Introduction: Facing Dementia Without Labels
When a loved one starts showing signs of memory loss and confusion, it’s natural to feel worried and uncertain. Dementia is a word that can bring a lot of fear, but sometimes, doctors can’t tell us exactly what type of dementia our family member has. This can leave us feeling like we’re in the dark, trying to find our way without a clear label to guide us.
The Reality of Unspecified Dementia
Not knowing the specific type of dementia can be challenging. It’s like having a puzzle with missing pieces. You see changes in your loved one’s behavior or memory, but without a clear diagnosis, it’s hard to understand what this means for the future. This is unspecified dementia – when the exact cause isn’t known.
Purpose of the Article
This article is like a flashlight in the dark. It shines a light on the path ahead, even when we don’t have all the answers. We’ll discuss how dementia can affect people differently and share some common signs to help you guess what stage your loved one might be in.
What Caregivers Can Expect to Learn
As caregivers, you’re not alone. This article will give you tools and tips to help you recognize the signs of dementia’s progression. You’ll learn how to spot early, middle, and late-stage behaviors, which can help you provide the best care possible. We’ll also share resources and support options so you can find help and hope on this journey.
Remember, even without a specific diagnosis, you can still make a big difference in your loved one’s life. You can navigate this challenge together with patience, love, and the right information.
Understanding Dementia: A Broad Overview
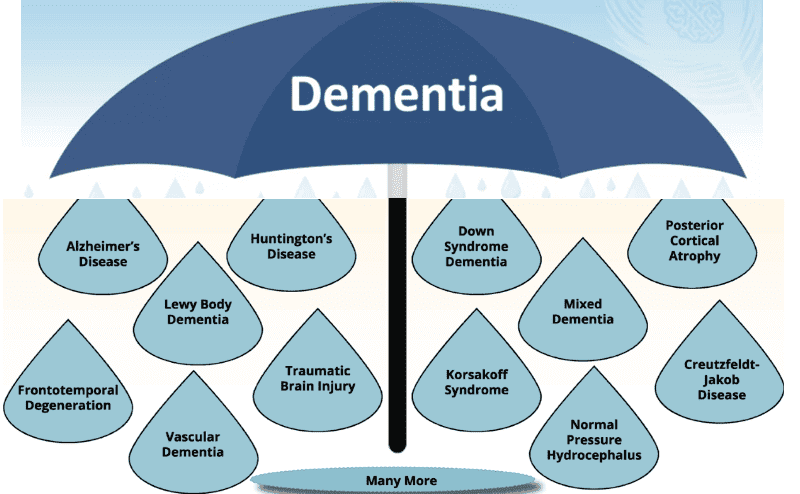
Dementia can be a confusing and scary word. It’s like an umbrella that covers many conditions affecting the brain. People with dementia may have trouble with their memory, find it hard to solve problems, or struggle with everyday tasks. It’s not just about forgetting where you put your keys; it’s like the brain is getting foggy, making it hard to think clearly.
What is Dementia?
Imagine your brain is like a busy office. Normally, everything is in order: files are where they should be, and everyone knows what they’re doing. Dementia is like someone mixing up all the files and turning off some of the lights. The brain’s ‘workers’—the nerve cells—can’t communicate well with each other, and things start to go wrong.
Common Types of Dementia
There are several types of dementia, each with its challenges. Alzheimer’s disease is the most common type, like a slow-moving storm that gradually changes the brain. Vascular dementia is like a series of small roadblocks in the brain’s blood vessels, causing sudden changes. Then there’s Lewy body dementia, which can make people see things that aren’t there, and frontotemporal dementia, which might change a person’s personality or language skills.
Each type of dementia affects people differently, and knowing which type a person has can help families and doctors provide the best care. But even when we don’t know the exact type, understanding these common forms can help us guess how the disease might progress and how to support our loved ones.
Summary of the Twelve Known Types of Dementia
There are currently thirteen (13) known types of dementia:
- Alzheimer’s disease is the most common type of dementia. It affects about six out of ten people with dementia (60%). Alzheimer’s disease damages the brain cells and causes them to die. This makes the brain shrink and have fewer connections. People with Alzheimer’s disease often struggle with memory, particularly in recalling recent events. They may also become confused, lose their sense of time and place, and experience changes in their mood and personality. Alzheimer’s disease gets worse over time, and there is no cure for it. But there are medicines and other ways to help people with Alzheimer’s disease live better.
