Tag: Mottling
Articles about mottling on the terminally ill person’s body and the significance of mottling at the end-of-life.
Articles about mottling on the terminally ill person’s body and the significance of mottling at the end-of-life.
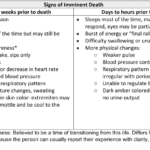
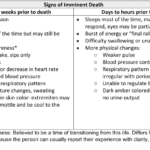
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.

As a caregiver or family member, it can be challenging to witness the changes that occur as a loved one approaches the end of their life. One such change that may occur is mottled skin, also known as livedo reticularis. Understanding what mottled skin is and its significance in the dying process can help you provide the best care and support to your loved one during this time.
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
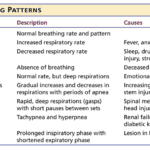
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.

There are observation and interviewing skills you can develop which will help you learn:
What could cause the current change in condition
Determining if a patient is having terminal restlessness
Determining if your patient is within two weeks or less of life to live
Knowing where your patient is in the dying process
While this article is primarily meant for new nurses, what I’m sharing is also valuable for family members and loved ones. Anyone with patience and love toward the person being observed and interviewed can hone and develop these skills.

The dying process involves physical and emotional changes as the body shuts down. As the heart weakens, circulation slows, leading to cold hands and feet, pale skin, and drowsiness. Breathing becomes irregular and shallow. The patient may experience delirium or visions. Providing comfort through pain management, emotional support, and spiritual care is crucial.

When I first started working in the field of hospice, my clinical manager told me (I’m paraphrasing), one day you will be able to walk into the room, and without getting a single vital sign, just by visual observation, be able to tell that the person is dying or will be shortly dying. That was about three years ago. Today, it’s almost chilling for me (as it is both a blessing and tremendous responsibility) to be able to share she told the truth, and that over time — if you give yourself patience and grace and take the time to listen, observe, and remember — you too will learn how to tell when someone is close to or otherwise is dying.
Please allow me to share some of my insight as to how I know a person has less than a month left to live, and often far less. First off, let’s go into the important discussion you should have with the family, friends, and the patient themselves that provides an overall background to the prognosis. That discussion should be centered around what types of decline (downward, negative) changes have been taking place in the patient’s life over the last six months making note as to whether the decline is minor, medium, or major and the frequency (once a month, once a week, etc.) of those changes.