Category: Medications
Medications used for symptom management or otherwise
Medications used for symptom management or otherwise
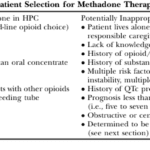
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

Discover the potential side effects of dementia medications and how to support your loved one.
Learn effective strategies for managing hallucinations in terminally ill patients. This guide covers pharmacological and non-pharmacological methods to improve comfort and quality of life.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.
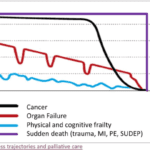
When a loved one is terminally ill, it can be a perplexing and emotional journey. Understanding the root cause of their declining health becomes paramount. It's a complex puzzle where family members often grapple with questions: Are the symptoms a result of medications prescribed, or are they intrinsic to the terminal disease? This article delves into the critical distinctions between medication side effects and the natural progression of terminal illnesses, offering insights to empower families and caregivers in making informed decisions about their loved one's care.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?

As an experienced hospice nurse, I understand that working in hospice care can be emotionally and physically challenging. In this presentation, I will share my knowledge and expertise on the topics of death and dying, as well as comfort medications including morphine, to help guide you in providing the best care for your patients.

Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives - Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.
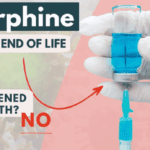
As a hospice nurse with years of experience, I have encountered many situations where family members are hesitant to allow their loved ones to receive medications such as morphine and lorazepam. One of the main reasons for this hesitancy is the belief that these medications will hasten death, leading to euthanasia.
In this article, I want to address this concern and help family members and friends understand the use of morphine and lorazepam in hospice care.

I’ve seen firsthand how important it is to understand comfort and discomfort in hospice care. Let’s dive into these terms and how they relate to end-of-life care.

Hospice comfort medications play a vital role in managing end-of-life symptoms. From morphine for pain and breathing difficulties to lorazepam for anxiety and restlessness, these medications are carefully administered to enhance quality of life while ensuring patient comfort and dignity.
Hey there, my friend! As an experienced hospice nurse, I understand that managing symptoms for comfort is crucial for terminally ill patients. One of the ways we do this is through PRN medications. Today, I want to help you understand PRN medications and how they can be used in conjunction with scheduled medications.
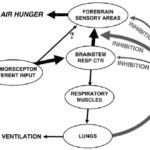
I can count the times I’ve run into air hunger at the end of life as a visiting RN Case Manager for going on five years on one hand. Over the years, I’ve managed patients with pulmonary fibrosis, lung cancers (diverse types), breast cancer, COPD, congestive heart failure, B-cell lymphoma, leukemia, and other diseases that can impact one person’s ability to breathe correctly. Air hunger is rare in my firsthand experiences, but it can happen.
Air hunger often sounds like the person is gasping for breath without regard to the actual respiratory rate (how fast they are breathing); it can also sound like stridor (YouTube videos below where you can hear the difference).

Ativan, generically called Lorazepam, pills can be easily melted into liquid, and given to your loved one in a syringe. This is typically done vs. putting the pill under the tongue if your loved one has a dry mouth, and the Ativan pills are not melting under the tongue.
The process of melting lorazepam into a liquid will require the following resources:
Hemoptysis, or coughing up blood, can be a distressing symptom for patients at the end of their life journey. As a hospice nurse, your expertise in managing this symptom is crucial in ensuring a peaceful and comfortable experience for your patients and their families.
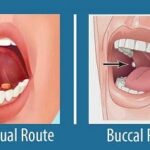
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter).
The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.

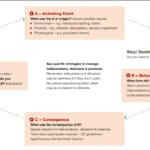
Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.
Morphine is a crucial medication in end-of-life care, but it's often misunderstood. This article debunks common myths about morphine use in hospice, addressing concerns about addiction, hastening death, and sedation. Learn the truth about morphine's role in providing comfort and dignity for terminally ill patients.