Antipsychotics & Dementia Risk: A Critical Analysis
Published on February 26, 2025
Updated on February 25, 2025
Published on February 26, 2025
Updated on February 25, 2025
Table of Contents
When a loved one is diagnosed with dementia, it’s a journey that affects the whole family. It’s natural to have many questions, especially about their needed medications. Antipsychotic medications are one type that doctors might suggest, and it’s essential to understand what they are and how they’re used in dementia care.
Antipsychotics are a group of medicines that can help manage the symptoms of certain mental health conditions. They’re often used to treat illnesses like schizophrenia or bipolar disorder, but sometimes, they’re also prescribed for people with dementia. These medications can help with difficult symptoms like agitation, aggression, or severe confusion, which can be tough for both the person with dementia and their caregivers.
But it’s not a decision to take lightly. Antipsychotics can have side effects, and they don’t work the same way for everyone. It’s like finding the correct key for a tricky lock – sometimes, it takes a few tries to find the best fit. And just like you’d talk to a locksmith for a tricky lock, it’s crucial to have open conversations with doctors about the benefits and risks of antipsychotic medications.
You might be surprised to learn that antipsychotics are pretty common in dementia care. It’s because those challenging behaviors – the ones that can make caregiving so challenging – are also really hard for our loved ones. Doctors turn to these medications, hoping to bring some peace and comfort.
But here’s the thing: just because something is familiar doesn’t mean it’s the best choice for everyone. That’s why staying informed and involved in your loved one’s care is so important. Ask questions, learn about the medications, and explore all the options. Your voice and care are potent tools in ensuring your loved one gets the best possible support.
Remember, you’re not alone on this journey. Doctors, nurses, and support groups are ready to help you navigate these decisions. Together, you can find the path that’s best for your family.
Caring for someone with dementia is a path filled with love, patience, and, sometimes, tough choices. One of those choices might be about antipsychotic medications. Let’s take a closer look at what recent research says about these drugs and how they relate to dementia.
Recent studies have raised concerns about the use of antipsychotic medications in people with dementia. These drugs, which are often prescribed to manage symptoms like agitation or aggression, have been linked to an increased risk of severe health issues. For example, a study published in The BMJ found that the use of antipsychotics in people with dementia is associated with higher risks of heart attack, stroke, heart failure, and even pneumonia.
It’s important to know that these risks are highest soon after starting the medication. This means that if your loved one is beginning antipsychotic treatment, it’s crucial to monitor them closely and have regular check-ins with their healthcare provider.
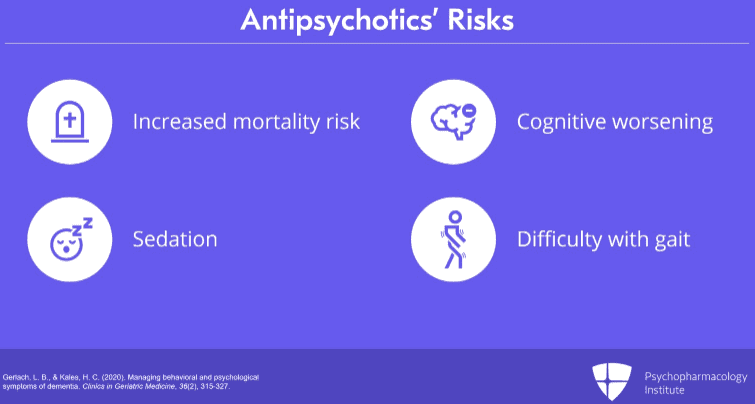
While antipsychotics can sometimes help with specific behavioral symptoms of dementia, they can also have the opposite effect. Some research suggests that these medications can worsen cognitive function, leading to increased confusion and memory problems. They may also cause side effects like drowsiness and shaking or even make dementia symptoms like thinking and memory problems worse.
It’s a delicate balance to strike. You want to ease your loved one’s distress, but not at the cost of their overall health and well-being. That’s why staying informed and working closely with doctors is essential to finding the best care plan for your family member.
