementia is atherosclerosis, the narrowing and hardening of the arteries due to the buildup of fatty deposits or plaques. This reduces the blood supply to the brain and increases the risk of stroke.
The key features of Vascular dementia depend on the location and extent of the brain damage. Some common symptoms include confusion, disorientation, trouble completing tasks, and vision problems. Other symptoms may include memory loss, language difficulties, mood changes, and physical weakness. The symptoms of Vascular dementia may vary in severity and progression, depending on the underlying cause and the individual’s health condition.
The risk factors for Vascular dementia are similar to those for stroke and heart disease. They include age, smoking, high blood pressure, high cholesterol, diabetes, obesity, and physical inactivity. Some of these risk factors can be modified by making lifestyle changes, such as quitting smoking, eating a healthy diet, exercising regularly, and managing stress. Other risk factors, such as family history and genetics, cannot be changed but monitored and treated if necessary.
The diagnosis of Vascular dementia is based on medical history, physical examination, cognitive tests, and brain imaging. Doctors will look for signs of stroke, atherosclerosis, or other vascular problems that may affect the brain. They will also assess the cognitive function and behavior of the person and compare them to the normal range for their age and education level. The diagnosis of Vascular dementia is usually confirmed by a brain scan, such as a CT or MRI, which can show the areas of the brain that are damaged or affected by reduced blood flow.
The treatment of Vascular dementia aims to prevent further damage to the brain and to improve the symptoms and quality of life of the person. Some medications, such as antiplatelets, anticoagulants, and statins, can help prevent or reduce the risk of stroke and atherosclerosis by improving blood flow and lowering cholesterol levels. Other medications, such as antidepressants, antipsychotics, and cholinesterase inhibitors, can help with mood and behavior problems and cognitive function. Surgery, such as carotid endarterectomy or angioplasty, may be performed to remove or widen the blocked or narrowed arteries and restore the blood supply to the brain. Lifestyle changes, such as diet, exercise, and stress management, can also help prevent or delay the progression of Vascular dementia and improve the overall health and well-being of the person. Rehabilitation, such as physical, occupational, and speech therapy, can help the person recover from the effects of stroke and regain some of their abilities and independence.
Mixed dementia is a type of dementia that involves two or more types of dementia occurring at the same time. The most common combination is Alzheimer’s disease and Vascular dementia, but other types of dementia, such as Dementia with Lewy bodies and Frontotemporal dementia, can also be involved. Mixed dementia affects about 1.2 million people in the United States and is more common in older adults.
Mixed dementia can be challenging to diagnose and treat because the symptoms and causes of the coexisting types of dementia may overlap or interact with each other. Some common symptoms of Mixed dementia include memory loss, confusion, disorientation, trouble completing tasks, vision problems, mood and behavior changes, and physical weakness. However, the symptoms of Mixed dementia may vary from person to person, depending on the types and severity of the dementia involved.
The risk factors for Mixed dementia are similar to those for the individual types of dementia. Age is the most significant risk factor, as the chances of developing Mixed dementia increase with older age. Having multiple causes of dementia, such as stroke, atherosclerosis, amyloid plaques, tau tangles, or genetic mutations, also increases the risk of Mixed dementia. Lifestyle changes can prevent or treat Some of these causes, such as quitting smoking, eating a healthy diet, exercising regularly, and managing stress. Other causes, such as family history and genetics, cannot be changed but can be monitored and treated if necessary.
The diagnosis of Mixed dementia is based on medical history, physical examination, cognitive tests, and brain imaging. Doctors will look for signs of the coexisting types of dementia and try to determine their relative contribution to the overall condition. The diagnosis of Mixed dementia is usually confirmed by a brain scan, such as a CT or MRI, which can show the areas of the brain that are damaged or affected by reduced blood flow, amyloid plaques, or tau tangles.
The treatment of Mixed dementia aims to address the symptoms and causes of the coexisting types of dementia and to improve the quality of life of the person and their caregivers. Some medications, such as cholinesterase inhibitors, memantine, antiplatelets, anticoagulants, statins, antidepressants, and antipsychotics, can help with memory, cognition, mood, behavior, and vascular health. Cognitive stimulation, such as puzzles, games, and music, can help maintain mental function and well-being. Supportive care, such as home care, assisted living, or nursing home, can provide safety, comfort, and assistance for people with Mixed dementia and their caregivers.
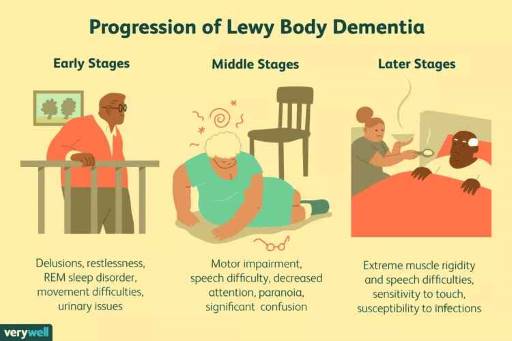
Dementia with Lewy bodies is a type of dementia that involves abnormal protein deposits in the brain. These deposits are called Lewy bodies, made of a protein called alpha-synuclein. Lewy bodies affect the brain cells that control thinking, memory, and movement. Dementia with Lewy bodies is the third most common type of dementia, affecting about 1.4 million people in the United States.
Dementia with Lewy bodies has some unique features that distinguish it from other types of dementia. One of these features is fluctuating cognition, which means that the person’s mental abilities can change from day to day or even hour to hour. The person may have periods of clarity followed by confusion, drowsiness, or disorientation. Another feature is visual hallucinations, which means that the person may see things that are not there, such as animals, people, or objects. The hallucinations may be vivid, colorful, realistic, and frequently occur. A third feature is REM sleep behavior disorder, which means people may act out their dreams while sleeping. The person may kick, punch, yell, or scream and may injure themselves or their bed partner. A fourth feature is movement disorders, which means the person may have symptoms similar to Parkinson’s disease, such as slow movement, rigid muscles, tremors, or shuffling walking. The person may also have problems with balance, coordination, and posture and may fall easily.
The risk factors for Dementia with Lewy bodies are not well understood, but some factors may increase the chance of developing it. Age is one of the risk factors, as Dementia with Lewy bodies usually affects people over 60 years old. Gender is another risk factor, as Dementia with Lewy bodies is more common in men than in women. Family history is a third risk factor, as having a relative with Dementia with Lewy bodies or Parkinson’s disease may increase the risk of Dementia with Lewy bodies. However, most cases of Dementia with Lewy bodies are not inherited, and the role of genetics is still unclear.
The diagnosis of Dementia with Lewy bodies is based on medical history, physical examination, cognitive tests, and brain imaging. Doctors will look for the presence of the four key features of Dementia with Lewy bodies and try to rule out other plausible causes of dementia, such as Alzheimer’s disease, Vascular dementia, or medication side effects. The diagnosis of Dementia with Lewy bodies is usually confirmed by a brain scan, such as a PET or SPECT, which can show the activity and function of the brain cells. However, the only definitive way to diagnose Dementia with Lewy bodies is by examining the brain tissue after death and finding the Lewy bodies in the brain.
Treating Dementia with Lewy bodies aims to improve the symptoms and quality of life of the person and their caregivers. Some medications, such as cholinesterase inhibitors, can help with cognition, hallucinations, and behavior. Other medications, such as levodopa, can help with movement problems. However, some medications, such as antipsychotics, can worsen the symptoms of Dementia with Lewy bodies and should be used with caution. Behavioral therapy, such as music, art, or pet therapy, can also help with mood, well-being, and communication. Palliative care, such as pain management, comfort care, and hospice, can provide support and relief for the person and their caregivers in the advanced stages of Dementia with Lewy bodies.

Frontotemporal dementia (FTD) is a type of dementia that affects the front and temporal lobes of the brain—these parts of the brain control personality, behavior, and language. FTD is different from other types of dementia, such as Alzheimer’s disease or Vascular dementia, because it usually starts at a younger age and affects various aspects of cognition. FTD is the fourth most common type of dementia, affecting about 0.6 million people in the United States.
FTD is caused by the damage and loss of brain cells, or neurons, in the front and temporal lobes. This leads to the shrinking of these lobes, known as atrophy. The exact cause of this process is not fully understood, but researchers have found that some people with FTD have abnormal proteins in their brain cells, such as tau or TDP-43. These proteins may interfere with the function and structure of the neurons and cause them to die.
The key features of FTD depend on which part of the front and temporal lobes is affected. Some common symptoms of FTD include:
The risk factors for FTD are not well known, but some factors may increase the chance of developing it. Age is one of the risk factors, as FTD usually affects people between the ages of 45 and 65, although it can occur earlier or later. Genetics is another risk factor, as some cases of FTD are inherited and linked to mutations in certain genes, such as C9orf72, MAPT, or GRN. Environmental factors, such as head injury, infection, or exposure to toxins, may also play a role in FTD, but more research is needed to confirm this.
The diagnosis of FTD is based on medical history, physical examination, cognitive tests, and brain imaging. Doctors will look for the presence of FTD symptoms and try to rule out other plausible causes of dementia, such as Alzheimer’s disease, vascular dementia, or psychiatric disorders. The diagnosis of FTD is usually confirmed by a brain scan, such as a CT or MRI, which can show the atrophy of the front and temporal lobes.
There is no cure for FTD, but there are treatments that can help manage the symptoms and improve the quality of life of the person and their caregivers. Some medications, such as antidepressants, antipsychotics, or mood stabilizers, can help with behavior and mood problems. Other medications, such as cholinesterase inhibitors or memantine, may help with cognition, but their effectiveness is not well established. Speech therapy can help with language problems and teach the person and their caregivers how to communicate better. Social support, such as counseling, education, or support groups, can provide emotional and practical assistance for the person and their caregivers.
| Dementia Disease Name | Short Description | Percentage Prevalence | Common Symptoms | Staging | Similarities |
|---|---|---|---|---|---|
| Alzheimer’s disease | A type of dementia caused by abnormal buildups of proteins in the brain | 60-80% of all cases of dementia | Memory loss, difficulty with language, numbers, or reasoning, mood swings, personality changes, hallucinations, delusions, or paranoia | Mild, moderate, or severe Uses FAST Scale (stages 1-3 early/mild, 4-5 middle/moderate, 6 late, 7 terminal/severe) | Similar to other types of dementia in causing memory loss and cognitive decline, but different in the cause, the pattern, and the treatment of the disease |
| Vascular dementia | A type of dementia caused by reduced blood flow to the brain | 10-20% of all cases of dementia | Memory loss, difficulty with language, numbers, or reasoning, trouble with planning, organizing, or following instructions, mood changes, personality changes, slowed thinking or movement | Multi-infarct dementia, subcortical vascular dementia, post-stroke dementia, or mixed dementia | Similar to other types of dementia in causing memory loss and cognitive decline, but different in the cause, the pattern, and the treatment of the disease |
| Mixed dementia | A condition where more than one type of dementia occurs simultaneously | Up to 45% of people with dementia | Memory loss, fluctuations in alertness, attention, or cognition, visual hallucinations, parkinsonism, sleep problems, autonomic dysfunction | Depends on the combination and severity of the types of dementia | Similar to other types of dementia in causing memory loss and cognitive decline, but different in the complexity and unpredictability of the symptoms and the progression of the disease |
| Dementia with Lewy bodies | A type of dementia that involves abnormal deposits of a protein called alpha-synuclein in the brain | 5-10% of all cases of dementia | Memory loss, fluctuations in alertness, attention, or cognition, visual hallucinations, parkinsonism, sleep problems, autonomic dysfunction | Mild, moderate, or severe | Similar to other types of dementia in causing memory loss and cognitive decline, but different in the cause, the pattern, and the treatment of the disease |
| Frontotemporal dementia | A type of dementia that affects the frontal and temporal lobes of the brain | 2-5% of all cases of dementia | Loss of interest or motivation, lack of empathy or awareness, impulsive or inappropriate actions, poor judgment or planning, difficulty finding words or understanding speech, repeating words or phrases, changes in mood or personality, withdrawal from social activities, eating too much or too little, having trouble with movement or balance | Behavioral variant FTD, semantic variant primary progressive aphasia, nonfluent variant primary progressive aphasia, corticobasal syndrome, or progressive supranuclear palsy | Similar to other types of dementia in causing memory loss and cognitive decline, but different in the cause, the pattern, and the treatment of the disease |
If you are caring for a loved one with dementia, you may have heard of hospice care, but you may not know what it is or when it is appropriate. Hospice care is a special type that focuses on providing comfort and support to people with life-limiting illnesses and their families. It does not aim to cure the disease but to ease the symptoms and improve the quality of life in the final stages.
Hospice care can benefit people with dementia and their families in many ways. It can help manage the pain, agitation, and distress common in advanced dementia. Hospice care can also provide emotional and spiritual support to the person with dementia and their loved ones and practical assistance with daily tasks and caregiving. Depending on the patient’s and family’s needs and preferences, hospice care can be provided at home, in a hospice facility, or in a nursing home.
Hospice care is available to people with a life expectancy of six months or less, as determined by a physician. However, this does not mean hospice care will end after six months. Hospice care can continue if the person meets the eligibility criteria and the family wishes to receive it. For people with dementia, the eligibility criteria may include experiencing multiple physical and mental declines, such as losing weight, having difficulty swallowing, being bedridden, or having severe cognitive impairment. Hospice care may also be appropriate for people with dementia who require frequent nursing care or who have recurrent infections that are hard to treat or prevent.
Dementia is a progressive disease that affects the brain and causes memory loss, confusion, and behavioral changes. There are different types and stages of dementia, but one of the most common and severe forms is Alzheimer’s disease. Alzheimer’s disease can be measured by the FAST Scale, which stands for Functional Assessment Staging. The FAST Scale has seven stages, from 1 to 7, that describe the functional decline of people with Alzheimer’s disease. Stage 7 is the most advanced, indicating that the person may benefit from hospice care.
Some of the signs and symptoms that are typical of stage 7 on the FAST Scale are:
Another sign that hospice care may be appropriate for someone with dementia is severe cognitive impairment. This means that the person has no awareness of self, environment, or time and cannot recognize familiar people or objects. The person may not respond to their name, not know where they are or what day it is, and may not remember their spouse, children, or friends. The person may also hallucinate, have delusions or paranoia, and may become agitated or aggressive.
Other signs and symptoms that indicate hospice care may be appropriate for someone with dementia are recurrent infections and difficulty swallowing, eating, or drinking. Recurrent infections, such as pneumonia, urinary tract infections, or sepsis, are common in people with advanced dementia, and they can be life-threatening or cause complications. Difficulty swallowing, eating, or drinking can lead to weight loss, dehydration, or malnutrition and can also increase the risk of choking or aspiration. These conditions can affect the person’s comfort and well-being and may require hospice care to manage them.
Pain, agitation, or distress are also signs and symptoms that indicate hospice care may be appropriate for someone with dementia. Pain can be caused by various factors, such as infections, injuries, pressure ulcers, or arthritis, and it can be hard to detect or measure in people with dementia, who may not be able to express or report it. Agitation or distress can be caused by cognitive impairment, environmental factors, or unmet needs, and they can manifest as restlessness, anxiety, anger, or depression. Pain, agitation, or distress can affect the person’s quality of life and comfort and may require hospice care to relieve them with medication or other interventions.
Hospice care can make a difference for people with dementia and their families in the final stages of the disease. Hospice care can help improve the person’s comfort and dignity and reduce their suffering and stress. Hospice care can also help the family cope with the emotional and practical challenges of caring for a loved one with dementia and provide them with guidance and support. Hospice care can help the family prepare for the end of life and the grief process and offer them bereavement services after the death of their loved one.
If you think that hospice care may be right for your loved one with dementia, you should talk to your physician and hospice team about your options and preferences. They can help you determine the eligibility and availability of hospice care and explain the benefits and services that hospice care can provide. They can also help you find and select a hospice provider that meets your needs and expectations.
There are many resources and contact information that you can use to learn more about hospice care and find a hospice provider near you. Some of them are:
Hospice care can be a valuable option for your loved one with dementia and your family. Hospice care can help you make the most of the time you have left with your loved one and provide you with comfort and support. Hospice care can help you honor your loved one’s wishes and values and celebrate their life and legacy. Hospice care can help you say goodbye to your loved one with peace and grace.
In this article, we have compared and contrasted the five most common types of dementia: Alzheimer’s disease, vascular dementia, Mixed dementia, Dementia with Lewy bodies, and Frontotemporal dementia. We have explained how they affect the brain, body, and person, as well as their key features, causes, and risk factors. We have also discussed the diagnosis and treatment options for each type of dementia and how they can help improve the symptoms and quality of life of the person and their caregivers.
We hope this article has helped you better understand the several types of dementia and how they can affect your loved one. We also hope that it has given you some helpful information and tips on how to care for and support your loved one and yourself as you face the challenges and stress of dementia.
We know that dementia can be a complicated and overwhelming condition, but you are not alone. Some resources and services can help you cope and find support. Some of these resources include:
You can also find local support groups, organizations, and agencies that can provide you with emotional, practical, and financial assistance. You can ask your doctor, social worker, or local aging agency for referrals or search online for resources in your area.
Remember, you and your loved one are not defined by dementia. You can still enjoy life and cherish the moments you have together. You can also find hope and strength in the knowledge that many people care about you and that researchers are working hard to find better treatments and cures for dementia. You are not alone, and you are not hopeless. You are brave, and you are loved.
Understanding Different Types of Dementia
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?