Supporting Your Loved One with Multiple Myeloma: A Guide to Compassionate Care From Diagnosis Through End-of-Life
Published on December 19, 2025
Updated on December 19, 2025
Published on December 19, 2025
Updated on December 19, 2025
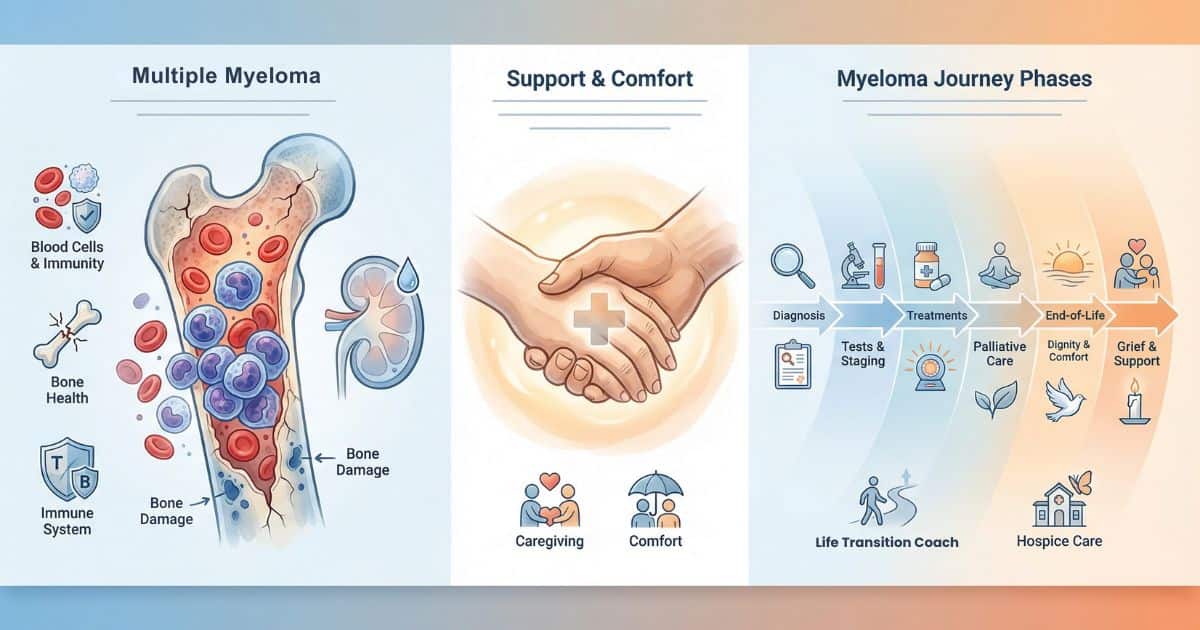
Table of Contents
Hearing the words Multiple Myeloma can feel like the ground has shifted under your feet. This guide is here to help you understand what is happening, what to expect, and how to support your loved one and yourself with as much comfort and dignity as possible.
Multiple Myeloma is a blood cancer that starts in the bone marrow when certain white blood cells, called plasma cells, grow out of control. These abnormal cells crowd out healthy cells and can damage bones, kidneys, and the immune system. This article walks with you from diagnosis to end-of-life, explaining tests, staging, survival estimates, palliative care, caregiving, hospice, and how a Health and Life Navigation Specialist can help your family navigate illness and grief.
Diagnosis usually starts when something “doesn’t look right,” such as anemia, bone pain, kidney problems, or frequent infections. Your loved one’s healthcare team may order blood and urine tests, then more specialized tests to confirm Multiple Myeloma.
Think of the diagnostic process like putting together a puzzle: each test is one piece. When enough pieces are in place, the picture becomes clear, and the team can explain what is going on and what comes next.
Blood and urine tests look for:
A bone marrow biopsy is a key test. The doctor numbs the area, usually at the back of the hip, and removes a small marrow sample with a needle. Many families compare it to “a few minutes of intense discomfort to get answers that guide the whole treatment plan.”
Imaging tests—such as X‑rays, MRI, or PET scans—look for weak spots or “holes” in the bones caused by Myeloma cells. You can picture these abnormal cells as weeds in a garden: imaging shows where the weeds have spread, so the team knows where to focus care.
You have the right to clear explanations. Consider asking:
Writing down your questions and bringing a notebook to each visit can help you feel more in control. Many families find it helpful to have a second person listening, so more details are remembered, and emotions feel less overwhelming.
Multiple Myeloma is commonly staged using the Revised International Staging System (R‑ISS). Instead of measuring tumor size, this system looks at:
You can think of staging as a way to group patients by overall risk, not as a simple countdown clock.
In simple terms:
Staging helps the team decide how aggressive treatment should be. For example, a younger, otherwise healthy person with Stage II or III may be offered strong combination therapy and possibly a stem cell transplant. Someone older or more fragile may receive a gentler regimen with a strong focus on comfort and function.
Staging guides:
It is vital to remember that staging is not a death sentence. It is a planning tool. Two people with the same stage can have very different experiences based on age, other illnesses, response to treatment, and personal goals.
Survival statistics can be scary, but they are only averages—not a prediction of any one person’s life. Current data show that about 62% of people with Myeloma in the United States are alive 5 years after diagnosis overall. For a disease that is still localized at diagnosis, 5‑year survival is around 80.7%, while for a more advanced disease, it is about 61.7%.