Remember, you’re not alone in this. There are resources and support systems for caregivers like you. By staying informed and advocating for your loved one, you can provide them with the best care possible.
Navigating the care of someone with dementia is like being a detective. You gather clues to make the best health decisions for your loved one. When it comes to antipsychotics, understanding how they work and their long-term effects is key to making informed choices.
Neurotransmitters are like the brain’s messengers, carrying signals that help control everything from our movements to our mood. In dementia, these messengers can get mixed up, and antipsychotic medications aim to help by adjusting the levels of these chemicals.
However, it’s not always straightforward. Sometimes, these medications can tip the balance too much, leading to other issues. For example, they might block certain neurotransmitters, which can help with some symptoms but also increase the risk of falls or confuse someone.
When a family member starts on antipsychotics, you might notice some immediate changes, but it’s the long-term effects that often go unnoticed at first. Over time, these drugs can affect the brain’s ability to think and remember. Studies have shown long-term use might lead to attention, memory, and problem-solving difficulties.
It’s a lot to think about, and feeling overwhelmed is normal. But remember, you’re the advocate for your loved one’s health. By understanding how these medications work and their potential impact, you can have meaningful discussions with healthcare providers about the best path forward.
Caring for someone with dementia is a journey of love and dedication. As you continue to support your loved one, know that your efforts to understand their treatment can make a real difference in their quality of life.
When we talk about dementia and the use of antipsychotic medications, it’s like navigating a complex map. Each person’s journey is unique; some paths may have more challenges. Understanding who might be at higher risk when taking these medications can help us choose the safest route.
Not everyone with dementia will have the same experience with antipsychotic medications. Some people might be more sensitive to these drugs, and it’s essential to know who these individuals are. Factors like age, overall health, and the severity of dementia symptoms can play a big role. For instance, someone who has other health issues, like heart problems or diabetes, might be at a higher risk for side effects from antipsychotics.
Knowing which areas of the map are prone to storms is like being aware of which areas are prone to storms; if we’re aware, we can better prepare. That’s why doctors often take extra care when prescribing these medications to someone who might be more vulnerable.
Learning from others’ experiences can be incredibly valuable. Case studies, which are detailed reports about individual patients, show us how antipsychotic medications have affected other people with dementia. These stories can range from someone who responded positively to treatment to another who may have experienced significant side effects.
Clinical observations are like notes a traveler might take on their journey. Healthcare professionals observe and record how patients respond to antipsychotic medications over time. These notes can reveal patterns, such as which symptoms might improve and which side effects to watch out for.
Understanding these profiles and observations can better equip caregivers to advocate for their loved ones. It’s about making informed decisions with healthcare providers to ensure the best care for those we love.
Caring for a loved one with dementia is a journey that requires compassion, understanding, and, sometimes, exploring paths less taken. When considering treatments, it’s not only about medications. There are many ways to support someone with dementia that don’t involve drugs. Let’s explore some of these alternative approaches together.
Sometimes, the best medicine doesn’t come in a bottle. Non-pharmacological approaches focus on the person, not just the symptoms. These methods include activities and therapies that engage and support individuals with dementia more naturally.
For example, reminiscence therapy uses memories from the past to create feelings of comfort and familiarity. Music therapy can soothe the soul and awaken memories through songs. Art and horticultural therapies provide a creative outlet and a connection to nature. These approaches can help reduce agitation and improve mood without the need for medication.
The way we live our daily lives can also significantly impact dementia. Simple lifestyle adjustments can make a big difference. Ensuring plenty of sleep, staying physically active, and eating a balanced diet of fruits and vegetables all support brain health.
Supportive therapies like massage or TENS (Transcutaneous Electrical Nerve Stimulation) can help with relaxation and pain relief. Occupational therapy can assist in adapting the living environment to suit the needs of someone with dementia better, making daily tasks easier.
