Full Code vs DNR: The Implications for Terminally Ill Patients and Their Caregivers
Published on August 2, 2024
Updated on August 2, 2024
Published on August 2, 2024
Updated on August 2, 2024
Table of Contents
If you are caring for a loved one who has a terminal illness, you may have to face a difficult decision: whether to choose full code or do not resuscitate (DNR) for their end-of-life care. What do these terms mean, and how do they affect your loved one and yourself?
Full code means that if your loved one’s heart stops beating or stops breathing, the medical team will do everything possible to revive them. This may include chest compressions, electric shocks, breathing tubes, and medications. Full code is also called cardiopulmonary resuscitation (CPR).
DNR means that if your loved one’s heart stops beating or stops breathing, the medical team will not attempt to revive them. They will only provide comfort measures, such as pain relief, oxygen, and emotional support. DNR is also called allow natural death (AND).
Choosing between full code and DNR is not easy. It depends on many factors, such as your loved one’s wishes, values, beliefs, and quality of life. It also depends on the chances of survival and recovery after CPR and the possible risks and complications.
According to a recent study, about 15% of terminally ill patients in the United States choose to be full code, while 85% choose to be DNR. However, these numbers may vary depending on the type of illness, the stage of the disease, and the setting of care.
This article aims to help you understand the outcomes of CPR and the benefits and drawbacks of full code and DNR for terminally ill patients and their caregivers. We will also discuss the impact of these decisions on family members and hospice staff, who are often involved in end-of-life care. We hope this article will provide helpful information, guidance, compassion, and support.
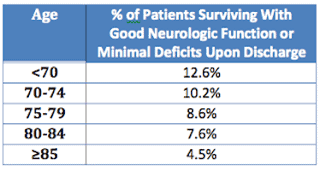
According to assorted studies, the success rate of CPR for non-terminal patients in a hospital setting where the patient is found in cardiac arrest quickly with CPR applied promptly, only twenty patients out of one hundred patients survive CPR, with sixteen of those twenty patients having a long-term impact to their quality of life.
In non-terminal patients in nursing homes, only five patients out of one hundred patients survive. For non-terminal home patients, the success rate varies tremendously based on how quickly (the longer the patient is without CPR, the more likely the patient will suffer brain damage even if the patient survives the CRP procedure) CPR is applied and the quality of the CPR applied by those giving CPR.
For those who are terminally ill, the success rate of CPR can be meager, with almost guaranteed broken ribs, punctured lungs, and witnesses of the highly violent procedure to restart the heart doing their best to avoid being sick watching their loved one go through a process that is often futile.
Some terminally ill patients may choose to be full code because they have hope that they can survive or recover from their illness or that a miracle or a cure will happen. They may also have faith in God or a higher power and believe that being full code follows their religious or spiritual beliefs. Some patients may have a fear of death or dying and want to avoid or delay it as much as possible. They may also have autonomy, meaning they can make decisions about their end-of-life care.
Being full code can have some benefits for terminally ill patients. One benefit is that it can potentially prolong life, which may give them more time to spend with their loved ones, to say goodbye, or to complete unfinished business. Another benefit is that it can preserve dignity, which means they can maintain their self-respect and identity and not feel like they are giving up or losing control. A third benefit is that it can honor wishes, meaning they can follow their personal or family preferences or respect their cultural or ethical values.
However, being full code can also have some drawbacks for terminally ill patients. One drawback is that it can cause immense suffering, which means that they can experience more pain, discomfort, or distress from the CPR procedures or their underlying illness. Another drawback is that it can be futile, which means it can have little or no chance of success or can only prolong the dying process, not the living. A third drawback is that it can burden others, putting more stress, pressure, or responsibility on their caregivers, family members, or hospice staff, who may have to witness or perform CPR or deal with the emotional or financial consequences.
Some terminally ill patients may choose to be DNR because they have acceptance of their condition and prognosis, and they do not want to prolong their suffering or delay their death. They may also seek comfort in their final days and prefer to focus on relieving their symptoms and improving their well-being. Some patients may value quality over quantity of life and want to have a meaningful and dignified death that reflects their personality and preferences. Some patients may also desire peace for themselves and their loved ones and want to avoid unnecessary conflicts or interventions that may cause more harm than good.
Being DNR can have some benefits for terminally ill patients. One benefit is that it can avoid invasive procedures, such as chest compressions, electric shocks, breathing tubes, and medications, which may be painful, stressful, or ineffective for the patient. Another benefit is that it can reduce pain by allowing the patient to receive adequate doses of painkillers or sedatives without worrying about the risk of respiratory depression or cardiac arrest. A third benefit is that it can enhance palliative care, which aims to improve the quality of life of patients and their families facing life-threatening illnesses by providing physical, emotional, social, and spiritual support.
However, being DNR can also have some drawbacks for terminally ill patients. One drawback is that it can hasten death, which may shorten the patient’s lifespan or deprive them of a chance of recovery or a miracle. Another drawback is that it can lose control, which may make the patient feel powerless or helpless or that they are giving up or surrendering to their illness. A third drawback is that it can feel guilty, which may make the patient feel like they are disappointed or abandoning their loved ones or violating their moral or religious principles.
Caring for a terminally ill patient who is full code or DNR can have a significant impact on the people who are involved in their end-of-life care. These people may include caregivers, such as spouses, children, siblings, or friends, who provide daily assistance and emotional support to the patient; family members, such as parents, grandparents, cousins, or relatives, who may visit or communicate with the patient; and hospice staff, such as nurses, doctors, social workers, or chaplains, who offer professional care and guidance to the patient and their family.
These groups may face different challenges and emotions when caring for a terminally ill patient who is full code or DNR. For example, caregivers may feel overwhelmed, exhausted, or isolated by the demands and responsibilities of caregiving. They may also feel conflicted, guilty, or angry if they disagree with the patient’s decision or must make decisions on their behalf. Family members may feel helpless, anxious, or sad about the patient’s condition or prognosis. They may also feel confused, frustrated, or resentful if they are uninformed or involved in decision-making. Hospice staff may feel stressed, pressured, or conflicted by the ethical or legal issues of providing end-of-life care. They may also feel compassionate, empathetic, or hopeful about the patient’s comfort and dignity.
These groups may also have different perspectives and expectations regarding full code and DNR for terminally ill patients. For example, caregivers may prefer full code because they want to keep their loved one alive as long as possible, or they may prefer DNR because they want to respect their loved one’s wishes and avoid unnecessary interventions. Family members may prefer full code because they hope for a miracle or a cure, or they may prefer DNR because they accept the reality and inevitability of death. Hospice staff may prefer full code because they have to preserve life and follow the patient’s consent, or they may prefer DNR because they have to provide comfort and palliative care and follow the patient’s best interest.
Therefore, it is essential to have communication, education, and support for these groups to cope with the stress and grief of end-of-life care. Communication means that the patient, the caregivers, the family members, and the hospice staff should talk openly and honestly about their feelings, thoughts, and preferences regarding full code and DNR. They should also listen respectfully and attentively to each other’s views and concerns and try to reach a mutual understanding and agreement. Education means that the patient, the caregivers, the family members, and the hospice staff should learn more about the benefits and drawbacks of full code and DNR, the medical and legal implications of these decisions, and the available resources and options for end-of-life care. They should also seek reliable and accurate information from credible sources, such as healthcare professionals, counselors, or organizations. Support means that the patient, the caregivers, the family members, and the hospice staff should receive emotional, social, and spiritual support from each other and other people or groups, such as friends, neighbors, clergy, or support groups. They should also seek professional help if they experience severe or persistent distress, such as depression, anxiety, or grief.
In this article, we have discussed the benefits and drawbacks of full code and DNR for terminally ill patients and their caregivers. We have also explored the impact of these decisions on family members and hospice staff, who are often involved in end-of-life care. We have learned that choosing between full code and DNR is not easy and that it depends on many factors, such as the patient’s wishes, values, beliefs, and quality of life, as well as the chances of survival and recovery after CPR, and the possible risks and complications. We have also learned that caring for a terminally ill patient who is full code or DNR can have a significant effect on the people who are involved in their end-of-life care and that they may face different challenges and emotions, as well as various perspectives and expectations, regarding full code and DNR.
We hope this article has helped you understand the complexity and diversity of full code and DNR decisions for terminally ill patients and their caregivers and provided helpful information, guidance, compassion, and support. However, we acknowledge that this article is not comprehensive or conclusive and that more questions or issues may need to be addressed. Therefore, we would like to offer some recommendations or implications for practice, policy, or research on this topic.
For practice, we recommend that the patient, the caregivers, the family members, and the hospice staff communicate, educate, and support each other and seek professional help, if needed, to cope with the stress and grief of end-of-life care. We also recommend that they respect and honor the patient’s decision, whether it is full code or DNR, and that they should not judge or pressure each other or themselves for their choices.
For policy, we suggest that the health care system and the legal system should provide clear and consistent guidelines and regulations for full code and DNR decisions and that they should protect the rights and interests of the patient, the caregivers, the family members, and the hospice staff. We also suggest that they should promote and facilitate advance care planning, which is a process of discussing and documenting the patient’s preferences and goals for end-of-life care, and that they should ensure that the patient’s decision is followed and respected by all parties.
For research, we propose that more studies should be conducted to investigate the benefits and drawbacks of full code and DNR for terminally ill patients and their caregivers and to evaluate the impact of these decisions on family members and hospice staff. We also propose that more studies should be conducted to explore the reasons, factors, and influences that affect full code and DNR decisions and to identify the best practices and strategies for improving the quality and outcomes of end-of-life care.
Long-Term Outcomes in Elderly Survivors of In-Hospital Cardiac Arrest
Outcomes of cardiopulmonary resuscitation in nursing homes: Can we predict who will benefit?
Opportunities and Risks of Resuscitation Attempts in Nursing Homes
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?