Navigating Swallowing Challenges in Dementia: A Comprehensive Guide
Published on June 30, 2025
Updated on June 30, 2025
Published on June 30, 2025
Updated on June 30, 2025
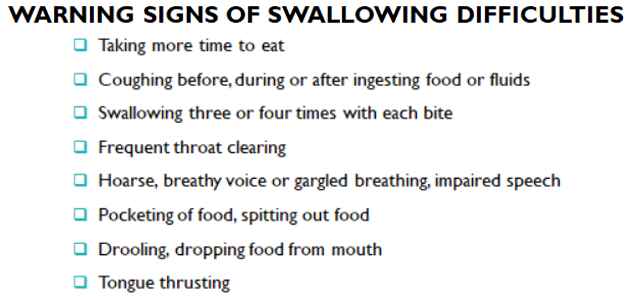
Table of Contents
Caring for a loved one with dementia can be challenging, especially when they develop swallowing problems, also known as dysphagia. This guide aims to help you understand these issues and provide practical advice for managing them. Remember, you’re not alone in this journey, and with the correct information and support, you can make a significant difference in your loved one’s quality of life.
Dementia is not a single disease but a term that describes symptoms affecting memory, thinking, and social abilities. It’s essential to recognize that dementia encompasses more than just occasional forgetfulness.
Key points about dementia:
Common symptoms of dementia include:
| Stage of Dementia | Typical Symptoms | Care Needs |
|---|---|---|
| Early | Forgetfulness, slight confusion | Minimal assistance, reminders |
| Middle | Increased memory loss, difficulty with daily tasks | Regular supervision, help with personal care |
| Late | Severe memory loss, physical decline | Full-time care, specialized support |
As dementia progresses, it can affect various parts of the brain, including those responsible for swallowing. This connection is crucial because swallowing problems can lead to serious health issues if not properly managed.
Here’s how dementia can affect swallowing:
It’s essential to note that swallowing problems can develop gradually, and their signs may initially be subtle. As a caregiver, being aware of this connection can help you spot potential issues early and seek appropriate help.
Common swallowing problems in dementia patients include:
Remember, every person with dementia is unique, and swallowing problems may manifest differently for each individual. Your attentiveness and care can make a significant difference in managing these challenges and ensuring your loved one’s comfort and safety.
As a caregiver or family member, you play a crucial role in identifying swallowing problems in your loved one with dementia. Awareness of the signs can help you seek timely medical attention and prevent serious complications.
Watch for these signs that may indicate your loved one is having trouble swallowing:
Remember, these symptoms may develop gradually, so stay vigilant and trust your instincts if you notice changes in your loved one’s eating habits.
Understanding the risk factors and potential complications of dysphagia can help you provide better care and know when to seek medical help.
Risk factors for developing swallowing difficulties in dementia patients include:
| Complication | Description | Warning Signs |
|---|---|---|
| Aspiration pneumonia | Infection caused by food or liquid entering the lungs | Fever, chest pain, difficulty breathing |
| Malnutrition | Inadequate nutrition due to reduced food intake | Significant weight loss, weakness, fatigue |
| Dehydration | Insufficient fluid intake | Dry mouth, dark urine, and confusion |
| Choking | Food blocking the airway | Inability to speak, blue lips or skin, panic |
If you notice any of these complications, seek immediate medical attention.
To help prevent these complications:
Remember, your attentiveness and care can make a significant difference in managing swallowing difficulties and ensuring your loved one’s comfort and safety. Don’t hesitate to contact healthcare professionals for support and guidance as you navigate this challenging aspect of dementia care.
Caring for a loved one with dementia involves understanding how the disease affects their nutrition and overall quality of life. Swallowing difficulties, or dysphagia, can significantly impact their ability to eat and drink, leading to various health challenges.
People with dementia often face numerous nutritional challenges due to their swallowing difficulties. These challenges can lead to malnutrition, dehydration, and a decline in overall health.
| Nutritional Challenge | Description | Tips for Management |
|---|---|---|
| Poor Appetite | Reduced interest in food | Offer favorite foods, small, frequent meals |
| Difficulty Chewing/Swallowing | Struggle with eating | Provide soft, easy-to-chew foods |
| Changes in Taste/Smell | Altered food preferences | Experiment with different flavors |
| Coordination Issues | Trouble using utensils | Use adaptive utensils, offer finger foods |
| Constipation | Discomfort from bowel issues | Ensure adequate hydration, high-fiber foods |
It’s common for caregivers to worry that their loved one with dementia is starving themselves. However, as dementia progresses, the brain’s ability to recognize hunger and thirst diminishes. In the later stages, the brain’s function for food and thirst may shut down completely.
