Sleeping as a Prognostication Tool for the Terminally Ill

Sleep patterns can help estimate how close a terminally ill person is to dying. Learn how changes in sleep can indicate approaching death and how to support your loved one during this time.
The Final Journey: Understanding Why the Actively Dying May Linger

Explore the profound journey of the actively dying. This article unravels the reasons behind their lingering, examining medical interventions and the emotional need for closure. Gain insight into this delicate phase of life."
Understanding Changes in Palliative Performance Scale in the Last Six Months of Life
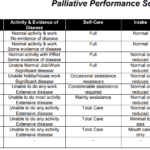
Explore the Palliative Performance Scale (PPS) and its crucial role in end-of-life care. Learn how this tool helps hospice professionals assess patient decline, predict life expectancy, and provide tailored care. Understand the significance of PPS changes in the final six months and how they guide compassionate care decisions.
Significant Signs a Terminally Ill Patient may be Close to Dying
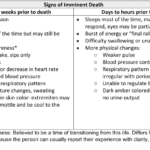
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.
Understanding Functional Decline in the Natural Dying Process
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.
Trigger Words for Hospice Nurses: Assessing End-of-Life in Two Weeks or Less
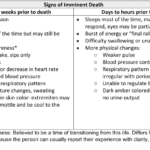
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
Breathing Patterns Before End of Life: Critical Clues for the Last Hours!
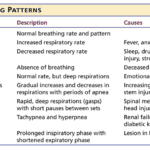
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.
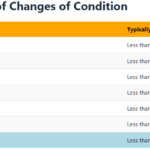
Frequency of Changes in Condition as an Indicator of Approaching Death

Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.
The Dying Process at the End of Life

The dying process involves physical and emotional changes as the body shuts down. As the heart weakens, circulation slows, leading to cold hands and feet, pale skin, and drowsiness. Breathing becomes irregular and shallow. The patient may experience delirium or visions. Providing comfort through pain management, emotional support, and spiritual care is crucial.