- Vascular dementia is the second most common type of dementia. It affects about two out of ten people with dementia (20%). Vascular dementia happens when the blood vessels in the brain get damaged or blocked. This reduces the blood flow to the brain and causes brain cells to die. People with vascular dementia may have problems with thinking, planning, and organizing. They may also experience difficulties with speaking, walking, and managing their emotions. Vascular dementia can happen suddenly after a stroke or gradually over time. The symptoms and the speed of progression depend on the cause and the location of the brain damage. Vascular dementia cannot be cured, but some of the causes can be prevented or treated. For example, controlling high blood pressure, diabetes, and cholesterol can lower the risk of vascular dementia.
- Lewy body dementia is another common type of dementia. It affects about one out of ten people with dementia (10%). Lewy body dementia is caused by abnormal protein deposits called Lewy bodies that build up in the brain. These deposits affect the brain cells that control memory, thinking, and movement. Individuals with Lewy body dementia may experience difficulties with attention, alertness, and visual perception. They may also hallucinate, which means seeing or hearing things that are not there. They may also have symptoms of Parkinson’s disease, such as tremors, stiffness, and slowness. Lewy body dementia can vary from day to day and can be hard to diagnose. There is no cure for Lewy body dementia, but some medicines and other treatments can help with the symptoms.
- Frontotemporal dementia is a rare type of dementia that affects younger people between the ages of 45 and 65. Frontotemporal dementia is caused by damage to the front and side parts of the brain. These brain parts are responsible for personality, behavior, and language. People with frontotemporal dementia may have changes in their personality and behavior. They may misbehave, lose interest in things, or become more impulsive. They may also have problems with speaking, understanding, and writing. Frontotemporal dementia can be inherited, which means it can run in families. There is currently no cure for frontotemporal dementia; however, some medications and other therapies can help alleviate symptoms.
- Huntington’s disease is a genetic type of dementia that affects younger people between the ages of 30 and 50. Huntington’s disease is caused by a faulty gene that makes the brain cells die. This involves the brain cells that control movement, thinking, and emotions. People with Huntington’s disease may have involuntary movements, such as jerking, twitching, or writhing. They may also have problems with memory, concentration, and judgment. They may also have changes in their mood and personality, such as depression, irritability, or aggression. Huntington’s disease gets worse over time, and there is no cure for it. But there are medicines and other ways to help people with Huntington’s disease cope with the symptoms.
- Korsakoff dementia is a type of dementia that is caused by a lack of vitamin B1, also known as thiamine. Vitamin B1 helps the brain use energy from food. Without sufficient vitamin B1, brain cells cannot function properly and may die. Korsakoff dementia is often linked to alcohol abuse, but it can also happen for other reasons, such as malnutrition, infection, or cancer. Individuals with Korsakoff syndrome have severe memory problems, particularly when forming new memories. They may also invent stories or fabricate facts to fill in the gaps in their memory. This is called confabulation. They may also have problems with coordination and balance. Korsakoff dementia can be prevented by eating a balanced diet and avoiding alcohol. It can also be treated by taking vitamin B1 supplements and stopping alcohol use. Some people with Korsakoff dementia may recover partially or entirely, but others may have permanent damage.
- Limbic-predominant age-related TDP-43 encephalopathy (LATE) is a newly discovered type of dementia that affects older people over the age of eighty. LATE is caused by a protein called TDP-43, which builds up in the brain and damages brain cells. TDP-43 is typically found in the cell’s nucleus but moves out of the nucleus in late stages and forms clumps in the cytoplasm. This affects the brain cells that control memory and emotions. People with LATE experience difficulties with memory, particularly with recent memory. They may also have mood changes, such as depression or anxiety. LATE can be hard to tell apart from Alzheimer’s disease, but it tends to progress more slowly and affects fewer areas of the brain. LATE has no cure, but some medicines and other treatments may help alleviate symptoms.
