Considerations for Increasing Hospice Visit Frequencies
Published on March 26, 2023
Updated on December 18, 2024
Published on March 26, 2023
Updated on December 18, 2024
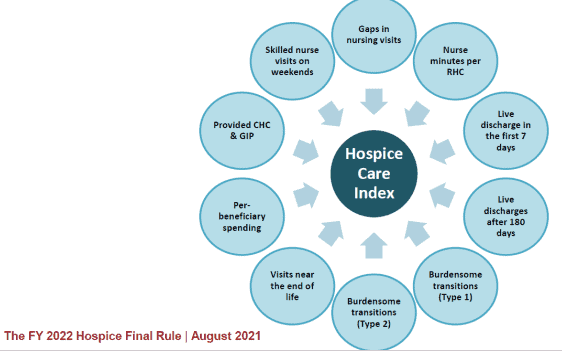
Table of Contents
Hospice care is focused on symptom management, pain relief, emotional support, and spiritual care. It is a privilege to be a part of a patient’s end-of-life journey, and as a new hospice nurse, you may feel overwhelmed, but you can make a difference in a patient’s life. One of the essential skills you need to learn as a hospice nurse is to recognize when to increase the scheduled visit frequency for a terminally ill patient under hospice care.
Before we dive into when to increase visit frequency, let’s review the hospice process. Hospice care is a service for people with serious illnesses who choose not to get (or continue) treatment to cure or control their illness. Hospice aims to provide comfort and peace to help improve the patient’s and their family’s quality of life. Hospice care typically involves a team of healthcare professionals, including doctors, nurses, social workers, chaplains, and volunteers, who work together to address the patient’s and their family’s physical, emotional, and spiritual needs.
As a hospice nurse, it’s important to consider several factors when determining if a patient requires an increased scheduled visit frequency. Here are some factors to consider:
As it relates to End-of-life care, every single visit, whether scheduled or PRN, should involve your documenting either in a recertification journal, a visit journal, or even in the patient’s narrative where appropriate, your clinical judgment as to where the patient is at within their hospice journey. How long do you think they have before their last breath? This is an “in the moment” clinical judgment that no one will hold you to in terms of exact standards but should help you have an idea of how often you need to put eyes on the patient as well as help you prepare the family for what may happen over the next several hours to several days to several weeks.
Always remember that you are a part of a hospice team. You may be alone in the field, but your medical director, supervisor, fellow nurses, and team members are a phone call or email away. Contact them if you are concerned about the frequency of scheduled visits. This can include asking for help from another nurse to see the patient more often if your caseload is too high.
Brand new admissions where the patient’s palliative performance scale (PPS) is 30% or higher and whose caregivers or family reports monthly to every other month significant declines: see the patient at least twice a week until you’ve confirmed a three-month to six-month estimate of what may remain of the patient’s lifespan.
If eligibility is questionable (i.e., they may be discharged for failure to decline), with patient and family agreement, back off visits to once a week to once every two weeks, with the understanding of the Medicare guideline for one visit every fourteen days.
For patients in the two-to-three-month window, at least twice-a-week visits; for those in the three-to-six-week window, three times a week visits; and for those with three weeks or less to live, daily visits, with consideration of telephone calls to skilled facilities on the weekend vs. in-person visits.
Caring for terminally ill patients under hospice care can be both challenging and rewarding. Knowing when to increase scheduled visit frequency is important to providing effective hospice care. By considering the factors listed above and being aware of the signs to look for, you can ensure that your patients receive the care and support they need during this challenging time. Remember, as a hospice nurse, you are part of a team of healthcare professionals who provide compassionate and comprehensive care to your patients and their families.
CMS Claims-based Quality Measure Development
Improving Your Agency with CMS Data: Quality Measures (HQRP) and PEPPER
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series