Tag: End Of Life Symptoms
Article about common end-of-life symptoms of the terminally ill.
Article about common end-of-life symptoms of the terminally ill.
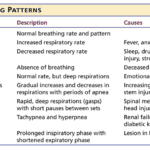
Understanding breathing patterns in end-of-life care is crucial for providing comfort to your loved one. Learn about regular vs. irregular breathing rhythms and when to contact hospice for additional support.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.

Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.
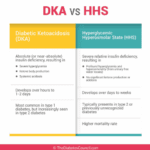
As an experienced hospice nurse, I understand that managing diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) at end of life can be challenging, especially when patients choose to stop taking their diabetic medications or when those medications are no longer an option. In this article, I will provide information on recognizing the signs and symptoms of hyperglycemic crises and outline comfort-based treatment options that align with hospice goals of care.
Caring for a comatose loved one during their hospice journey requires special attention, particularly when it comes to oral care. In this guide, we'll explore best practices for oral care, considering the unique needs of comatose patients, and provide you with valuable resources for further guidance.
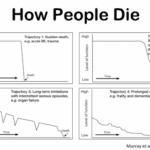
Explore the journey through terminal illness, understanding key signs and symptoms at each stage. This guide offers insight into the physical and emotional changes as life nears its end, helping caregivers provide compassionate support.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.

Witnessing a loved one nearing the end of life can be challenging and emotional for a caregiver. One symptom you may encounter during this time is the death rattle. Understanding what the death rattle is, how to recognize it, and how to manage its symptoms can help you provide comfort and support to your loved one in their final days. This guide will explore the death rattle, its significance, and practical tips for managing it.
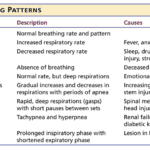
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.

I have cared for many terminally ill patients over the years. One question that comes up frequently is should the dying patient be on oxygen at the end of life?
I see it from both sides, from hospice intake personnel as well as the admitting nurse — all had it drilled into them over the years that low oxygen saturation must be treated — to families who see how hospital and nursing home staff rush to put someone on oxygen because of low oxygen saturation.
Contrary to widespread belief, most dying patients do not need oxygen. Here’s why:
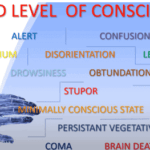
Understanding drowsiness, lethargy, and obtundation is crucial in hospice care. Drowsiness is a normal sleepiness, lethargy is more profound tiredness, and obtundation indicates severe unresponsiveness. Recognizing these levels helps in providing the right care and comfort for terminally ill patients.

Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives - Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.
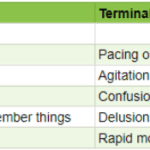
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.
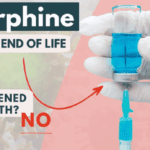
As a hospice nurse with years of experience, I have encountered many situations where family members are hesitant to allow their loved ones to receive medications such as morphine and lorazepam. One of the main reasons for this hesitancy is the belief that these medications will hasten death, leading to euthanasia.
In this article, I want to address this concern and help family members and friends understand the use of morphine and lorazepam in hospice care.
Hey there, my friend! As an experienced hospice nurse, I understand that managing symptoms for comfort is crucial for terminally ill patients. One of the ways we do this is through PRN medications. Today, I want to help you understand PRN medications and how they can be used in conjunction with scheduled medications.
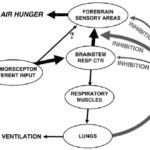
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen.
Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference).

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.