- Normal pressure hydrocephalus (NPH) is a type of dementia that is caused by a buildup of fluid in the brain. The cerebrospinal fluid (CSF) flows around the brain and spinal cord, protecting them from injury. However, in NPH, the liquid does not drain properly, putting pressure on the brain. This affects the brain cells that control walking, thinking, and bladder control. People with NPH may experience difficulties with walking, such as shuffling, slowing down, or losing their balance. They may also have problems with memory, concentration, and reasoning. They may also have problems with holding urine or having accidents. NPH can be caused by head injury, infection, surgery, or aging. NPH can sometimes be treated by draining the excess fluid from the brain through a shunt tube. This can improve the symptoms and quality of life for some people with NPH.
- Parkinson’s dementia is a type of dementia that affects some people with Parkinson’s disease. Parkinson’s disease is a condition that affects the brain cells that produce a chemical called dopamine. Dopamine helps the brain control movement and coordination. People with Parkinson’s disease have less dopamine and have problems with movement, such as tremors, stiffness, and slowness. Parkinson’s dementia happens when the brain cells that control memory and thinking also get damaged. People with Parkinson’s dementia may have problems with memory, attention, and planning. They may also experience hallucinations, delusions, and paranoia. Parkinson’s dementia can happen at any stage of Parkinson’s disease, but it is more likely to occur in the later stages. There is no cure for Parkinson’s dementia, but some medicines and other treatments can help with the symptoms.
- Chronic traumatic encephalopathy (CTE) is a type of dementia that happens when the brain gets hurt many times. This can happen to people who play sports like football or boxing, or to people who are in the military or get hit in the head a lot. CTE damages brain cells, causing them to die. This causes the brain to become smaller and less interconnected. People with CTE have trouble remembering things, thinking clearly, and controlling their emotions. They may also act differently, get angry or sad quickly, or see or hear things that are not there. CTE gets worse over time, and there is no cure for it. However, there are ways to help people with CTE live better.
- Creutzfeldt-Jakob disease (CJD) is a rare type of dementia that is caused by a misfolded protein in the brain called a prion. Prions are usually harmless, but when they change shape and clump together, they cause the brain cells to die. This affects the brain cells that control memory, thinking, and movement. People with CJD may have problems with confusion, vision, speech, and balance. They may also have muscle cramps, seizures, and hallucinations. CJD can happen for no reason, or it can be inherited, or it can be passed on by contact with infected tissue. CJD is profoundly serious, and there is no cure for it. However, there are medications and other treatments that can help alleviate the symptoms.
- Mixed dementia is when a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can make it more challenging for the person to remember things, think clearly, and perform everyday tasks. They may also have other problems, depending on the types of dementia they have. For example, they may have trouble with movement, vision, or emotions. Mixed dementia can be complex to diagnose because the symptoms may overlap or change over time. Sometimes, the doctors may not know that a person has mixed dementia until they look at their brain after they die. However, some tests and scans can help doctors determine the types of dementia that are part of the picture.
- Logopenic Primary Progressive Aphasia, often abbreviated as LPPA, is a rare type of dementia that primarily affects language skills. Imagine a library where the books are in perfect condition, but the librarian struggles to find the right ones. That’s what LPPA is like. The person’s knowledge is intact, but finding the right words becomes increasingly tricky.
The Challenge of Undiagnosed Dementia
Caring for someone with dementia is a journey that often comes with many questions and few clear answers. When dementia doesn’t have a name, it’s like walking through a thick fog. It would be best to move forward, but seeing the path ahead is hard. This is the challenge of undiagnosed dementia – you’re doing your best without knowing exactly what you’re up against.
Why a Specific Diagnosis May Be Missing
Sometimes, despite the best efforts of doctors, a specific type of dementia remains a mystery. It could be because the symptoms overlap with many types of dementia, making it hard to pinpoint one. Or maybe the tests that could tell more aren’t available or are too hard on your loved one. It’s like trying to tune into a radio station but only getting static – you know there’s a clear signal somewhere, but you can’t find it.
Impact on Caregivers and Patients
Not having a diagnosis can feel like sailing without a compass for caregivers. You might feel lost, frustrated, or even scared. Planning for the future is tough when you don’t know what to expect. For patients, it means they might not get the most effective treatment right away, which can be confusing and upsetting.
But here’s the thing: your love and care can still make a huge difference, even without a specific diagnosis. By learning about the general stages of dementia and the common signs to look out for, you can create a loving and supportive environment for your loved one. And remember, you’re not alone. There are communities and resources out there to help guide you through the fog. Together, you can navigate these uncharted waters with hope and determination.
General Indicators of Dementia Progression
When we talk about dementia, we often think about memory loss, but it’s more than that. It’s a series of changes that can affect someone’s ability to do everyday things. As dementia progresses, these changes become more noticeable.
Cognitive Symptoms
Cognitive symptoms are like the brain’s tools getting a little rusty. Early on, someone might forget recent conversations or repeat themselves. As time passes, they might struggle with tasks they used to do easily, like balancing a checkbook or following a recipe. In the later stages, they may not recognize familiar faces or remember important life events.
Behavioral and Psychological Symptoms
Behavioral and psychological symptoms are like unexpected storms in the mind. Your loved one might get upset more easily or act in ways that don’t seem like them. They might see or hear things that aren’t there or believe things that aren’t true. Sometimes, they might wander or feel restless, especially in the late afternoon or evening.
Seeing these changes is tough, but understanding them can help you provide the proper support. Knowing what to expect can create a calm and safe space for your loved one, no matter where they are in their dementia journey. Remember, you’re not alone; both need help and support.
Staging Dementia: A Practical Approach
Understanding the stages of dementia can be like following a map through unfamiliar territory. It helps caregivers anticipate what might come next and how to prepare for it. Even without a specific diagnosis, there are common signs that can guide us.
Early-Stage Indicators
In the early stage, signs can be subtle and easily missed. It’s like starting a journey with a few clouds in the sky, but you can still see the road ahead. Your loved one might:
- Forget recent events or conversations.
- Misplace belongings more often.
- Have trouble finding the right words or names.
- Struggle with planning or organizing tasks.
Mid-Stage Manifestations
As the journey continues, the path gets a bit harder to follow. The clouds grow darker, and the road signs are harder to read. In the mid-stage, your loved one may:
- Repeat questions or stories.
- Need help with dressing or grooming.
- Show changes in sleep patterns.
- Experience mood swings or withdrawal.
Late-Stage Characteristics
The road becomes more challenging in the late stage, and the clouds can turn into storms. It’s when your loved one needs a lot of support and care. They might:
- Lose awareness of recent experiences and surroundings.
- Have difficulty communicating.
- Need full-time help with personal care.
- Show physical symptoms, like trouble walking or eating.
Remember, each person’s journey with dementia is unique. These stages are just a guide. With love, patience, and understanding, you can help make this journey as comfortable as possible for your loved one. And don’t forget, there’s a community of caregivers and professionals who can walk with you on this path. You’re not alone.
Tools and Resources for Caregivers
Caring for a loved one with dementia is a big responsibility, and it’s okay to seek help. Tools and resources are designed to make your role as a caregiver a bit easier. These can help you understand where your loved one is in their dementia journey and how you can best support them.
Cognitive Assessment Scales
Consider cognitive assessment scales as questions and tasks that help you measure how well your loved one’s brain works. It’s like a yardstick for the mind. These scales can show you if there are changes in their memory, language, and problem-solving abilities. Some common scales professionals use—and you can learn about—are the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA). They’re like quizzes that give you a snapshot of your loved one’s cognitive health.
Behavioral Observation Techniques
Behavioral observation is about watching and noting changes in how your loved one acts. It’s like being a detective, looking for clues in their behavior that tell you how they’re feeling and what they might need. You might notice they get upset at certain times of the day or in specific situations. Keeping a journal of these observations can help you spot patterns and plan. This way, you can create a calm environment that reduces stress for both of you.
Remember, using these tools doesn’t mean diagnosing your loved one—that’s a job for medical professionals. But they can give you valuable insights and help you communicate better with doctors and other caregivers. You’re doing an amazing job, and with the right tools, you can continue to provide loving and effective care.
Creating a Supportive Environment
Creating a supportive environment for someone with dementia is like building a nest – it’s all about making it safe, comfortable, and nurturing. It’s important to create a space where your loved one can feel secure and at ease, even as their needs change.
Adapting Care Strategies for Each Stage
As dementia progresses, your loved one’s abilities and needs will change. They might need reminders or help with complex tasks in the early stages. They may need more help with daily activities like dressing or eating as time passes. In the late stages, they may rely on you for most of their care.
Here’s how you can adapt:
- Early Stage: Keep routines simple and consistent. Use notes or alarms as reminders for important tasks.
- Mid Stage: Simplify choices to avoid confusion. Label cabinets or drawers with pictures to help find things.
- Late Stage: Focus on comfort and safety. Use adaptive equipment to assist with eating or bathing.
Communication Tips for Caregivers
Communication is key in caregiving. Here are some tips:
- Listen with your heart: Sometimes, it’s not about the words but the emotions behind them.
- Use simple language: Short, clear sentences can be easier to understand.
- Be patient: Give your loved one time to respond, and avoid interrupting.
- Use non-verbal cues: Smile, make eye contact, and use gentle touches to convey your message.
Remember, creating a supportive environment is about the physical space and the emotional atmosphere. Empathy, patience, and love are the most comforting things you can offer.
When to Seek Professional Help
Caring for a loved one with dementia is a road filled with love, challenges, and sometimes, uncertainty. Knowing when to seek professional help is crucial. It’s like recognizing when a storm is too big to handle alone, and calling in the experts is time.
Signs That It’s Time for Expert Intervention
There are moments when the changes in your loved one’s behavior or health signal a need for professional help. Here are some signs:
- Sudden changes in behavior or mood that are hard to manage.
- Safety concerns include wandering off or not recognizing dangers like a hot stove.
- Health issues that you’re not equipped to handle, such as problems with swallowing or walking.
- Caregiver stress is overwhelming and affects your health.
Navigating Healthcare Systems
Finding your way through the healthcare system can be daunting. It’s like entering a maze with lots of turns and dead ends. But there are ways to make it easier:
- Start with your loved one’s primary care doctor. They know your loved one’s history and can guide you to the right specialists.
- Reach out to local dementia support groups. They can offer advice and share their experiences with different services.
- Use community resources. Organizations like the Alzheimer’s Association provide tools and information to help you find the best care options.
Remember, asking for help is a sign of strength. It means you’re doing everything you can to ensure the best care for your loved one. As you navigate these waters, know that professionals, friends, and fellow caregivers are ready to support you every step of the way.
Conclusion: Embracing Uncertainty with Compassion
As we come to the end of our guide, it’s important to remember that dealing with dementia, especially without a clear diagnosis, is a journey of love, patience, and resilience. It’s about embracing the uncertainty with a heart full of compassion.
The Importance of Patience and Understanding
Patience is like a soft blanket on a cold night—it offers warmth and comfort when things seem overwhelming. Understanding is the light that helps us see through the fog of dementia. Together, they form the foundation of care that can weather the storm of this condition.
- Be patient: Your loved one may have good days and bad days. Patience means accepting this and being there for them, no matter what.
- Seek to understand: Try to step into their shoes and see the world from their perspective. This understanding can guide your actions and responses.
Finding Strength in Community and Support Networks
No one should walk this path alone. There’s strength in numbers, and finding a community of caregivers and support networks can be a lifeline.
- Join support groups: Sharing experiences with others who understand can be incredibly comforting and informative.
- Lean on resources: From local health services to national organizations, many resources are available to help you.
In conclusion, while the road may be uncertain, your journey with your loved one can be filled with joy and connection. With each step, remember that you’re not just a caregiver but a beacon of hope in your loved one’s life. And as you move forward, take comfort in knowing that there’s a whole community ready to support you in this act of love.
Resources
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer’s Disease and Other Dementias
Creating Moments of Joy Along the Alzheimer’s Journey: A Guide for Families and Caregivers, Fifth Edition, Revised and Expanded
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Caregiver Support Book Series
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
The Validation Breakthrough: Simple Techniques for Communicating with People with ‘Alzheimer’s-Type Dementia’
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Fading Reflection: Understanding the complexities of Dementia
Dementia Caregiving: A Self Help Book for Dementia Caregivers Offering Practical Coping Strategies and Support to Overcome Burnout, Increase Awareness, and Build Mental & Emotional Resilience
Navigating the Dementia Journey: A Compassionate Guide to Understanding, Supporting, and Living With Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
My Loved One with Dementia
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Disease and Other Dementias
How Do I Know You? Dementia at the End of Life
The Dementia Caregiver: A Guide to Caring for Someone with Alzheimer’s Disease and Other Neurocognitive Disorders (Guides to Caregiving)
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
The Caregiver’s Guide to Dementia: Practical Advice for Caring for Yourself and Your Loved One (Caregiver’s Guides)
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage