Category: Tips For Nurses
Articles for nurses caring for terminally ill patients including how to manage challenging situations.
Articles for nurses caring for terminally ill patients including how to manage challenging situations.
Dementia affects memory, thinking, and behavior, presenting challenges for patients and caregivers. This article discusses the best products for managing these challenges, enhancing quality of life for those with dementia.

Discover essential strategies for managing adrenal insufficiency crises in terminally ill patients. Learn about symptoms, risk factors, and crucial interventions to ensure patient comfort and safety. This guide provides valuable insights for hospice nurses and caregivers in this critical condition.

Explore the crucial roles of Karnofsky Performance Status (KPS) and Palliative Performance Score (PPS) in palliative and hospice care. This comprehensive guide helps nurses and caregivers understand these assessment tools, their applications, and critical differences, empowering them to provide more effective, patient-centered care.
Compliance-based, Eligibility Driven Hospice Documentation: Tips for Hospice Nurses" offers comprehensive guidance for hospice professionals. This valuable resource provides practical examples for various aspects of hospice care documentation, including admissions, recertifications, IDG/IDT notes, continuous care, and GIP records. Enhance your documentation skills while ensuring regulatory compliance.

Explore why side effects from medications can emerge after initial use and understand the critical need for vigilant monitoring and regular medication reconciliation to ensure patient safety and efficacy.
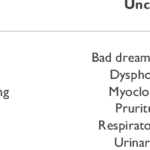
Learn about uncommon opioid side effects like myoclonus and hyperalgesia, and how they impact you and your family. This guide explains these conditions, offers tips for managing them, and highlights the role of hospice in providing comfort and support.

Hospice nurses are crucial in comforting and supporting patients nearing death and their families. This article explores what to expect from hospice care, focusing on patient assessments, educational discussions, and addressing common family concerns.

RUSH Medical Center's Caring for Caregivers (C4C) program offers vital support to those caring for adults 60 and older at home. Learn about the program's comprehensive approach, including skill-building sessions, planning assistance, and care-team coordination. Discover how C4C makes a difference in caregivers' lives and improves patient outcomes.

Discover how to use the CUS tool and Caring Feedback Model to advocate for your loved one's health. This guide empowers caregivers to communicate effectively with healthcare providers, ensuring their concerns are heard and addressed.

Explore comprehensive approaches to managing hallucinations in loved ones with dementia. This article covers pharmacological methods, focusing on Seroquel and non-drug strategies such as Naomi Feil's validation therapy. Learn how to validate feelings, de-escalate fear, and improve the quality of life for those experiencing cognitive impairment.
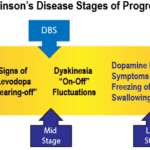
Identifying end-stage Parkinson's for hospice admission can be challenging. This article explores key criteria, including decline in function, weight loss, swallowing difficulties, and mobility issues. Learn how hospice professionals assess patients and utilize guidelines to ensure appropriate and timely hospice care for those with advanced Parkinson's disease.

Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.

Navigating interstate hospice transfers can be complex. This guide explores the process, challenges, and considerations for patients and families. Learn about Medicare regulations, coordination between hospice agencies, and how to ensure continuity of care when moving across state lines during end-of-life care.

Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients' better quality of life.

This guide covers how to write effective hospice nursing narratives, key documentation areas, and the importance of detailed and negative-based wording to support continued hospice eligibility.

The journey towards the end of life can be a challenging and emotional time, both for the individual facing the end of their life and for their caregivers and family members. One aspect of this journey that may be unfamiliar to many is the presence of self-soothing sounds made by the patient during the transition and actively dying phase. These sounds can be puzzling and sometimes unsettling for caregivers and family members who have never witnessed them. This article will explore self-soothing sounds, why they occur, and how caregivers and family members can distinguish between self-soothing sounds and signs of discomfort.
This article delves into the intricate relationship between dementia and seizures, offering insights on identification, safety protocols, and advocacy for caregivers.

As a hospice admission nurse, asking the right questions is crucial for assessing patients' eligibility and providing compassionate care. This article explores critical questions to understand the patient's condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a "good death" for patients and families.
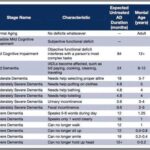
As a nurse who has cared for many terminally ill individuals with Alzheimer's disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer's disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
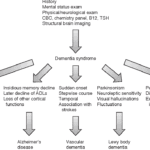
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care
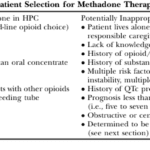
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

This article is crafted with heartfelt understanding and care, recognizing the challenges you face as caregivers and family members of terminally ill loved ones. Our goal is to empower you with knowledge and practical advice to manage the risk of aspiration pneumonia, a common yet often preventable complication in hospice care.

As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.