These numbers reflect large groups of patients and include people of all ages and with many health conditions.
With modern treatments—such as proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies, and stem cell transplant—many patients live significantly longer than in the past, and some achieve long‑lasting remissions. Without treatment, Myeloma usually progresses faster, causing more pain, infections, and organ damage.
Treatment does not always mean harsh chemotherapy. For some, it may be lower‑intensity regimens focused on controlling disease while preserving quality of life.
Every person’s path is unique. Survival depends on:
This is why two people diagnosed the same year with the same stage can have very different experiences.
The good news is that survival rates have improved steadily over the last two decades, thanks to newer therapies and better supportive care. Many people live for years with Myeloma as a chronic condition, primarily when symptoms are well managed.
Quality of life can include:
Your loved one’s care team and palliative support can help protect this quality of life at every stage.
Palliative care is comfort‑focused care that can be added at any stage of a serious illness. It works alongside cancer treatment to manage symptoms, support decision‑making, and care for emotional and spiritual needs.
A helpful image is this: palliative care is like adding support beams to a house while it’s still being built. It strengthens the entire structure, allowing it to carry more weight.
Research in blood cancers, including Multiple Myeloma, shows that early palliative care is both feasible and beneficial. It does not require stopping chemotherapy or other disease‑directed treatments. In fact, many patients start palliative care near the time of diagnosis or early in their treatment course.
Starting early means:
Palliative providers work as part of the team with oncologists and hematologists. While the cancer team focuses on controlling Myeloma, palliative care focuses on:
Patients receiving palliative care often have fewer emergency visits, better symptom control, and greater peace of mind regarding complex decisions.
Palliative care may offer:
Many families find that palliative care gives them “permission” to focus on comfort and connection, even while still hoping that treatment will control the cancer.
Caring for someone with Myeloma is a marathon, not a sprint. Your role as caregiver is vital, and your needs matter too.
In the early stages, your loved one may still feel pretty well. You can help by:
Simple actions, like keeping a shared calendar for labs and visits, help reduce stress and miscommunication.
During active treatment, fatigue, nausea, infections, or bone pain may increase. As a caregiver, you can:
Many caregivers find it helpful to make a “helping list” so others can pitch in with meals, rides, or errands.
As the disease advances or relapses, goals may shift more toward comfort and meaningful time together. You can:
Caregiver support is essential at this stage. Depression, burnout, and complicated grief are more common when caregivers don’t get help. Reaching out to a counselor, support group, or a Health and Life Navigation Specialist can protect both you and your loved one.
Hospice is usually considered when a person is thought to be in the last six months of life if the disease continues its usual course. In Multiple Myeloma, signs may include:
These signs suggest that focusing on comfort and support may bring more benefit than continuing aggressive treatment.
Hospice is specialized care for people nearing the end of life, focused on comfort, dignity, and quality of time rather than a cure. It can be provided at home, in hospice facilities, or in some nursing homes.
Hospice teams often include:
They manage pain and other symptoms, support family caregivers, and help with emotional, spiritual, and practical needs.
Many families fear that hospice means “giving up” or that death will come immediately. In reality, entering hospice does not cause death, and in some illnesses, hospice enrollment is associated with equal or even longer survival and better comfort.
It is essential to know:
Starting hospice when your loved one is first eligible—around the six‑month mark—offers:
Families often say they wish they had started hospice sooner, once they see the level of support it provides.
When hospice is called in only in the last days or week of life, the focus often shifts to crisis management rather than thoughtful planning. This can mean:
Waiting until your loved one is actively dying can rob everyone of the chance to use hospice fully—for teaching, emotional support, and gentle closure.
Early hospice enrollment is best understood as extending a well‑lived time, not shortening life. It allows comfort, connection, and dignity to be the priority for as long as possible.
Remember:
These conversations can guide you toward a timing that honors both medical reality and your family’s values.
A Health and Life Navigation Specialist specializes in walking alongside individuals and families during significant life changes, including serious illness. This person can help you:
Think of a Health and Life Navigation Specialist as a kind, skilled guide who helps you find your footing on unfamiliar ground.
Anticipatory grief is the sadness and worry you feel before a loss happens. A Health and Life Navigation Specialist can:
After a death, the same coach can support post‑loss adjustment, helping survivors rebuild daily life and find meaning in their loved one’s memory.
Between the medical team, palliative care, hospice, and a Health and Life Navigation Specialist, your family can be held by a circle of support. You are not expected to “be strong” without help. Reaching out is an act of wisdom and love—for your loved one and for yourself.
If your loved one has Multiple Myeloma and is not yet receiving palliative care, consider making this your next conversation. Ask the oncologist or hematologist:
If your loved one is declining and you wonder about hospice, it is okay to say, “I’m noticing big changes. Is it time to talk about hospice options?” Early, honest conversations do not take away hope—they refocus hope on comfort, connection, and peace.
Your action steps might include:
You and your family deserve quality time together, comfort, and dignity at every stage of this journey. Asking for help—early and often—is one of the most loving choices you can make.
International Multiple Myeloma Foundation
Epidemiology, Staging, and Management of Multiple Myeloma
Survival Rates for Multiple Myeloma
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
Remember that there is currently no official accrediting body for end-of-life doula programs. Certification only means one graduated from a program. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series