These alternative treatments and preventative measures are like tools in a toolbox. Each one has its purpose and can be helpful in different situations. By combining these approaches with traditional care, you can create a comprehensive plan that supports your loved one’s well-being in every way possible. Remember, you’re not just a caregiver; you’re a vital part of their support system, and your efforts make a world of difference.
Knowing the best course of action when caring for a family member with dementia can be challenging. Expert opinions and guidelines are like a compass that guides us through the complex landscape of dementia care. Let’s explore what the experts say about antipsychotic use and the latest care protocols for dementia patients.
The medical community is cautious about the use of antipsychotic medications in dementia care. While these drugs can sometimes help manage severe symptoms like agitation or psychosis, they also come with risks. Recent studies have shown that antipsychotics can increase the risk of severe health issues, such as heart attack, stroke, and even pneumonia, especially soon after starting the medication.
Experts suggest that antipsychotic medications should not be the first choice for managing dementia symptoms. Instead, they recommend considering them only when non-pharmacological approaches have not been successful and when symptoms are severe enough to pose a risk of harm to the patient or others. The goal is to use the lowest effective dose for the shortest time possible.
Care for dementia patients always evolves as we learn more about the disease. Updated care protocols emphasize a person-centered approach, which means focusing on each person’s individual needs and preferences. These guidelines first encourage non-drug approaches, such as environmental modifications, structured activities, and behavioral strategies.
When medications are necessary, the protocols advise careful monitoring and regular reassessment to ensure the benefits outweigh the risks. They also highlight the importance of involving family members and caregivers in the care planning process, ensuring they have the information and support they need to make informed decisions.
Navigating dementia care can be overwhelming, but you’re not alone. By staying informed and working closely with healthcare professionals, you can help ensure your loved one receives the best care tailored to their unique situation. Remember, your role as a caregiver is invaluable, and your love and support make all the difference in your loved one’s journey with dementia.
As we come to the end of our journey through understanding antipsychotics and their role in dementia care, it’s essential to reflect on what we’ve learned and look ahead to how we can apply this knowledge for the betterment of our loved ones.
The evidence we’ve gathered paints a complex picture. While antipsychotics can help manage certain symptoms of dementia, they also carry risks that cannot be ignored. Studies have shown that these medications can increase the chances of severe health issues like heart problems, stroke, and even pneumonia, especially soon after starting them. It’s clear that while these drugs may offer some relief, they should be used with great caution and under close supervision.
Looking forward, the treatment of dementia is evolving. The focus is shifting towards a more personalized approach, considering the unique needs of each individual. This includes exploring non-drug therapies and lifestyle changes that can improve quality of life without the added risks of medication. Research continues to advance, and new treatments are on the horizon that promise to target the underlying causes of dementia more effectively.
As caregivers, we stay informed, ask questions, and work closely with healthcare professionals to navigate the best course of action for our loved ones. It’s about finding the right balance between managing symptoms and maintaining overall health and well-being. With compassion, understanding, and knowledge, we can help guide our loved ones through the challenges of dementia with hope and dignity.
Antipsychotics Lead to Dementia; New Research Illuminates Why
Dementia: The risks of prescribing antipsychotic drugs as a treatment
Understanding The Contraindication Of Antipsychotics In Dementia Patients
Antipsychotics and other drug approaches in dementia care
Anticholinergic Drug Exposure and the Risk of Dementia: A Nested Case-Control Study
Antipsychotics for dementia associated with elevated risks of serious adverse outcomes
5 Medications to Avoid for People with Dementia
Use of antipsychotics in adults with dementia
Frontiers | Antipsychotic Treatment of Behavioral and Psychological Symptoms of Dementia (BPSD)
Long-term effects of antipsychotics (article 1)
Long-term effects of antipsychotics (article 2)
Long-Term Antipsychotic Use Leads to Poorer Cognitive Functioning
The risk of using antipsychotic medications to treat dementia
Non-pharmacological interventions in dementia
Non-pharmacological approaches to alleviate distress in dementia care
Therapy for dementia: Types, benefits, and more
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage