Understanding PACE: A Complete Guide to All-Inclusive Care That Keeps Seniors Home
Published on November 12, 2025
Updated on November 12, 2025
Published on November 12, 2025
Updated on November 12, 2025
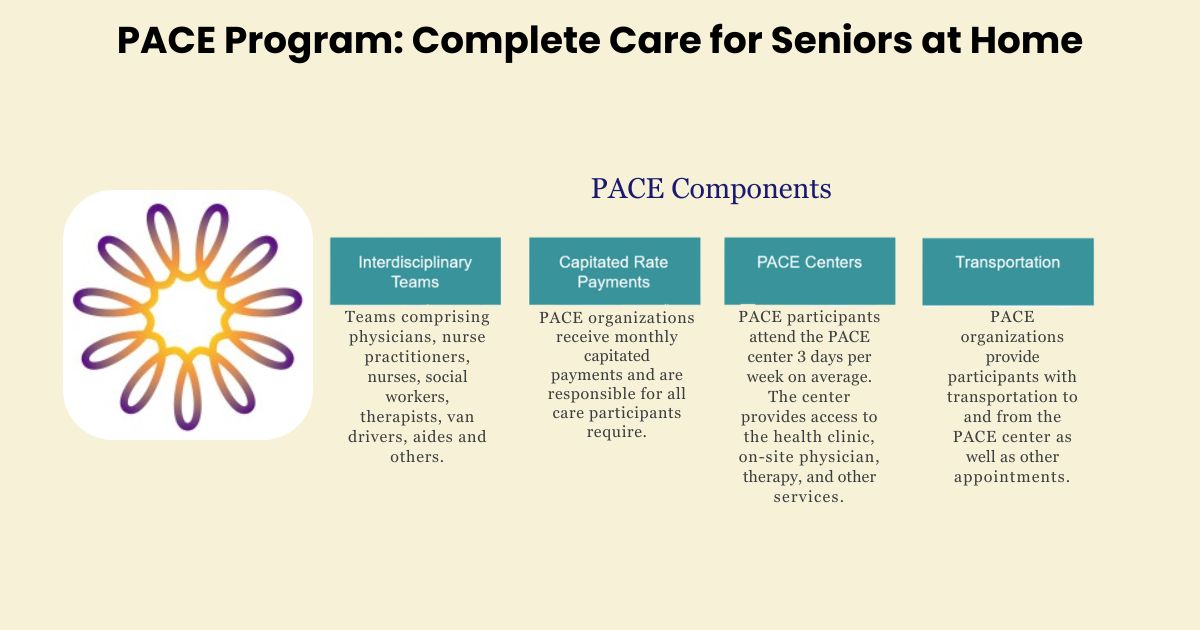
Table of Contents
When your loved one needs more help than you can provide at home but isn’t ready for a nursing home, you might feel stuck between difficult choices. The All-Inclusive Care for the Elderly (PACE) program offers a third option that many families don’t know exists—one that can help seniors get the care they need while staying in their own communities.
PACE stands for Program of All-Inclusive Care for the Elderly. It’s designed specifically for people who qualify for nursing home care but want to continue living at home or in their community. Think of it as a bridge between independent living and institutional care.
This program brings together all the services your loved one needs under one roof—medical care, therapy, meals, transportation, and social activities. Instead of juggling multiple doctors, insurance companies, and service providers, PACE coordinates everything through one team of professionals who get to know your family members personally.
For families, PACE can be a lifeline. It means you don’t have to choose between keeping your loved one at home without adequate support or placing them in a nursing facility before they’re ready. PACE helps seniors maintain their independence while ensuring they receive comprehensive, professional care.
The program also provides peace of mind for family caregivers. You’ll know that your loved one has access to medical care, nutritious meals, social interaction, and emergency support when needed. This can reduce the stress and worry that often comes with caring for an aging family member.
PACE operates on a simple but powerful belief: most seniors prefer to age in their own communities rather than in institutional settings. The program was created with the understanding that older adults thrive when they can maintain connections to their neighborhoods, friends, and familiar surroundings.
The mission of PACE centers around person-centered care. This means that instead of fitting your loved one into a standard care plan, the PACE team creates services around their specific needs, preferences, and goals. Whether someone loves gardening, enjoys playing cards, or has specific dietary needs, the PACE team works to honor these individual preferences.
PACE also believes in preventive care. Rather than waiting for health problems to become emergencies, the program focuses on keeping participants healthy and catching issues early. This approach often helps people avoid hospital stays and maintains their quality of life longer.
The philosophy extends to families, too. PACE recognizes that caring for an aging loved one affects the entire family, so it provides support and resources for caregivers and participants.
This guide is written for patients, caregivers, family members, and healthcare providers who want to understand how PACE might help in their specific situations.
If you’re a senior who needs more support but wants to stay in your community, this information can help you understand what PACE offers and whether it might be right for you.
If you’re a family caregiver, you might feel overwhelmed by the responsibility of caring for your loved one while managing your own life. This guide can help you understand how PACE might provide the support your family needs.
If you’re a family member living far away from an aging parent or relative, PACE might offer comprehensive local support that gives you confidence in your loved one’s care.
Healthcare providers can use this information to better understand PACE as an option for patients who need nursing home-level care but want to remain in the community.
Whether you’re just beginning to explore care options or you’ve been struggling with current arrangements, this guide will help you understand if PACE could be the solution your family has been looking for.
PACE is a comprehensive healthcare program designed specifically for seniors who need nursing home-level care but want to continue living in their communities. The name says it all—it’s truly “all-inclusive,” meaning it covers virtually every healthcare and support service your loved one might need.
Think of PACE as a safety net that catches seniors before they fall through the cracks of traditional healthcare. Instead of piecing together different services from multiple providers, PACE brings everything together under one program. This includes medical care, prescription drugs, therapy services, meals, transportation, and even social activities.
The core purpose is simple but powerful: to help seniors age with dignity in familiar surroundings while receiving the comprehensive care they need. PACE recognizes that most older adults don’t want to leave their homes, neighborhoods, and communities unless absolutely necessary.
PACE serves as both a healthcare provider and a health insurance plan. This dual role means they can coordinate all aspects of care without the usual insurance barriers and approval delays that often frustrate families. The PACE team can make it happen quickly when your loved one needs something—whether it’s a doctor’s appointment, physical therapy, or help with daily activities.
The program is specifically designed for people who are frail or have multiple chronic conditions. If your loved one has been told they qualify for nursing home care, they likely qualify for PACE. This includes people with conditions like dementia, heart disease, diabetes, mobility issues, or those recovering from strokes or other serious health events.
PACE began in the 1970s in San Francisco’s Chinatown with a program called “On Lok,” which means “peaceful, happy abode” in Chinese. The community was facing a crisis—many elderly Chinese immigrants needed nursing home care, but the available facilities couldn’t provide culturally appropriate services or communicate in their language.
A group of community leaders and healthcare professionals came together to create something different. They believed that seniors could receive quality care while staying in their communities if the right support system existed. This wasn’t just about medical care but about preserving dignity, culture, and family connections.
The On Lok model was revolutionary for its time. Instead of waiting for people to get sick and then treating them, the program focused on keeping people healthy and independent for as long as possible. They brought together doctors, nurses, social workers, and other professionals to work as a team, something that wasn’t common in healthcare at the time.
The success in San Francisco’s Chinatown proved that community-based care could work. Participants stayed healthier, lived longer, and reported higher satisfaction with their care compared to those in traditional nursing homes. Families were happier, too, knowing their loved ones could receive excellent care while staying close to home.
Word of On Lok’s success spread throughout the healthcare community. Other communities began asking how to create similar programs for their elderly populations. This led to demonstration projects in other cities, each adapting the model to fit their local communities’ needs.
For many years, PACE existed only as demonstration projects funded by special government grants. While these programs were successful, they served limited numbers of people and weren’t available everywhere. Families and healthcare advocates pushed for PACE to become a permanent part of Medicare so more seniors could benefit.
In 1997, Congress passed legislation making PACE a permanent option under both Medicare and Medicaid. This was a significant milestone because it meant PACE programs could operate with stable, ongoing funding rather than relying on temporary grants.
The decision to make PACE permanent wasn’t made lightly. Congress reviewed years of data showing that PACE participants had better health outcomes, higher satisfaction, and often lower costs compared to traditional nursing home care. The evidence was clear: this model of care worked.
Making PACE a permanent Medicare benefit meant that eligible seniors anywhere in the country could access this type of care. However, PACE programs still need to be established locally, which is why they aren’t yet available in every community.
The 1997 legislation also established quality standards and oversight requirements to ensure that all PACE programs meet high standards of care. This gives families confidence that any PACE program they consider has been thoroughly evaluated and approved by federal and state agencies.
The fundamental philosophy of PACE is that most seniors can live safely and happily in their communities when they have the right support. This stands in contrast to the traditional approach of moving people to nursing homes when they need significant help with daily activities or medical care.
PACE believes that familiar surroundings, family connections, and community ties are essential to a person’s well-being. When someone has lived in a neighborhood for decades, has friends at the local grocery store, and knows every street corner, moving to an institutional setting can be traumatic and disorienting.
The program recognizes that “home” isn’t just a building—it’s a network of relationships, routines, and memories that give life meaning. PACE works to preserve these connections while providing the medical and personal care that keeps people safe and healthy.
This doesn’t mean PACE is against nursing homes. There are times when institutional care is necessary and appropriate. However, PACE believes this should be a last resort, not the first option when someone needs help.
The PACE philosophy extends to how care is delivered. Instead of focusing solely on medical problems, PACE considers the whole person—their interests, preferences, cultural background, and personal goals. Suppose someone loves gardening but has mobility issues. In that case, the PACE team may provide adaptive tools and physical therapy to help them continue enjoying gardening rather than simply accepting that this activity is no longer possible.
PACE also believes in the importance of choice and dignity. Participants aren’t told what they must do; instead, they work with their care team to make decisions about their care. This collaborative approach helps people maintain a sense of control over their lives, which is crucial for emotional and mental well-being.
The program’s philosophy recognizes that aging doesn’t mean giving up on life—it means adapting to changes while maintaining as much independence and joy as possible. This perspective shapes every aspect of PACE programs, from the services they provide to how staff interact with participants and families.
PACE brings together all the healthcare and support services your loved one needs under one coordinated system. Instead of managing appointments with different doctors, therapists, and service providers scattered across town, everything is connected through your PACE program.
This integration means that when your loved one sees the physical therapist, that therapist already knows about their heart condition, medications, and home situation. The social worker understands their medical needs, and the doctor knows about their social challenges. This complete picture helps everyone provide better, more personalized care.
PACE covers both medical services and the daily support that helps people stay independent. Medical services include doctor visits, prescription drugs, hospital care, and specialty treatments. Social services include help with bathing, dressing, meal preparation, transportation, and companionship. By combining these services, PACE addresses the health problems and practical challenges of aging.
The integration also extends to your family. PACE staff understand that caring for an aging loved one affects everyone in the family. They provide support and education to help family caregivers feel more confident and less overwhelmed. This might include teaching you how to help with medications, connecting you with support groups, or simply being available to answer questions when concerns arise.
PACE focuses on keeping people healthy rather than just treating them when they get sick. This preventive approach means regular check-ups, health screenings, and early intervention when problems are detected. Your loved one’s care team watches for warning signs and addresses issues before they become emergencies.
When acute care is needed—such as treatment for pneumonia, a fall, or a heart episode—PACE coordinates everything from the emergency room visit to follow-up care at home. The PACE team stays involved throughout the entire process, ensuring that hospital staff understand your loved one’s complete medical history and that the transition back home goes smoothly.
Long-term care coordination means planning for the future while managing current needs. As your loved one’s condition changes over time, the PACE team adjusts services accordingly. If someone needs more help with daily activities, additional support is arranged. If their medical needs become more complex, the care plan is updated to address these changes.
This coordination eliminates the gaps that often occur in traditional healthcare. You won’t have to worry about whether the hospital knows about all your loved one’s medications or whether the physical therapist understands their cognitive limitations. The PACE team maintains this information and ensures it follows your loved one wherever they receive care.
Every PACE participant has a dedicated team of professionals who work together to provide comprehensive care. This team becomes like an extended family, getting to know your loved one personally and understanding their unique needs, preferences, and goals.
The primary care physician serves as the medical leader of the team. This doctor coordinates all medical care, manages medications, and makes referrals to specialists when needed. Having one doctor who knows your loved one’s complete medical history eliminates the confusion that can happen when multiple doctors aren’t communicating with each other.
Nurses provide hands-on medical care and serve as the daily connection between participants and their care team. They monitor health conditions, provide treatments, educate families about medical care, and help coordinate services. The nursing staff often becomes the most familiar face to participants and families.
The social worker addresses the non-medical challenges that affect health and well-being. This includes helping with insurance questions, connecting families with community resources, providing counseling support, and helping solve practical problems like housing or transportation issues.
Physical and occupational therapists help maintain and improve function. The physical therapist works on mobility, strength, and balance to help prevent falls and maintain independence. The occupational therapist focuses on daily living skills such as dressing, bathing, and cooking, often recommending adaptive equipment to make these tasks easier and safer.
The dietitian ensures that nutritional needs are met. This is especially important for seniors who may have diabetes, heart disease, or other conditions that require special diets. The dietitian also addresses problems such as poor appetite, difficulty swallowing, and unintentional weight loss.
Personal care attendants provide hands-on help with daily activities. They assist with bathing, dressing, grooming, and other personal care needs. These staff members often develop close relationships with participants and provide companionship and practical assistance.
Every day, the entire care team meets to discuss each participant’s needs and coordinate services. These meetings ensure that everyone is working toward the same goals and that nothing falls through the cracks.
During these meetings, team members share observations about how participants are doing physically, emotionally, and socially. If the nurse notices someone seems more confused than usual, the social worker might arrange additional support at home. If the physical therapist observes that someone is having more difficulty walking, the doctor might adjust medications or order further tests.
These daily discussions allow the team to respond quickly to participant condition changes. Instead of waiting for a scheduled appointment to address concerns, the team can make adjustments immediately. This rapid response often prevents small problems from becoming serious emergencies.
The coordination extends beyond the PACE center. The PACE team stays involved when participants receive care in hospitals, emergency rooms, or other facilities. They communicate with outside providers, ensure that care plans are followed, and coordinate the transition back to PACE services.
Each participant has an individualized care plan that reflects their specific needs, preferences, and goals. The team develops this plan together, with participant and family input. The plan is reviewed regularly and updated as needs change.
The team approach means that care decisions are made collaboratively rather than by a single person. If someone is having difficulty managing their diabetes, the doctor, nurse, dietitian, and social worker might all contribute to finding a solution. The doctor adjusts medications, the nurse provides education, the dietitian modifies the meal plan, and the social worker addresses any barriers to following the treatment plan.
Communication is constant among team members. If a personal care attendant notices that someone seems depressed during their home visit, this information is immediately shared with the nurse and social worker. If the physical therapist observes someone at risk for falls, the team works together to address this safety concern.
The team also coordinates with family members and other caregivers. They provide education about medical conditions, teach family members how to provide safe care, and offer support when caregiving becomes overwhelming. This partnership approach recognizes that families are essential members of the care team.
The PACE center is where participants come for medical appointments, therapy sessions, social activities, and meals. Think of it as a one-stop location where your loved one can receive comprehensive care and enjoy social interaction with peers.
Most participants visit the PACE center several times a week, though the frequency depends on individual needs and preferences. Some people come daily for meals and activities, while others visit only for medical appointments and therapy sessions.
The center is designed to feel welcoming and homelike rather than clinical. Common areas are comfortable and inviting, with spaces for socializing, activities, and quiet relaxation. The medical areas are equipped with everything needed for routine care, including examination rooms, therapy areas, and diagnostic testing areas.
Transportation to and from the PACE center is provided as part of the program. PACE vehicles are equipped to accommodate wheelchairs and other mobility aids. The transportation staff are trained to assist participants safely and are familiar with each person’s specific needs.
Medical services at the PACE center include routine check-ups, medication management, wound care, and monitoring of chronic conditions. Having these services on-site means fewer trips to multiple medical offices and better coordination of care.
Therapy services are available right at the center. Physical therapy helps maintain mobility and prevent falls. Occupational therapy focuses on daily living skills and may include practice with adaptive equipment. Speech therapy addresses communication and swallowing problems. Having all therapies in one location makes coordinating treatment and tracking progress easier.
Social activities are a vital part of the PACE experience. These might include games, crafts, music programs, educational presentations, and holiday celebrations. The activities are designed to provide mental stimulation, social interaction, and enjoyment. Many participants say that the friendships they form at the PACE center are one of the most valuable aspects of the program.
Nutritious meals are provided daily at the PACE center. The dietitian ensures that meals meet individual dietary requirements and preferences. For many participants, the social aspect of sharing meals with friends is as important as the nutrition. The dining area becomes a gathering place where people can enjoy conversation and companionship.
The PACE center also serves as a respite for family caregivers. Knowing that your loved one is in a safe, supervised environment with access to medical care and social interaction gives families peace of mind and allows them time to attend to their own needs.
All services at the PACE center are coordinated through the care team. If someone needs to see the doctor, receive physical therapy, and participate in a social activity, the schedule is arranged so these services complement each other rather than conflict. This coordination makes the day more pleasant and productive for participants.
PACE provides all the medical care your loved one needs, starting with a primary care doctor who becomes the central coordinator of their health. This isn’t just any doctor—it’s a physician who specializes in caring for older adults and understands the complex medical needs that come with aging.
Your loved one will see their primary care doctor regularly, not just when they’re sick. These routine visits help catch health problems early and keep chronic conditions like diabetes, heart disease, and high blood pressure under control. The doctor gets to know your family member personally, understanding their medical history, preferences, and concerns.
When specialty care is needed, PACE arranges visits with specialists such as cardiologists, neurologists, and orthopedic doctors. The beauty of the PACE system is that your primary care doctor stays involved and coordinates with these specialists. You won’t have to worry about different doctors giving conflicting advice or not knowing about other treatments your loved one is receiving.
All medical records are shared among the care team, so every provider has a complete picture of your loved one’s health. This coordination prevents dangerous drug interactions, duplicate tests, and conflicting treatment plans that can happen when seniors see multiple doctors who don’t communicate with each other.
The medical team also includes nurse practitioners and physician assistants who can handle many routine medical needs. This means your loved one can get medical attention quickly without always waiting for the doctor to be available.
When medical emergencies happen, PACE coordinates everything from the ambulance ride to the hospital stay and back home again. The PACE team doesn’t disappear when your loved one needs emergency care—they remain involved throughout the entire process.
If your loved one needs to go to the emergency room, the PACE medical team communicates directly with the hospital staff. They provide the complete medical history, current medications, and essential information about your family member’s preferences and needs. This communication helps emergency room doctors make better decisions faster.
During hospital stays, PACE staff visit regularly to ensure your loved one is receiving appropriate care and to help with the transition back home. They work with hospital discharge planners to make sure all necessary equipment, medications, and follow-up care are arranged before your loved one leaves the hospital.
PACE also covers urgent care needs that aren’t quite emergencies. If your loved one develops a fever, has a fall, or experiences other concerning symptoms, they can be seen quickly by the PACE medical team rather than waiting for a regular appointment or going to an emergency room.
The program includes coverage for ambulance services when they’re medically necessary. This means families don’t have to worry about the cost of emergency transportation or make difficult decisions about whether to call for help.
All prescription medications are covered through PACE, with no copayments or deductibles. The PACE pharmacist works closely with the medical team to ensure each participant’s medications are appropriate, safe, and effective.
Medication management is a crucial service, especially for seniors taking multiple prescriptions. The PACE team monitors drug interactions, side effects, and effectiveness. They also help with practical issues like organizing pills, setting up reminder systems, and teaching family members how to manage medications safely.
PACE covers both brand-name and generic medications, choosing the most appropriate option for each person’s needs. The pharmacist can also work with doctors to find alternative medicines if cost or availability becomes an issue.
Dental care is included in PACE services, which is unusual since traditional Medicare doesn’t cover most dental work. PACE provides routine dental cleanings, fillings, extractions, and dentures when needed. Good oral health is especially important for seniors because dental problems can affect nutrition, speech, and overall health.
Dental services are coordinated with the medical team because dental health is vital for overall health. For example, gum disease can worsen diabetes, and certain medications can cause dry mouth, leading to dental problems.
Physical therapy through PACE focuses on helping your loved one move safely and maintain their independence for as long as possible. The physical therapist works on balance, mobility, and strength to prevent falls and help with daily activities like walking, getting in and out of chairs, and climbing stairs.
The approach is practical and focused on real-life needs. Instead of generic exercises, the physical therapist designs activities that help with specific challenges your loved one faces at home. This might include practicing getting up from their favorite chair, navigating stairs safely, or using a walker effectively.
Occupational therapy helps with the daily activities that make life meaningful and independent. This includes bathing, dressing, cooking, managing medications, and using adaptive equipment that makes these tasks easier and safer. The occupational therapist might recommend grab bars, shower seats, or special utensils that help your loved one continue doing things for themselves.
Recreational therapy is often overlooked but is incredibly important for emotional and mental well-being. The recreational therapist helps your loved one stay engaged in activities they enjoy or discover new interests. This might include adapted gardening, art projects, music activities, or games that provide mental stimulation and social interaction.
All therapy services are coordinated with the medical team and adjusted as your loved one’s needs change. The therapists work together to address speech, movement, and daily living skills if someone is recovering from a stroke. If someone has dementia, the therapy focuses on maintaining abilities and providing comfort rather than trying to restore lost functions.
PACE provides personal care attendants who come to your loved one’s home to help with daily activities. This includes assistance with bathing, dressing, grooming, toileting, and other personal care needs that help people maintain their dignity and cleanliness.
The personal care attendants are trained specifically to work with older adults and understand the importance of treating each person with respect and compassion. They’re not just there to complete tasks—they provide companionship and emotional support that can be just as valuable as the physical assistance.
Home care services are flexible and can be adjusted based on changing needs. One person might need help only with bathing a few times a week, while another might need daily assistance with multiple activities. The PACE team regularly evaluates what’s needed and adjusts services accordingly.
Personal care attendants also serve as the eyes and ears of the care team in the home. They report changes in your loved one’s condition, safety concerns, or other issues that need attention. This communication helps the medical team respond quickly to problems before they become serious.
The home care services also include light housekeeping related to health and safety, such as keeping pathways clear to prevent falls, ensuring the bathroom is clean and safe, and helping with laundry that affects hygiene and comfort.
PACE provides transportation to all medical appointments, therapy sessions, and PACE center activities. The vehicles are equipped to accommodate wheelchairs, walkers, and other mobility aids. The drivers are trained to assist participants safely and understand each person’s specific needs.
Transportation isn’t limited to medical needs. PACE may also provide rides to essential errands like grocery shopping, pharmacy visits, or other appointments that affect health and well-being. This service is especially valuable for seniors who can no longer drive safely or don’t have family members available to provide transportation.
The nutrition program includes meals at the PACE center and home-delivered meals when needed. The dietitian designs all meals to meet individual dietary requirements and preferences. This is especially important for people with diabetes, heart disease, kidney problems, or other conditions that require special diets.
Home-delivered meals ensure your loved one has access to nutritious food even when they can’t reach the PACE center. These meals are particularly valuable during illness, bad weather, or mobility problems, which make preparing food safely difficult.
The nutrition program also includes nutrition education and counseling. The dietitian works with participants and families to address problems like poor appetite, unintentional weight loss, difficulty swallowing, or confusion about dietary restrictions.
The social worker provides counseling and support for both participants and their families. This includes help with adjusting to changes in health or function, coping with chronic illness, dealing with loss and grief, and managing the emotional challenges that come with aging.
Social work services include practical assistance with insurance questions, benefit applications, housing issues, and connecting families with community resources. The social worker can help navigate complex systems and advocate for your loved one’s needs.
Family counseling and support are essential parts of the social work services. Caring for an aging loved one can be emotionally and physically exhausting. The social worker provides support groups, individual counseling, and practical advice to help family caregivers manage their responsibilities without becoming overwhelmed.
Respite care gives family caregivers a break from their responsibilities. This might include additional hours of personal care assistance at home, extended time at the PACE center, or temporary placement in a care facility when families need to travel or handle other responsibilities.
The social worker also helps with advance care planning and end-of-life decisions. This includes discussions about preferences for care, completion of advance directives, and support for families facing difficult decisions about treatment options.
All social work services are provided with compassion and respect for individual values and preferences. The goal is to support both participants and families through the challenges of aging while maintaining dignity and quality of life.
PACE is designed for older adults, with most programs requiring participants to be at least 55 years old. This age requirement recognizes that people in their mid-50s and beyond may start experiencing health challenges that make it difficult to manage their care independently.
The age requirement isn’t arbitrary—it reflects the reality that complex health needs often begin to emerge in the mid-50s. People in this age group may be dealing with chronic conditions like diabetes, heart disease, or arthritis that require ongoing medical management and support services.
Some PACE programs may have slightly different age requirements, but 55 is the standard minimum age across most programs. If your loved one is close to this age and has significant health needs, it’s worth contacting your local PACE program to discuss their specific requirements.
Age alone doesn’t determine eligibility—your loved one must also meet the other requirements. However, being 55 or older is the first step in determining whether PACE might be an option for your family.
PACE programs aren’t available everywhere, which can be disappointing for families who would benefit from these services. Currently, PACE operates in 33 states and the District of Columbia, but even within these states, programs may only serve specific counties or regions.
Each PACE program has a defined service area where participants must live. This requirement exists because PACE provides transportation, home care services, and emergency response that need to be geographically manageable. The program can’t effectively serve someone who lives hours away from the PACE center.
If you’re considering PACE, the first step is to find out if a program operates in your area. You can search for PACE programs through the Medicare website or by contacting your state’s aging services department. Some areas may have waiting lists if the local PACE program is at capacity.
Geographic requirements also mean that if your loved one moves to a different area, they may need to transfer to a new PACE program or find alternative care options. If your family is thinking about relocating, this is something to consider.
This is often the most confusing requirement for families to understand. “Nursing home level of care” doesn’t mean your loved one needs to be bedridden or unable to think clearly. Instead, it means they need ongoing assistance and medical supervision that typically requires placement in a nursing facility.
People who qualify for nursing home level of care typically need help with multiple daily activities. This might include bathing, dressing, using the bathroom, eating, or moving around safely. They may also have medical conditions that require regular monitoring and intervention by healthcare professionals.
The certification process involves a comprehensive assessment by state officials or their designated representatives. They evaluate your loved one’s physical health, mental status, ability to perform daily activities, and need for medical supervision. This assessment determines whether the level of care needed would typically require nursing home placement.
Having a nursing home level of care certification doesn’t mean your loved one must go to a nursing home. In fact, PACE is specifically designed for people who meet this criterion but want to remain in their communities. The certification simply confirms that the level of care needed is significant enough to qualify for PACE services.
Even with PACE services, participants must be able to live safely in a community setting rather than requiring the 24-hour supervision of an institutional facility. This requirement ensures that PACE can provide adequate support while maintaining the program’s community-based philosophy.
“Living safely in the community” means different things to different people. For some, it might mean living independently in their home with support from PACE services. For others, it might mean living in an assisted living facility or with family members while receiving PACE services.
The key factor is that your loved one can be safe with the supervision and support provided by PACE. This includes having a safe living environment, being able to follow basic safety instructions, and not requiring constant medical monitoring that can only be provided in a hospital or nursing facility.
PACE teams work with families to address safety concerns and make modifications that allow people to remain in the community. This might include installing grab bars, arranging for more frequent check-ins, or providing additional personal care assistance.
When healthcare professionals talk about “nursing home level of care,” they’re referring to a specific standard of need that goes beyond what most people can manage with occasional help. This level of care involves needing assistance with basic daily activities, combined with medical supervision that requires professional healthcare staff.
The assessment looks at six key areas of daily living: bathing, dressing, eating, using the bathroom, moving around, and maintaining continence. If your loved one needs help with several of these activities on a regular basis, they may meet the criteria for nursing home level of care.
Medical complexity is another important factor. Someone with multiple chronic conditions that require frequent monitoring, medication management, and medical interventions may qualify even if they can still perform some daily activities independently. Examples include people with advanced heart disease, diabetes with complications, or moderate to severe dementia.
The assessment also considers cognitive function and safety awareness. Someone who becomes confused about medications, forgets to eat, or doesn’t recognize dangerous situations may need a nursing home level of care, even if they’re physically capable of many activities.
It’s important to understand that this assessment isn’t about whether your loved one should go to a nursing home—it’s about determining whether they need that level of comprehensive care and support. PACE provides this level of care in a community setting, which is why the certification is required.
Each state has trained assessors who evaluate potential PACE participants using standardized assessment tools. These assessors are typically nurses, social workers, or other healthcare professionals who specialize in evaluating older adults’ care needs.
The comprehensive assessment process looks at physical health, mental status, social situation, and safety factors. The assessor will review medical records, talk with your loved one and family members, and may observe your loved one performing daily activities.
States use specific criteria and scoring systems to ensure consistency in determining eligibility. This means that someone with similar needs should qualify for PACE regardless of which assessor evaluates them or when the assessment takes place.
The assessment considers not just current needs but also the trajectory of your loved one’s condition. Someone whose health is declining and who will likely need increasing levels of care may qualify for PACE even if their current needs seem manageable.
States also consider the availability of informal support from family and friends. Someone living alone with limited family support might qualify for PACE with fewer care needs than someone who has extensive family assistance available.
The PACE eligibility assessment typically takes several weeks from start to finish, though this can vary depending on your location and the assessor’s schedule. It’s important to start this process as soon as you think PACE might be helpful, rather than waiting until a crisis occurs.
The initial contact with PACE usually involves a phone screening to determine if your loved one might be eligible. A formal assessment will be scheduled if the screening suggests they could qualify. This preliminary step helps avoid unnecessary assessments for people who clearly don’t meet the basic requirements.
The formal assessment usually takes place in your loved one’s home and can last several hours. The assessor needs time to thoroughly evaluate physical abilities, cognitive function, medical needs, and safety factors. They’ll also want to see the living environment and understand what support systems are already in place.
After the assessment, it typically takes one to two weeks to receive the eligibility determination. If your loved one qualifies, the PACE program will contact you to begin the enrollment process. If they don’t qualify, you’ll receive information about the decision and may have options for appealing if you disagree with the assessment.
The timeline may be longer during busy periods or in areas with limited assessors. If your loved one’s situation is urgent, let the PACE program know when you first contact them. They may be able to expedite the process or suggest interim resources while you wait for the assessment.
Preparing for the assessment by gathering medical records, medication lists, and information about current care providers can help. Having this information readily available can make the assessment process smoother and more accurate.
The cost of PACE depends on your loved one’s insurance coverage, and the good news is that many people pay very little or nothing at all. Understanding how PACE pricing works can help you plan financially and make informed decisions about this care option.
If your loved one has both Medicare and Medicaid (called “dual eligible”), they typically pay no monthly premium for PACE services. This is one of the most significant advantages of PACE for families with limited income. All services are covered without any out-of-pocket costs, making comprehensive care affordable for those who need it most.
There is a monthly premium for people who have Medicare but don’t qualify for Medicaid. This premium varies by location and PACE program, but it’s designed to be reasonable compared to the cost of purchasing similar services separately. The premium covers all medical care, medications, therapy, transportation, meals, and support services.
Some PACE programs offer sliding scale premiums based on income for people who don’t qualify for Medicaid but have limited financial resources. This helps make PACE accessible to middle-income seniors who might otherwise struggle to afford comprehensive care.
Private pay participants—those who don’t have Medicare or Medicaid—pay the full monthly cost. While this is the most expensive option, it’s often still less than the combined cost of nursing home care, medical insurance, and additional services that would be needed separately.
The monthly premium structure makes budgeting easier because you know exactly what PACE will cost each month, regardless of how many services your loved one uses. This predictability is especially valuable for families managing fixed incomes.
One of the most significant financial benefits of PACE is that there are no deductibles, copayments, or coinsurance for any approved services. This means your loved one can see the doctor, receive therapy, get medications, or use any other PACE service without paying additional fees each time.
This is very different from traditional Medicare, where your loved one might pay copayments for doctor visits, coinsurance for hospital stays, and separate costs for medications. With PACE, once the monthly premium is paid (if applicable), all covered services are included at no additional cost.
The “no copayment” benefit is especially valuable for people with chronic conditions who need frequent medical care. Someone with diabetes, heart disease, or other ongoing health issues might see healthcare providers multiple times per month. Under traditional Medicare, these visits could result in significant out-of-pocket costs, but with PACE, they’re all covered.
Prescription medications are included without copayments, which can result in substantial savings. Many seniors spend hundreds of dollars monthly on medications, but PACE participants receive all necessary prescriptions at no additional cost.
Emergency room visits, hospital stays, and specialist appointments are also covered without additional fees. This protection is crucial because medical emergencies can create unexpected financial burdens for families on fixed incomes.
The no-copayment structure also eliminates the difficult decisions that some seniors face about whether they can afford needed medical care. With PACE, your loved one can receive all necessary services without worrying about the cost of each visit or treatment.
PACE uses what’s called a “capitated payment system,” which means the program receives a fixed amount of money each month to provide all of your loved one’s care. This system is different from traditional healthcare, where providers are paid separately for each service they provide.
Under the capitated system, PACE receives the same monthly payment regardless of whether your loved one uses many services or few services. This creates an incentive for PACE to keep participants healthy and prevent expensive medical emergencies rather than simply treating problems after they occur.
The capitated payment comes from Medicare, Medicaid, or private payments, depending on your loved one’s insurance coverage. PACE then uses this money to provide all necessary medical care, support services, medications, and other benefits included in the program.
This system benefits participants because it encourages preventive care and early intervention. Since PACE doesn’t make more money by providing more services, they focus on keeping people healthy and independent rather than maximizing the number of treatments or procedures.
The capitated system also provides financial predictability for families. You know that all of your loved one’s healthcare needs will be covered for the monthly premium, without surprise bills or unexpected costs for additional services.
PACE programs must carefully manage their resources under this system, which means they focus on providing efficient, effective care. This often results in better coordination of services and more personalized care plans that address individual needs rather than applying one-size-fits-all approaches.
Most PACE participants use Medicare and Medicaid to pay for their services, and understanding how these programs work with PACE can help you determine what your family will pay. The combination of these two government programs often provides comprehensive coverage with minimal out-of-pocket costs.
If your loved one has both Medicare and Medicaid, they’re considered “dual eligible,” and PACE services are typically provided at no cost to the family. Medicare pays for medical services, while Medicaid covers the long-term care and support services that help people remain in their communities.
For people who have Medicare but don’t qualify for Medicaid, Medicare covers the medical portion of PACE services. This includes doctor visits, hospital care, medications, and therapy services. However, a monthly premium will cover the additional support services that Medicare doesn’t typically pay for, such as personal care assistance and meals.
Medicaid eligibility can change over time, especially if your loved one’s financial situation changes due to medical expenses. Some people who initially pay a premium for PACE may later qualify for Medicaid, which would eliminate their monthly costs. The PACE social worker can help families understand and apply for Medicaid benefits.
PACE programs work directly with Medicare and Medicaid, so families don’t have to handle insurance paperwork or claims. The program manages all the billing and administrative tasks, making the process much simpler for participants and their families.
It’s important to understand that enrolling in PACE means your loved one will receive all their healthcare through the PACE program. They can’t use other Medicare providers or services outside of PACE except in emergency situations or with prior approval.
Some people choose to pay for PACE services privately, either because they don’t qualify for Medicare and Medicaid or because they prefer to maintain private pay status. Private pay arrangements give families more control over their healthcare decisions but come with higher costs.
Private pay participants typically pay the full monthly cost of PACE services. While this is more expensive than insurance coverage, it’s often still less than the combined cost of nursing home care, private health insurance, and additional services needed separately.
Private pay can be a good option for people who have assets that make them ineligible for Medicaid but want the comprehensive care and community-based approach that PACE provides. Some families prefer this option to avoid the asset limitations that come with Medicaid eligibility.
PACE programs may offer different payment arrangements for private pay participants, such as quarterly or annual payment options that might provide some cost savings. Some programs also offer payment plans that make the monthly costs more manageable for families.
Private pay participants receive the same comprehensive services as those covered by Medicare and Medicaid. There’s no difference in the quality or scope of care based on how services are paid for.
Families considering private pay should carefully evaluate their long-term financial situation. The costs can add up significantly over time, and it’s important to ensure that paying for PACE won’t exhaust resources that might be needed for other purposes.
One of the greatest financial advantages of PACE is the predictability it provides for healthcare expenses. Families know exactly what they’ll pay each month, which makes budgeting much easier and eliminates the worry about unexpected medical bills.
The comprehensive nature of PACE services often results in significant cost savings compared to purchasing similar services separately. When you add up the costs of medical care, medications, therapy, transportation, meals, and personal care assistance, PACE typically provides better value than trying to arrange these services individually.
PACE can help protect families from the financial devastation that often comes with serious illness or injury. Because all medical care is covered, families don’t have to worry about choosing between necessary treatments and financial security.
The program’s focus on preventive care and early intervention can result in long-term cost savings. By keeping people healthier and preventing medical emergencies, PACE often reduces the need for expensive hospital stays and emergency treatments.
For families concerned about the cost of long-term care, PACE provides an often more affordable alternative to nursing home placement. The average cost of nursing home care is typically higher than PACE premiums, and PACE allows people to remain in their communities.
PACE also eliminates many of the hidden costs associated with aging and chronic illness. Transportation to medical appointments, special dietary needs, adaptive equipment, and other support services are all included in the program rather than being additional expenses for families.
The financial benefits extend to family caregivers as well. Because PACE provides comprehensive support, family members may be able to continue working rather than leaving their jobs to provide care. This protection of family income can be just as valuable as the direct cost savings from PACE services.
PACE programs are currently available in 33 states plus the District of Columbia, but this doesn’t mean every community in these states has one. The availability depends on local organizations that have chosen to develop PACE services and have received approval to operate.
The states with PACE programs include major population centers like California, New York, Florida, and Texas, as well as smaller states like Vermont and Rhode Island. However, even within these states, PACE programs typically serve specific geographic areas or counties rather than entire states.
If you live in a state without PACE programs, you may need to consider other care options or explore whether any neighboring states have programs near your area. Some PACE programs serve communities close to state borders, though you would need to live within their designated service area.
New PACE programs are being developed regularly as communities recognize the value of this care model. If PACE isn’t available in your area now, it’s worth checking periodically to see if new programs are being planned or developed.
Geographic limitations are one of the biggest challenges families face when considering PACE. Many people who would benefit greatly from PACE services simply don’t have access because no program operates in their community. This is why it’s important to check availability early in the care planning process.
The easiest way to find PACE programs in your area is through Medicare’s official website at Medicare.gov. The site has a specific search tool that allows you to enter your zip code and find nearby PACE programs along with their contact information.
When you search on Medicare.gov, you’ll get information about each PACE program, including its address, phone number, and service area. This helps you determine whether a program exists nearby and whether your loved one’s specific address falls within their service boundaries.
The Medicare search tool also provides basic information about each program’s services and may include links to the program’s website. This can help you learn more about specific programs before contacting them.
You can also call Medicare directly at 1-800-MEDICARE (1-800-633-4227) to get help finding PACE programs in your area. The customer service representatives can search for you and provide contact information for local programs.
State aging services departments are another valuable resource for finding PACE programs. These departments often have comprehensive information about all long-term care options in your state, including PACE programs, and can help you understand what’s available.
Local Area Agencies on Aging can also provide information about PACE programs and other care options in your community. These agencies specialize in helping older adults and their families navigate available services and often have staff who are very familiar with PACE programs.
The first step in applying to PACE is making initial contact with your local program. This usually involves a phone call where program staff will ask basic questions about your loved one’s age, health conditions, and care needs to determine if PACE might be appropriate.
The PACE program will schedule a comprehensive assessment if the initial screening suggests your loved one might be eligible. This assessment is typically conducted in your loved one’s home and can take several hours as the assessor evaluates physical abilities, cognitive function, medical needs, and safety factors.
The assessment process includes reviewing medical records, talking with your loved one and family members, and observing how your loved one manages daily activities. The assessor needs to understand not just current needs but also the trajectory of your loved one’s condition and what support systems are already in place.
After the assessment, the eligibility determination typically takes one to two weeks to receive. If your loved one qualifies for PACE, the program will contact you to begin the enrollment process. If they don’t qualify, you’ll receive information about the decision and may have options for appealing.
The enrollment process involves completing paperwork, understanding the program’s policies and procedures, and making arrangements for your loved one to begin receiving services. This includes setting up transportation, scheduling initial appointments, and coordinating with current healthcare providers.
During enrollment, you’ll also need to make decisions about your loved one’s existing healthcare providers and insurance coverage. Enrolling in PACE means receiving all healthcare through the PACE program, so you’ll need to understand how this transition will work.
The PACE assessment is comprehensive and designed to understand your loved one’s complete situation, not just their medical needs. The assessor will evaluate physical health, mental status, ability to perform daily activities, social situation, and safety factors in the home environment.
During the assessment, be prepared to discuss your loved one’s medical history, current medications, and any recent changes in their condition. The assessor will also want to understand what help your loved one currently receives from family members, friends, or paid caregivers.
The assessor will observe your loved one performing various activities to understand their actual abilities rather than relying only on what they or family members report. This might include watching them walk, get up from a chair, or perform simple tasks like making a sandwich.
The home environment assessment looks at safety factors like lighting, stairs, bathroom accessibility, and general cleanliness. The assessor isn’t judging your housekeeping but rather identifying potential safety hazards or modifications that might be needed.
If your loved one qualifies for PACE, the orientation process introduces them to the program’s services and staff. This typically includes a visit to the PACE center, meeting key team members, and understanding the daily routine and available activities.
During orientation, the PACE physician and other team members will provide your loved one with a comprehensive medical evaluation. This helps the team understand your loved one’s current health status and begin developing an individualized care plan.
The orientation process also includes practical arrangements like setting up transportation schedules, understanding meal programs, and learning how to contact the PACE team when questions or concerns arise. The goal is to make the transition to PACE services as smooth as possible.
Family members are encouraged to participate in the orientation process. This helps ensure that everyone understands how PACE works, what services are available, and how family members can continue to be involved in their loved one’s care.
The PACE team will work with you to coordinate the transition from your current healthcare providers to PACE services. This includes transferring medical records, coordinating medications, and ensuring that there are no gaps in care during the transition period.
It’s normal to feel overwhelmed during the assessment and orientation process. PACE staff understand that this is a significant decision and transition for families. They’re available to answer questions, address concerns, and provide support throughout the process.
Most PACE participants visit the center several times a week, creating a routine that provides structure, social connection, and comprehensive care all in one place. The daily schedule is designed to feel natural and comfortable rather than rigid or institutional.
A typical day at the PACE center might begin with arrival between 8:00 and 9:00 AM, when participants are greeted by familiar staff members who know them by name. This personal touch helps create a welcoming atmosphere that feels more like visiting friends than going to a medical facility.
Morning activities often include a nutritious breakfast and time for socializing with other participants. Many people find that sharing meals and conversation becomes one of their favorite parts of the PACE experience. These social connections can be especially meaningful for people who might otherwise spend much of their time alone.
Medical appointments and therapy sessions are scheduled throughout the day, but they’re woven into the routine in a way that doesn’t feel overwhelming. Your loved one might see the doctor in the morning, participate in a group activity after lunch, and have physical therapy in the afternoon—all without having to travel to different locations.
Activities at PACE centers are designed to be enjoyable and meaningful rather than just ways to pass the time. This might include art projects, music programs, gardening, games, educational presentations, or holiday celebrations. The activities are adapted to accommodate different abilities and interests, ensuring everyone can participate in ways that feel comfortable.
The pace of the day is relaxed and flexible. The staff can adjust the schedule if your loved one is having a difficult day or doesn’t feel well. There’s no pressure to participate in every activity or follow a strict routine.
Lunch is typically served around noon and provides another opportunity for social interaction and good nutrition. The meals are prepared by the PACE center’s kitchen staff under the guidance of a dietitian, ensuring they meet individual dietary needs and preferences.
Afternoon activities might include quiet time for those who need rest, continued social activities for those who want to stay engaged, or additional medical appointments as needed. The goal is to create a day that feels balanced and fulfilling rather than exhausting.
Building relationships with your PACE care team is one of the most important aspects of the program’s success. These professionals become familiar with your loved one’s personality, preferences, and needs in ways that create truly personalized care.
Communication with the care team should feel natural and comfortable. The staff encourages questions and wants to hear about any concerns or changes you notice in your loved one’s condition. You don’t need to wait for scheduled appointments to share important information—the team is available when you need them.
Your loved one’s care plan is developed collaboratively, with input from the participant, family members, and all team members. This isn’t something that’s decided for your loved one—it’s created with them based on their goals, preferences, and values.
Regular care plan meetings provide opportunities to discuss how things are going and make adjustments as needed. These meetings include your loved one and family members, ensuring everyone has a voice in care decisions. The team wants to understand what’s working well and what might need to be changed.
The care team communicates with each other constantly throughout the day. If the nurse notices that your loved one seems more tired than usual, this information is immediately shared with the doctor and social worker. This ongoing communication helps catch problems early and prevents small issues from becoming bigger concerns.
Family members are considered essential partners in the care team. The staff want to understand your observations about your loved one’s condition and any concerns you might have. They also provide education and support to help you feel more confident in your caregiving role.
Advocacy is an important part of working with the care team. If you feel that your loved one’s needs aren’t being met or if you disagree with a care decision, the team wants to hear from you. They’re committed to finding solutions that work for everyone involved.
PACE transportation is much more than just a ride to and from the center—it’s often the first and last interaction your loved one has with PACE staff each day. The drivers are trained to assist participants safely and often develop caring relationships with the people they transport.
The vehicles are equipped to accommodate wheelchairs, walkers, and other mobility aids. The drivers know how to help people get in and out of the vehicle safely and understand each participant’s specific needs and preferences.
Transportation schedules are flexible and can be adjusted based on your loved one’s needs and preferences. If they prefer to arrive later in the morning or need to leave early for a family event, the PACE team can usually accommodate these requests.
The ride to and from the PACE center often becomes a social experience. Participants may develop friendships with others who share their transportation route, creating connections beyond the center.
PACE also provides transportation to medical appointments, therapy sessions, and other healthcare services outside the center. This eliminates the stress and expense of arranging medical transportation and ensures your loved one doesn’t miss important appointments.
Social engagement at PACE centers goes far beyond organized activities. Many participants develop genuine friendships with other participants and look forward to seeing familiar faces each day. These relationships can provide emotional support, companionship, and a sense of belonging.
The social aspect of PACE is especially valuable for people who might otherwise be isolated. Spending time with peers who understand similar challenges can reduce feelings of loneliness and depression while providing opportunities for laughter, conversation, and shared experiences.
Staff members also contribute to social engagement by getting to know participants as individuals. They remember birthdays, ask about family members, and show genuine interest in each person’s life and experiences.
One of the most important things to understand about PACE is that participation is always voluntary. Your loved one can choose how much or how little they want to participate in center activities, and they can decide to leave the program at any time if it’s not meeting their needs.
The frequency of visits to the PACE center can be adjusted based on your loved one’s preferences and needs. Some people enjoy coming to the center every day, while others prefer to visit just a few times a week. The program can accommodate different preferences as long as medical and safety needs are met.
If your loved one is having a difficult day or doesn’t feel well, they don’t have to participate in scheduled activities. The staff understand that energy levels and moods can vary, and they’re flexible in accommodating these natural fluctuations.
PACE participants can choose to disenroll from the program at any time. This might happen if their needs change, if they want to try a different care approach, or if they simply decide that PACE isn’t the right fit for them. There are no penalties for leaving the program.
The voluntary nature of PACE extends to specific services as well. While the care team might recommend certain treatments or activities, participants always have the right to refuse services they don’t want. The team respects these decisions while continuing to provide information and support.
Flexibility also applies to family involvement. Some families prefer to be very involved in daily activities and care decisions, while others prefer to step back and let the PACE team take the lead. The program can accommodate different family dynamics and preferences.
The PACE philosophy recognizes that each person’s needs and preferences are unique. What works well for one participant might not work for another, and the program is designed to adapt to these individual differences rather than requiring everyone to fit into the same mold.
This flexibility and respect for choice help maintain your loved one’s dignity and sense of control over their life. Even when they need significant help with daily activities, they can still make meaningful decisions about their care and how they spend their time.
PACE makes it possible for seniors to remain in their own homes and communities even when they need nursing home-level care. This is perhaps the most significant benefit of the program, as most older adults strongly prefer to stay in familiar surroundings rather than move to institutional settings.
Staying at home means maintaining connections to neighbors, friends, and familiar places that have been part of your loved one’s life for years. These connections provide emotional comfort and a sense of continuity that can be crucial for mental and emotional well-being during times of declining health.
PACE provides all the support services needed to make aging in place safe and successful. This includes medical care, personal assistance, home modifications, and emergency response systems that work together to create a comprehensive safety net around your loved one.
The program helps families avoid the difficult and often traumatic decision of nursing home placement. Many families struggle with guilt and worry when considering institutional care, and PACE offers a viable alternative that honors both safety needs and personal preferences.