Key Points to Understand:
Many caregivers fear that their loved one suffers from reduced food and fluid intake. However, with proper care and attention, you can help manage their symptoms and ensure they remain comfortable.
Important Considerations:
Dysphagia and nutritional challenges can also have psychological and social effects on individuals with dementia. Understanding these effects can help you offer more effective emotional and social support.
| Psychological Effect | Description | Tips for Management |
|---|---|---|
| Frustration/Anxiety | Stress from eating difficulties | Offer reassurance, create a calm environment |
| Depression | Sadness from reduced intake | Engage in enjoyable activities, seek professional help |
| Loss of Independence | Needing help with meals | Encourage participation in meal preparation |
| Social Effect | Description | Tips for Management |
|---|---|---|
| Isolation | Avoiding social meals | Encourage social interaction, and adapt mealtime settings |
| Changes in Mealtime Dynamics | Altered family traditions | Maintain a positive atmosphere, and include your loved one in conversations |
Understanding and addressing these psychological and social effects can help improve your loved one’s quality of life and emotional well-being. Remember, your support and empathy make a significant difference in their journey with dementia.
As a caregiver, understanding the diagnosis and assessment process for swallowing difficulties in patients with dementia can help you provide better support to your loved one. Early detection and proper evaluation are crucial for managing dysphagia effectively.
When you notice signs of swallowing problems in your loved one with dementia, their healthcare provider will typically start with a thorough medical evaluation. This process usually includes:
Remember, your observations are valuable. Be prepared to share any changes you’ve noticed in your loved one’s eating habits or specific incidents related to swallowing difficulties.
The doctor may recommend specialized tests if the medical evaluation suggests swallowing problems. These tests help determine the exact nature and severity of the swallowing difficulty.
| Test | Description | What to Expect |
|---|---|---|
| Barium Swallow Study | X-ray exam of the swallowing process | Your loved one will swallow barium-coated foods and liquids while being X-rayed |
| Endoscopy | Visual examination of the throat and esophagus | A thin, flexible tube with a camera is passed down the throat |
| FEES (Fiber-optic Endoscopic Evaluation of Swallowing) | Examines swallowing function | A small camera is inserted through the nose to observe swallowing |
| Manometry | Measures muscle contractions in the esophagus | A thin tube is inserted into the esophagus to measure pressure |
What you can do to prepare:
After the tests:
Remember, these tests are crucial for developing an effective care plan. Your support and understanding during this process can significantly affect your loved one’s comfort and well-being.
As a caregiver, it’s normal to feel overwhelmed by the medical processes. Don’t hesitate to ask questions or seek clarification from the healthcare team. Your active involvement is essential in ensuring the best care for your loved one with dementia and swallowing difficulties.
Managing dysphagia in dementia patients involves a combination of dietary modifications, swallowing techniques, and mealtime assistance. These strategies aim to ensure safety, improve nutrition, and enhance the quality of life for your loved one.
Modifying the consistency of food and fluids is a common strategy to help with swallowing difficulties. This can make eating safer and more comfortable for your loved one.
Soft Foods: These are easier to chew and swallow.
Pureed Foods: These have a smooth texture and are easier to swallow.
Thickened Liquids: These reduce the risk of aspiration.
Tips for Preparing Soft Foods:
Foods to Avoid:
| Food Group | Safe Options | Foods to Avoid |
|---|---|---|
| Dairy | Yogurt, custard, pudding | Hard cheese, yogurt with chunks |
| Fruits | Applesauce, ripe bananas | Pineapple, dried fruits |
| Vegetables | Mashed potatoes, steamed carrots | Raw vegetables, corn |
| Proteins | Scrambled eggs, pureed meats | Tough meats, nuts |
Swallowing exercises can help strengthen the muscles involved in swallowing and improve coordination. These exercises should be done under the guidance of a healthcare professional, such as a speech-language pathologist.
