Tag: Hospice Services
Articles about the services offered by hospice providers.
Articles about the services offered by hospice providers.

This position involves being the first point of contact for families, patients, and facilities, making a lasting impression by offering both compassion and confidence in explaining hospice services. In this discussion, we will delve into the various aspects of the role of the Hospice Liaison, bringing insight from forever Christmas-loving Kathy Naccarato, including its dynamic nature, your dedication to dispelling misconceptions, and the importance of building relationships within the healthcare community.
If your loved one has been diagnosed with Vascular Dementia, it is natural to have questions and concerns about what lies ahead. This educational article aims to provide you with an overview of what to expect over the course of the disease, the changes you might see in your loved one, and how to best care for them from onset until the end of life.

Hospice care is often misunderstood and shrouded in myths that can prevent individuals and families from accessing the compassionate support they need during a challenging time. This article will address common misconceptions about hospice care and provide you with the facts. We aim to empower you with accurate information to make informed decisions when considering hospice for yourself or a loved one.
Caring for a loved one with dementia can be a rewarding experience, but it can also be physically, emotionally, and mentally exhausting. Family caregivers often neglect their own well-being while focusing on the needs of their loved ones, leading to burnout. Caregiver burnout is a state of physical, emotional, and mental exhaustion that can happen when caregivers don't get the help they need or try to do more than they are able to do. In this article, we will discuss how family caregivers of a loved one with dementia can avoid burnout and recover if they are already experiencing burnout.

In this article, we will explore the vital role of a hospice chaplain, as explained by Katherine Seiler, an experienced and compassionate hospice chaplain. Hospice chaplains play a significant role in providing emotional, social, and spiritual support to terminally ill patients and their families during their end-of-life journey.

In the realm of hospice care, compassion and comfort take precedence. A team of skilled professionals comes together to offer comprehensive support to patients, their families, and caregivers. Among these essential contributors, Certified Nursing Assistants (CNAs) stand out as unsung heroes, bringing immeasurable value to the field of hospice care. This article delves into the distinctive role CNAs play in hospice, their frequent and meaningful interactions, and their leadership within the hospice team.
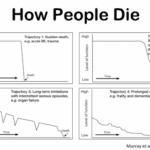
Is it Too Early to Start Hospice?
It's crucial to remember that hospice care is about improving the quality of life for the patient and their family, regardless of the time left. Hospice care can be initiated when the patient's condition is declining and they require comfort-focused care rather than life-prolonging treatments. Starting hospice care early can provide ample time for the patient and their family to benefit from the support and services offered.
If you're unsure when to consider hospice care, consult the patient's primary physician or a hospice care provider. They can guide you through the process and help you make an informed decision based on the patient's needs and circumstances.

Caring for a terminally ill loved one can be challenging. Still, with the proper support and understanding, you can help ensure they experience a comfortable and dignified end of life. Hospice care offers specialized medical and emotional support during this time. This guide aims to empower families new to hospice services by providing essential information on what to expect from a hospice provider and how to manage the journey towards a good death.
I understand the challenges that patients and families face when receiving hospice services. One common issue that arises is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can play a crucial role in reducing after-hour calls and providing better support to patients and their families. Here’s how:

Hospice care offers a specialized service known as the Continuous Care Benefit. This unique care type provides crucial 24-hour support to patients who are going through an acute symptom crisis. In this article, we'll delve into what Continuous Care Benefit is, who's eligible for it, how it operates, why it's important, how to access it, and its duration.
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.

This short article is meant for hospice patients, family members, and friends.
It’s common to read various social media posts where a patient, family member, or friend does the right thing by calling their hospice provider to alert them of a change of condition or otherwise significant issue for on-call to come out for an unscheduled visit. Also, common is follow up posts where the writer asked, “it’s been ______ (minutes, hours) since the call, I hope they show up.”
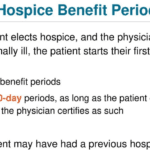
There are several things that go on behind the scenes when you or your loved one is admitted to a hospice provider. Some of them you may never see because it doesn’t impact the care provided and received. Others like the hospice benefit periods may only come out of the woodwork (so to write) at certain times and can either cause joy or distress depending on one’s point of view.
The goal of this article is to keep it simple and smile (my version of the K.I.S.S. principal) understanding of hospice benefit periods. When a person is first admitted to a hospice provider (having never been on hospice), they start off (behind the scenes) in benefit period number one. This is the first half (90-days/3-months) of the estimated six-months or less to live. Benefit period number two is the second half (3 more months/90-days). And since a terminal illness doesn’t come with guarantees that one will pass in six months or less, Medicare allows for (with fine print through the entire journey) an unlimited number of sixty-day (two months at a time) benefit periods.
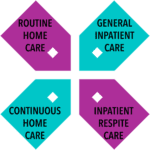
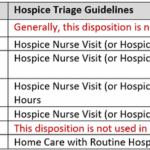
This article is meant to help families and new hospice staff understand the four hospice care levels. According to Medicare guidelines, several levels of care govern hospice services in the United States of America, whether the patient uses Medicare or not.

Hospice care is a vital service that provides compassionate and specialized support to individuals with life-limiting illnesses, particularly when they receive care at home. Understanding what home hospice covers is essential for patients and their families to ensure comprehensive and personalized end-of-life care. This article aims to shed light on the various aspects of home hospice care, including medications, durable medical equipment, staffing support, and expertise in managing the natural dying process. By delving into these details, individuals can make informed decisions and better comprehend the valuable assistance hospice care provides during this sensitive time.
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it's readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor's orders, care plans, documentation, and education. We'll conclude with two real-life cases to illustrate these points.

A hospice house is a peaceful, home-like residence where terminally ill people receive short-term hospice care. It is designed to provide a setting as close to home as possible, allowing for more freedom than a traditional facility. Hospice houses are typically run by not-for-profit organizations and are financed by donations, making them more economical for families who cannot afford skilled nursing facilities. Unlike inpatient hospice units (IPUs), hospice houses work with several hospice providers, allowing families to choose the provider that best suits their needs. They also follow a more flexible visitation policy, allowing families to visit 24x7 without appointments.