Aging in place through PACE also means maintaining independence and dignity. Your loved one can continue to make choices about their daily routine, keep their personal belongings, and maintain the privacy and autonomy that comes with living in their own space.
PACE eliminates the frustration and confusion that often come with managing multiple healthcare providers, insurance companies, and service agencies. Everything is coordinated through one program, with one team of professionals who communicate with each other daily.
The comprehensive nature of PACE means that all of your loved one’s needs are addressed—medical, social, emotional, and practical. Instead of having gaps in care or services that don’t work well together, PACE provides a complete package of support that’s tailored to individual needs.
Coordination extends to emergency situations as well. When your loved one needs hospital care or emergency treatment, the PACE team stays involved throughout the process, ensuring continuity of care and smooth transitions back to home-based services.
The program’s focus on preventive care helps catch health problems early, often preventing serious complications or hospitalizations. Regular monitoring and early intervention can help maintain your loved one’s health and independence longer than traditional healthcare approaches.
Medication management is seamlessly integrated into the care plan, eliminating dangerous drug interactions and ensuring that all medications work together effectively. The PACE pharmacist coordinates with the medical team to optimize medication regimens for each individual.
PACE centers provide daily opportunities for social interaction with peers who understand similar challenges. These relationships can reduce isolation, depression, and anxiety while providing companionship, laughter, and emotional support.
The social aspect of PACE often becomes one of the most valued benefits for participants. Many people develop genuine friendships at the center and look forward to seeing familiar faces each day. These connections can provide a sense of purpose and belonging that’s crucial for emotional well-being.
Family support is built into the PACE program through education, counseling, and respite services. The program recognizes that caring for an aging loved one affects the entire family and provides resources to help everyone cope with the challenges and changes.
PACE staff provide ongoing support and guidance to family caregivers, helping them feel more confident and less overwhelmed in their caregiving roles. This might include teaching practical skills, providing emotional support, or connecting families with additional resources.
The program also offers respite care, giving family caregivers breaks from their responsibilities. This support helps prevent caregiver burnout and allows family members to maintain their own health and well-being while caring for their loved one.
The biggest challenge with PACE is that it’s not available everywhere. Currently operating in only 33 states and the District of Columbia, many families who would benefit from PACE simply don’t have access to the program in their communities.
Even within states that have PACE programs, availability is often limited to specific counties or regions. This means that families might live in a state with PACE programs but still be unable to access services because they’re outside the service area.
The geographic limitation can be particularly frustrating for families who are considering relocating to be closer to PACE services. Moving to a new community just to access healthcare can be disruptive and may not be practical for many families.
Limited availability also means that some PACE programs have waiting lists. Even if you live in a service area, you might have to wait months before your loved one can begin receiving services.
Some seniors find it difficult to adjust to the structured nature of PACE programs. After years of managing their own schedules and making independent decisions, the routine of regular center visits and coordinated care can feel restrictive.
While the social aspect of PACE centers is beneficial for many people, it can be challenging for those who are naturally introverted or prefer solitude. Being around groups of people regularly might feel overwhelming or uncomfortable for some participants.
Transportation schedules and center activities operate on set routines that might not match your loved one’s natural preferences. Someone who has always been a night owl might struggle with morning pickup times, or someone who values quiet time might find the center environment too stimulating.
Some participants initially resist the idea of receiving help with personal care or daily activities. The adjustment from independence to accepting assistance can be emotionally difficult and may require time and patience from both participants and families.
Enrolling in PACE means that your loved one must receive all healthcare through the PACE program. They cannot continue seeing their longtime family doctor or specialists outside the PACE network except in emergency situations or with special approval.
This limitation can be particularly difficult for people who have strong relationships with current healthcare providers. Leaving a trusted doctor who has provided care for years can feel like losing an important relationship and source of security.
Specialist care is provided through the PACE network, which might not include the specific specialists your loved one has been seeing. While PACE provides access to necessary specialty care, it might not be with the same providers your family prefers.
The network limitations also apply to hospitals and other healthcare facilities. PACE participants typically receive care at facilities that have contracts with the PACE program, which might not be the hospitals your family has used in the past.
Traditional Medicare provides medical coverage but doesn’t coordinate care or provide the comprehensive support services that help seniors remain safely at home. With traditional Medicare, families must arrange and coordinate multiple services separately, often resulting in gaps in care and confusion about coverage.
PACE offers more comprehensive coverage than traditional Medicare, including services like transportation, meals, personal care assistance, and social activities that Medicare doesn’t typically cover. However, PACE requires using only PACE providers, while traditional Medicare allows more choice in healthcare providers.
Nursing home care provides 24-hour supervision and comprehensive services, but requires leaving home and the community. While nursing homes can be appropriate for people who need constant medical supervision, PACE allows people with similar care needs to remain in their communities.
PACE typically costs less than nursing home care while providing many of the same services in a community setting. The social and emotional benefits of remaining at home often result in a better quality of life compared to institutional care.
Home health services provide limited assistance with medical care and daily activities, but don’t offer the comprehensive coordination and support that PACE provides. Home health is typically short-term and focused on specific medical needs, while PACE provides ongoing, comprehensive care.
PACE combines the medical benefits of nursing home care with the independence of home-based services, creating a unique option that addresses both safety needs and quality of life preferences.
PACE is often the right choice for families who want to keep their loved one at home but recognize that they need more support than traditional services can provide. If your loved one qualifies for nursing home care but strongly prefers to remain in their community, PACE might be the perfect solution.
The program works well for people who enjoy social interaction and would benefit from the companionship and activities available at PACE centers. If your loved one is isolated at home or would enjoy making new friends, the social aspect of PACE can be particularly valuable.
PACE is ideal for families who feel overwhelmed by coordinating multiple healthcare providers and services. If you’re struggling to manage appointments, medications, and various support services, PACE’s comprehensive coordination can provide significant relief.
The program especially benefits people with complex medical needs requiring frequent healthcare services. The comprehensive coverage and coordinated care can result in better health outcomes and fewer emergency situations.
PACE might be the right choice if your family is concerned about the unpredictable costs of healthcare and long-term care. The program’s comprehensive coverage and predictable monthly costs can provide financial peace of mind.
The Program of All-Inclusive Care for the Elderly (PACE) offers a unique solution for seniors who need nursing home-level care but want to remain in their communities. This comprehensive program brings together medical care, support services, and social activities under one coordinated system that puts the person at the center of all decisions.
PACE works by providing everything your loved one needs through one team of professionals who get to know them personally. Instead of juggling multiple doctors, insurance companies, and service providers, families work with one care team that coordinates all services—from medical appointments and medications to transportation and meals.
The program serves people who are 55 or older, live in a PACE service area, qualify for nursing home-level care, and can live safely in the community with support. For many participants, PACE is covered entirely by Medicare and Medicaid, making comprehensive care affordable for families with limited resources.
PACE centers serve as healthcare hubs where participants receive medical care, therapy services, nutritious meals, and social activities. The social connections formed at these centers often become one of the most valued aspects of the program, reducing isolation and providing companionship with peers who understand similar challenges.
The program’s strength lies in its flexibility and respect for individual choice. While PACE provides structure and comprehensive services, participants always maintain the right to make decisions about their care and can choose to leave the program at any time if it’s not meeting their needs.
PACE offers significant advantages over traditional care options, including comprehensive coverage without copayments, coordinated care that prevents gaps in services, and the ability to age in place while receiving professional support. The program often costs less than nursing home care while providing many of the same services in a community setting.
If you’re feeling overwhelmed by the challenges of caring for an aging loved one, you’re not alone. Many families struggle to balance ensuring safety and honoring their loved one’s desire to remain independent. PACE offers a path forward that addresses both of these crucial needs.
It’s natural to feel uncertain about making changes to your loved one’s care, especially when they’ve been managing with current arrangements. However, waiting until a crisis occurs often limits your options and can result in emergency decisions that don’t reflect your family’s preferences.
PACE is designed specifically for families facing the situation you’re in right now. The program was created by people who understood that seniors could receive excellent care while staying in their communities if the right support system existed. Thousands of families have found that PACE provides the comprehensive care their loved ones needed while preserving the dignity and independence they valued.
Remember that exploring PACE doesn’t commit you to anything. The assessment process is designed to help you understand whether the program would be a good fit for your family’s specific situation. Even if you decide that PACE isn’t right for you now, the information you gather can help you make more informed decisions about future care needs.
Many families find that PACE actually increases their loved one’s independence rather than restricting it. By providing comprehensive support and safety nets, the program often allows people to do more activities and maintain more control over their lives than they could manage without this support.
Trust your instincts about what’s best for your family. If your loved one values staying in their community, enjoys social interaction, and would benefit from coordinated care, PACE might be exactly what you’ve been looking for.
The first step is to find out if PACE is available in your area. Visit Medicare.gov and use their search tool to enter your zip code and find nearby PACE programs. You can also call Medicare at 1-800-MEDICARE for help locating programs in your area.
Once you’ve identified a local PACE program, call them directly to discuss your loved one’s situation. The staff can provide information about their specific services, answer questions about eligibility, and help you understand what the program would mean for your family.
Prepare for your initial conversation by gathering basic information about your loved one’s health conditions, current medications, and care needs. This will help the PACE staff determine whether an assessment might be appropriate and what services would be most relevant.
If the initial conversation suggests that PACE might be a good fit, schedule the comprehensive assessment. This evaluation typically takes place in your loved one’s home and provides the detailed information needed to determine eligibility and develop a care plan.
During the assessment process, don’t hesitate to ask questions about anything you don’t understand. This is your opportunity to learn about the program, understand what services would be provided, and determine whether PACE aligns with your family’s values and preferences.
If your loved one qualifies for PACE and you decide to move forward, the enrollment process will include orientation sessions that introduce you to the program’s services and staff. Take advantage of these sessions to build relationships with the care team and understand how the program will work for your specific situation.
Remember that you can take time to make this decision. While it’s important not to wait until a crisis occurs, you don’t have to rush into enrollment. Use the assessment and orientation process to gather the information you need to make a confident decision about your loved one’s care.
Consider involving your loved one in every step of this process. Their input and preferences are crucial to making the right decision, and their comfort with the program will significantly impact its success.
Finally, remember that choosing PACE is not a permanent decision. If you try the program and find that it’s not meeting your family’s needs, you can always explore other options. The goal is to find the care approach that provides the best quality of life for your loved one while giving your family peace of mind.
Taking the first step to explore PACE shows your commitment to finding the best possible care for your loved one. Whatever you decide, you’re approaching this important decision with the love, thoughtfulness, and dedication that your family member deserves.
The National PACE Association is the main organization representing all PACE programs across the country. It provides general information about PACE, helps families understand how the program works, and can direct you to local programs in your area.
You can contact the National PACE Association through their website or by phone to get basic information about PACE and find programs near you. They also provide educational materials that can help you understand whether PACE might be right for your family.
The association maintains a directory of all PACE programs nationwide, making it easy to find contact information for programs in your specific area. This directory includes addresses, phone numbers, and service areas for each program.
Each PACE program operates independently and serves a specific geographic area. Once you identify a program in your area, you’ll work directly with their staff for assessment, enrollment, and ongoing services.
Local PACE programs typically have intake coordinators who specialize in helping families understand the program and navigate the enrollment process. These staff members can answer questions about eligibility, services, costs, and what to expect during the assessment.
Most PACE programs have social workers on staff who can help families understand how PACE compares to other care options and whether the program would be appropriate for their specific situation. They can also provide information about other resources if PACE isn’t available or suitable.
Medicare customer service representatives can help you find PACE programs in your area and provide basic information about how PACE works with Medicare benefits. They can also help you understand how enrolling in PACE would affect your current Medicare coverage.
The Medicare helpline is available to answer questions about PACE eligibility, coverage, and costs. They can explain how PACE differs from traditional Medicare and help you understand what services would be covered.
The official Medicare website has a specific section dedicated to PACE that explains how the program works, who qualifies, and what services are covered. This is one of the most reliable sources of accurate, up-to-date information about PACE.
Medicare.gov includes a search tool that allows you to enter your zip code and find PACE programs in your area. The search results include contact information, service areas, and links to individual program websites.
The website also provides information about how PACE costs compare to other Medicare options and what you can expect to pay based on your insurance coverage. This can help you understand the financial aspects of PACE before you contact local programs.
Your state Medicaid office can provide information about PACE programs in your state and help you understand how Medicaid works with PACE services. They can also help determine whether your loved one might qualify for Medicaid benefits that could reduce PACE costs.
State Medicaid offices often have staff who specialize in long-term care options and can explain how PACE compares to other services available in your state. They may also have information about waiting lists or new programs being developed.
Area Agencies on Aging are local organizations that specialize in helping older adults and their families navigate available services and resources. They often have detailed knowledge about PACE programs and other care options in your community.
These agencies can provide information about PACE and help you understand how it fits into the broader range of services available for older adults in your area. They may also offer counseling services to help families make informed decisions about care options.
Area Agencies on Aging often provide free consultations to help families assess their needs and explore available options. This can be particularly helpful if you’re not sure whether PACE is the right choice or if you want to understand all available alternatives.
State health departments oversee PACE programs and ensure they meet quality standards. They can provide information about program oversight, quality measures, and how to file complaints if you have concerns about a PACE program.
Some state health departments maintain information about PACE program performance, including participant satisfaction surveys and quality indicators. This information can help you evaluate different programs if you have multiple options in your area.
Ask about the specific services included in the program and how they’re delivered. Find out what medical services are available on-site versus those that require transportation to other locations. Understanding the scope of services helps you determine whether the program can meet your loved one’s needs.
Inquire about the qualifications and experience of the care team members. Ask about the primary care physician, nursing staff, therapists, and other professionals who would be involved in your loved one’s care. Understanding who will provide care helps build confidence in the program.
Ask how the program handles emergencies and after-hours care. Find out what happens if your loved one needs medical attention outside of normal business hours and how the program coordinates with hospitals and emergency services.
Inquire about the program’s approach to medication management. Ask how medications are monitored, how the pharmacy services work, and what happens if your loved one needs medications that aren’t typically covered.
Ask about transportation services and how they work. Find out about pickup and drop-off times, what happens if your loved one is sick and can’t come to the center, and whether transportation is available for medical appointments outside the program.
Inquire about the daily schedule and activities at the PACE center. Ask about meal programs, social activities, and how the program accommodates different interests and abilities. Understanding the daily routine helps you determine whether your loved one would enjoy the experience.
Ask about the program’s policies regarding family involvement. Find out how families can stay informed about their loved one’s care, participate in care planning, and communicate with the care team.
Inquire about the program’s approach to individual preferences and choices. Ask how they accommodate dietary restrictions, cultural preferences, and personal routines. Understanding their flexibility helps determine whether the program would respect your loved one’s individuality.
Ask for a clear explanation of all costs associated with the program. Find out what the monthly premium would be based on your loved one’s insurance coverage and whether there are any additional fees for specific services.
Inquire about what happens if your loved one’s insurance situation changes. Ask about options if they lose Medicaid eligibility or if their Medicare coverage changes. Understanding these scenarios helps with long-term planning.
Ask about the program’s policies regarding private pay arrangements. If your loved one doesn’t qualify for Medicare or Medicaid coverage, find out what private pay options are available and what they would cost.
Ask about the program’s track record and outcomes for participants. Inquire about participant satisfaction, how long people typically stay in the program, and what happens when participants’ needs change significantly.
Ask about staff turnover and continuity of care. Find out how long key staff members have been with the program and what happens when staff members leave. Continuity of care is important for building relationships and maintaining quality.
Inquire about the program’s approach to quality improvement and how it handles complaints or concerns. Ask about its grievance process and how it works to continuously improve its services.
Ask for references from current participants or their families. Speaking with other families who have experience with the program can provide valuable insights that you won’t get from program staff alone.
Ask about the enrollment process timeline and what to expect during assessment and orientation. Find out how long the process typically takes and what information you’ll need to provide.
Inquire about how the program coordinates with your loved one’s current healthcare providers. Ask about transferring medical records, coordinating medications, and ensuring continuity of care during the transition.
Ask about the program’s policies regarding disenrollment. Find out what the process is if you decide PACE isn’t working for your family and what options are available for transitioning to other care arrangements.
Inquire about waiting lists and availability. Ask whether there’s currently space in the program or if you’ll need to wait, and find out what support is available while you’re waiting for enrollment.
These questions will help you gather the information needed to make an informed decision about whether PACE is right for your family. Remember that choosing a care program is an important decision that affects your loved one’s daily life and well-being. Take the time to ask questions, visit the program, and ensure you feel comfortable with the care team and services before making a commitment.
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
Remember that there is currently no official accrediting body for end-of-life doula programs. Certification only means one graduated from a program. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.