Effortful Swallow:
Dynamic Shaker:
Masako Maneuver:
Mendelsohn Maneuver:
Supraglottic Maneuver:
Safety Considerations:
Providing the proper support during mealtime can help prevent choking and aspiration, ensuring your loved one receives adequate nutrition.
Proper Positioning:
Small Bites and Sips:
Supervised Eating:
Adaptive Utensils:
Calm Environment:
| Assistance Strategy | Description | Tips for Implementation |
|---|---|---|
| Proper Positioning | Sit upright during and after meals | Use supportive chairs, avoid reclining |
| Small Bites and Sips | Take small amounts of food and drink | Cut food into small pieces, use small utensils |
| Supervised Eating | Monitor for swallowing difficulties | Stay present, offer encouragement |
| Adaptive Utensils | Use specially designed utensils | Try weighted forks, cups with lids |
| Calm Environment | Reduce distractions during meals | Play soft music, maintain routines |
By incorporating these management strategies, you can help ensure your loved one with dementia and dysphagia eats safely and comfortably. Your attentiveness and care are crucial in maintaining their health and quality of life.
Caring for a loved one with dementia and swallowing difficulties can be challenging, but there are several treatment options available to help manage these issues. Working closely with healthcare professionals to determine the best approach for your loved one’s needs is essential.
Medications can play a crucial role in managing dementia symptoms and swallowing difficulties. However, they require careful consideration and monitoring.
Key points about medications:
| Medication Consideration | Description | Action |
|---|---|---|
| Review current medications | Some may affect swallowing | Consult with the doctor for potential adjustments |
| Alternative forms | Options for easier swallowing | Ask about liquids, dissolvable tablets, or patches |
| Timing | Some drugs need specific timing | Follow the doctor’s instructions carefully |
| Crushing medications | Can alter drug effectiveness | Always consult a professional before crushing |
Various therapy approaches can help improve swallowing function and overall quality of life for individuals with dementia and dysphagia.
Common therapy approaches include:
Speech and Language Therapy:
Occupational Therapy:
Physical Therapy:
Nutritional Therapy:
Remember: Consistency in applying these therapies is key to their effectiveness. Your support and encouragement can have a significant impact on your loved one’s progress.
Adaptive equipment can significantly enhance independence and safety during meals for individuals with dementia and swallowing difficulties. These tools are designed to make eating and drinking more manageable and more comfortable.
Here are some helpful adaptive tools:
Utensils:
Plates and Bowls:
Drinking Aids:
Positioning Aids:
| Type of Equipment | Examples | Benefits |
|---|---|---|
| Utensils | Weighted forks, spoons with handcuffs | Improved control and grip |
| Plates and Bowls | High-sided plates, non-slip bottoms | Reduced spills, easier eating |
| Drinking Aids | Two-handled cups, dysphagia cups | Easier grip, controlled liquid intake |
| Positioning Aids | Cushions, non-slip placemats | Better posture, stable eating surface |
When choosing adaptive equipment:
By combining appropriate medications, therapy approaches, and adaptive equipment, you can help your loved one with dementia and swallowing difficulties maintain better nutrition, safety, and quality of life. Remember, your support and understanding are invaluable throughout this process.
Caring for a loved one with dementia and swallowing difficulties can be challenging, but you’re not alone. Proper support and education can make a significant difference in both your life and the life of your loved one.
Learning safe feeding practices is crucial for ensuring your loved one’s health and comfort. Here are some key areas to focus on:
Proper Positioning:
Food Preparation:
Feeding Techniques:
Recognizing Difficulties:
| Safe Feeding Practice | Description | Why It’s Important |
|---|---|---|
| Proper Positioning | Sit upright at 90 degrees | Reduces risk of choking and aspiration |
| Food Preparation | Soft, moist, small pieces | Easier to chew and swallow |
| Feeding Techniques | Small bites, allow time | Prevents overwhelming the person |
| Recognizing Difficulties | Watch for coughing, choking | Enables quick response to problems |
Always consult healthcare professionals, such as speech or occupational therapists, for personalized guidance on safe feeding practices.
Caring for someone with dementia and swallowing difficulties can be emotionally taxing. It’s crucial to take care of your emotional well-being. Here are some strategies:
Join Support Groups:
Practice Self-Care:
Seek Professional Help:
Educate Yourself:
Ask for Help:
Emotional Support Resources for Caregivers:
Remember: Your emotional well-being is just as important as the physical care you provide. You’ll be better equipped to care for your loved one by taking care of yourself.
Caring for someone with dementia and swallowing difficulties is a journey, and it’s okay to have ups and downs. Your dedication and love make a significant difference in your loved one’s life. Stay informed, seek support when needed, and be kind to yourself throughout this challenging but essential role.
When caring for a loved one with advanced dementia, you may face difficult decisions about their care, especially regarding nutrition and end-of-life choices. It’s essential to approach these decisions compassionately, keeping your loved one’s best interests and quality of life at the forefront.
Feeding tubes, such as percutaneous endoscopic gastrostomy (PEG) tubes, are often considered for patients with difficulty swallowing. However, for individuals with advanced dementia, feeding tubes are generally not recommended. Here’s why:
| Consideration | Feeding Tubes | Alternative Approaches |
|---|---|---|
| Comfort | May cause distress | Focus on comfort feeding |
| Quality of Life | Limited improvement | Emphasis on personal care and comfort |
| Medical Risks | Infections, complications | Reduced risk of medical interventions |
| Family Involvement | Less hands-on care | More opportunities for personal connection |
Remember: Choosing not to use a feeding tube is not the same as choosing to let your loved one go hungry. Alternative approaches focus on comfort and quality of life.
Making decisions about end-of-life care for a loved one with dementia can be emotionally challenging. Here are some guidelines to help you through this process:
Key Factors in Decision-Making:
Remember: There’s no one-size-fits-all approach. Each decision should be based on your loved one’s unique situation and what you believe they would want.
Instead of feeding tubes, many healthcare professionals recommend “comfort feeding” for individuals with advanced dementia. This approach involves:
Benefits of Comfort Feeding:
Making these decisions is never easy, but remember you’re doing your best to honor your loved one’s dignity and wishes. Don’t hesitate to seek support for yourself during this challenging time, whether from support groups, counselors, or your healthcare provider.
Caring for a loved one with dementia and swallowing difficulties can be challenging, but your dedication makes a world of difference. As we wrap up this guide, let’s recap the key points and offer encouragement to help you continue your caregiving journey.
Understanding Dementia and Dysphagia:
Recognizing Symptoms:
Management Strategies:
Treatment Options:
Caregiver Support:
Ethical Considerations:
Future Directions:
| Aspect of Care | Key Takeaway |
|---|---|
| Symptoms | Early detection is crucial |
| Management | Food modification and safe feeding practices are essential |
| Treatment | Work closely with healthcare professionals |
| Caregiver Support | Seek training and emotional support |
| Decision Making | Prioritize comfort and quality of life |
| Future Care | Stay informed about new developments |
Your role as a caregiver is invaluable, and your efforts make a significant difference in your loved one’s life. Here are some words of encouragement to keep you going:
Remember: Caregiving is a journey; taking it one day at a time is okay. Your efforts to provide comfort, maintain dignity, and ensure the best possible quality of life for your loved one are truly admirable.
As you continue on this path, know that you’re not just a caregiver—you’re a source of comfort, an advocate, and a beacon of love for your family member. Your dedication and compassion are making a profound difference in their life journey.
Stay informed, seek support when needed, and remember the importance of self-care at all times. You’re doing an incredible job, and your loved one is fortunate to have you by their side.
Helping a Person with Dementia to Eat and Drink Safely (PDF)
Advice on eating, drinking and swallowing in dementia (PDF)
Strategies for Feeding Patients with Dementia (PDF)
Thinning Evidence for Thickened Liquid Diets in Dementia and Dysphagia
Modifying the consistency of food and fluids for swallowing difficulties in dementia
Managing Dysphagia in Residents with Dementia
Soft Foods for Seniors With Swallowing Issues
How to Care for Someone with Swallowing Problems
Swallowing Difficulties in Dementia
Dementia support: understanding and helping with swallowing issues
Identifying Swallowing Difficulties: The Role of the Caregiver
Dementia: How physical and sensory difficulties can affect eating
Interventions to address mealtime support needs in dementia: A scoping review
Tube Feeding on Hospice — Increased Risk of Your Loved One Suffering
End-of-Life Nutrition: Is Tube Feeding the Solution?
Dementia care: an overview of available non-pharmacological therapies
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.