As experienced hospice nurses, our primary goal is to provide the best possible care and comfort to our terminally ill patients during their final journey. Pain management is a crucial aspect of hospice care, and it becomes even more challenging when dealing with patients who may have difficulty expressing their pain due to cognitive impairments or other factors. In such situations, the PAINAD scale emerges as a valuable tool for pain assessment. Let’s explore why and when using the PAINAD scale is essential, particularly when patients consistently over or underreport their pain.
The Significance of the PAINAD Scale
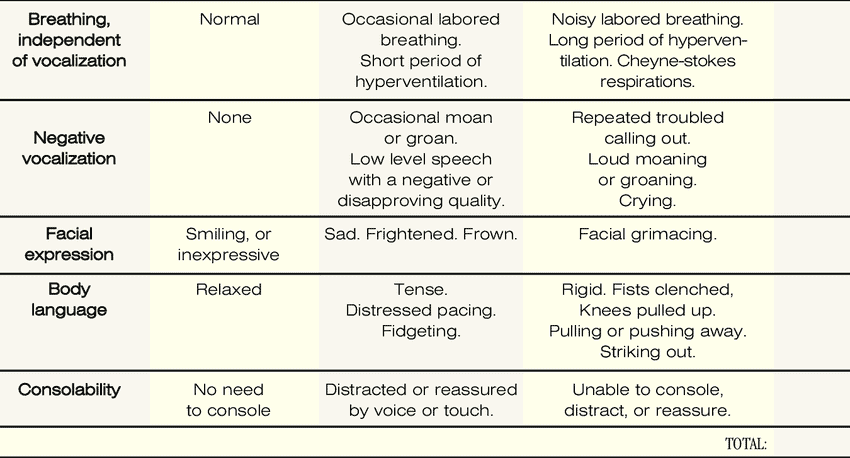
The Pain Assessment In Advanced Dementia (PAINAD) scale is designed to assess pain in nonverbal or cognitively impaired older adults. It focuses on five observable behaviors, including:
- Breathing
- Vocalization
- Facial expression
- Body language
- Consolability
By observing these behaviors, we can gain valuable insights into our patient’s pain experience, even if they cannot verbally express it. The PAINAD scale allows us to identify and address pain effectively, ensuring our patients receive the utmost comfort and care during their end-of-life journey.
When to Use the PAINAD Scale
- Cognitive Impairments: Some people have problems with their memory or thinking. They may forget things, get confused, or have trouble speaking. This can make it hard for them to tell us when they are in pain. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can look at how they breathe, how they sound, how they look, how they move, and how they react to comfort. Based on these signs, we can give them a score from 0 to 10. The higher the score, the more pain they have. The PAINAD scale helps us understand their pain and treat them properly.
- Communication Barriers: Some people speak different languages or have trouble hearing or speaking. This can make it hard for them to tell us how much pain they have. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can use the same signs as before: breathing, sound, look, movement, and reaction. Based on these signs, we can give them a score from 0 to 10. The PAINAD scale helps us communicate and give them the proper treatment.
- Consistent Over- or Underreporting: Some people may say they have more pain than they have. They may do this to get more attention or medicine. Some people may say they have less pain than they have. They may do this to be brave or not bother anyone. These habits can make it hard for us to know how much pain they have. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can use the same signs as before: breathing, sound, look, movement, and reaction. Based on these signs, we can give them a score from 0 to 10. The PAINAD scale helps us be fair and honest and gives them the proper treatment.
- Disease Progression: Some people have diseases that get worse over time. They may lose their strength, appetite, or ability to do things. They may also lose their ability to tell us when they are in pain. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can use the same signs as before: breathing, sound, look, movement, and reaction. Based on these signs, we can give them a score from 0 to 10. The PAINAD scale helps us care for them and treat them properly.
- Pain Management: Some people have pain that is hard to treat. They may need different medicine or other ways to help them feel better. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can use the same signs as before: breathing, sound, look, movement, and reaction. Based on these signs, we can give them a score from 0 to 10. The PAINAD scale helps us measure their pain and determine whether the treatment works. We can change the treatment if the score is too high or too low.
- Family Involvement: Some people have family members who love them and want to help them. They may visit them, talk to them, or comfort them. The PAINAD scale is a way to look at their behavior and see if they are in pain. We can use the same signs as before: breathing, sound, look, movement, and reaction. Based on these signs, we can give them a score from 0 to 10. The PAINAD scale helps us involve the family in the pain assessment and management. We can teach them how to use the scale and what to do if the score is too high or too low. We can also listen to their concerns and suggestions. The PAINAD scale helps us work with the family and give them the best care.
How to use the PAINAD Scale
Step 1: Observe Your Loved One
Before using the PAINAD scale, you must observe your loved one for five minutes. During this time, look for behaviors that might indicate discomfort or pain. These behaviors include:
- Facial expressions: Look for frowning, grimacing, or other signs of distress on your loved one’s face.
- Vocalizations: Listen for moaning, groaning, or other sounds that might indicate discomfort.
- Body language: Look for tense muscles, restlessness, or other signs of discomfort in your loved one’s body language.
- Breathing: Observe your loved one’s breathing for signs of distress, such as rapid or shallow breathing.
- Consolability: Try to console your loved one by holding their hand or speaking to them soothingly. Observe how they respond.
Step 2: Score Your Loved One’s Behaviors
After observing your loved one for five minutes, you can use the PAINAD scale to score their behaviors. The scale uses a score of 0-2 for each behavior, with a total score ranging from 0-10. Here’s how to score each behavior:
- Facial expressions: Look for furrowing of the brow, narrowing of the eyes, or deepening of the nasolabial furrow (lines on your face around your nose and mouth)—score 0 for no expression, 1 for mild, and 2 for moderate to severe.
- Vocalizations: Listen for moaning, groaning, or other sounds that might indicate discomfort. Score 0 for no vocalization, 1 for occasional moaning or groaning, and 2 for frequent or loud vocalization.
- Body language: Look for tense muscles, restlessness, or other signs of discomfort in your loved one’s body language. Score 0 for relaxed muscles, 1 for tense or restlessness, and 2 for rigid or constant restlessness.
- Breathing: Observe your loved one’s breathing for signs of distress, such as rapid or shallow breathing. Score 0 for normal breathing, 1 for occasional labored breathing or short periods of hyperventilation, and 2 for noisy labored breathing, long periods of hyperventilation, or Cheyne-Stokes respirations.
- Consolability: Try to console your loved one by holding their hand or speaking to them soothingly. Observe how they respond. Score 0 for easily consoled, 1 for difficult to console, and 2 for unable to console.
Step 3: Interpret Your Loved One’s Score
Once you have scored your loved one’s behaviors, you can interpret their score. A score of zero (0) means no pain. A score of 1-3 indicates mild discomfort. A score of 4-7 indicates moderate discomfort. A score of 8-10 indicates severe discomfort. Providers should be notified of severe discomfort.
Hospice PAINAD Score to Rating and Recommendations
| PAINAD Score | Pain Severity | Recommendations |
| 0 | None | None |
| 1-3 | Mild | Nothing to Acetaminophen (Tylenol) |
| 4-7 | Moderate | Opioid / Breakthrough Pain Medication |
| 8-10 | Severe | Call your provider! Opioid / Breakthrough Pain Medication |
Please always consult your hospice provider or doctor in terms of the recommendations or changes to the table that they would apply and follow their instructions!
Examples of the PAINAD Scale in Action
Example 1: PAINAD score of 0
You are visiting your grandmother, who has dementia, at her nursing home. You notice that she is smiling and relaxed. She usually breathes and does not make any noises. She does not seem to have any pain in her face or body. She is happy to see you and responds to your voice and touch. You use the PAINAD scale to score her pain as follows:
- Breathing: 0 (normal)
- Negative vocalization: 0 (none)
- Facial expression: 0 (smiling)
- Body language: 0 (relaxed)
- Consolability: 0 (no need to console)
The total score is 0, which means she has no pain. You are glad that she is comfortable and enjoy spending time with her.
Example 2: PAINAD score of 3
You are helping your father, who has dementia, with his morning routine. He has arthritis and sometimes has pain in his joints. You notice that he is breathing harder than usual and occasionally moans. He looks sad and frowns when you touch his arms or legs. He is tense and fidgets with his hands. He is distracted by your voice and touch but still seems unhappy. You use the PAINAD scale to score his pain as follows:
- Breathing: 1 (occasional labored breathing)
- Negative vocalization: 1 (occasional moan or groan)
- Facial expression: 1 (sad)
- Body language: 1 (tense)
- Consolability: 1 (distracted or reassured by voice or touch)
The total score is 3, which means he has mild pain. You decide to give him his pain medication and massage his joints gently. You hope that his pain will improve soon.
Example 3: PAINAD score of 4
You are taking your mother, who has dementia, to the dentist. She has a toothache and needs a filling. You notice that she is breathing rapidly and deeply. She makes a low-level speech with a negative or disapproving quality. She looks frightened and grimaces when the dentist examines her mouth. She is rigid and pulls away from the dentist. She is unable to console, distract, or reassure. You use the PAINAD scale to score her pain as follows:
- Breathing: 2 (short period of hyperventilation)
- Negative vocalization: 1 (low-level speech with a negative or disapproving quality)
- Facial expression: 2 (frightened)
- Body language: 2 (rigid)
- Consolability: 0 (unable to console, distract or reassure)
The total score is 4, which means she has moderate pain. You ask the dentist to give her some local anesthesia and explain what he is going to do. You hold her hand and talk to her calmly. You hope that the procedure will be over soon and that her pain will go away.
Example 4: PAINAD score of 7
You are watching your husband, who has dementia, at home. He has a urinary tract infection and needs antibiotics. You notice that he is breathing noisily and laboriously. He cries out loud and repeats troubled phrases. He looks angry and facially grimaces. He is rigid and strikes out at you when you try to help him. He is unable to console, distract, or reassure. You use the PAINAD scale to score his pain as follows:
- Breathing: 2 (noisy labored breathing)
- Negative vocalization: 2 (repeated troubled calling out)
- Facial expression: 2 (facial grimacing)
- Body language: 2 (striking out)
- Consolability: 0 (unable to console, distract or reassure)
The total score is 7, which means he has severe pain. You call his doctor and ask for advice. You give him his pain medication and try to keep him comfortable. You hope the infection will clear up soon and his pain will subside.
Example 5: PAINAD score of 10
You are accompanying your sister, who has dementia, to the hospital. She has fallen and broken her hip. You notice she is breathing in a rhythmic pattern of very deep to shallow respirations with periods of no breathing. She screams and cries loudly. She looks in agony and facially grimaces. She is rigid and clenches her fists and knees. She is unable to console, distract, or reassure. You use the PAINAD scale to score her pain as follows:
- Breathing: 2 (Cheyne-Stokes respirations)
- Negative vocalization: 2 (crying)
- Facial expression: 2 (facial grimacing)
- Body language: 2 (rigid)
- Consolability: 0 (unable to console, distract or reassure)
The total score is 10, which means she has severe pain. You alert the hospital staff and ask for immediate help. You give her your support and sympathy. You hope that she will get the treatment she needs and that her pain will be relieved.
Remembering the Importance of Empathy
As hospice nurses, we must approach pain assessment with empathy and sensitivity, recognizing that each patient’s pain experience is unique. The PAINAD scale is a tool that complements our clinical judgment and enhances our ability to provide compassionate care.
Always take the time to:
- Observe: Sometimes, people cannot tell us when they are in pain. They may not be able to talk or understand us. They may not know they are in pain. They may not want to tell us. The PAINAD scale is a way to watch their behavior and see if they are in pain. We can look at how they breathe, how they sound, how they look, how they move, and how they react to comfort. Based on these signs, we can give them a score from 0 to 10. The higher the score, the more pain they have. We need to pay close attention to these signs and notice any changes that could make them more or less painful.
- Document: When using the PAINAD scale, we must write down what we see and do. We need to write down the date, the time, the score, and the treatment. We need to write clearly and in detail. This helps us keep track of the pain and the medicine. This also helps us share the information with others caring for the patient. They can read what we wrote and know what to do next. Writing down the PAINAD scale helps us manage the pain and communicate better.
- Collaborate: We are not the only ones who care for the patient. Other people can help us. They may be doctors, nurses, social workers, chaplains, or volunteers. They may be family members, friends, or caregivers. They may know the patient better than us. They may have different ideas or skills. We need to work closely with them and listen to them. They can help us understand the patient’s pain better. They can also help us with the PAINAD scale. They can use the scale with us or tell us what they see or hear. They can also tell us how they feel or what they need. Working together with others helps us care for the patient better.
- Reassess: Pain is not always the same. It can change over time. It can get worse or better. It can move to different parts of the body. It can also change with the disease. The patient may get sicker or better. They may lose or gain abilities. They may need more or less medicine. We need to check the pain often using the PAINAD scale. We need to see if the score changes. We need to see if the treatment works. We need to see if the patient needs something different. Checking the pain regularly helps us keep the pain under control.
- Educate: Sometimes, people do not know much about pain or the PAINAD scale. They may not know why we use the scale or how it works. They may not know what the signs of pain are or what the score means. They may not know what the treatment is or how it helps. We need to teach them about pain and the PAINAD scale. We need to explain what we do and why we do it. We need to answer their questions and clear their doubts. We need to use simple words and examples. We need to make sure they understand and agree. Teaching them about pain and the PAINAD scale helps them trust us and cooperate with us.
- Empathize: Pain is not just a physical feeling. It can also affect the emotions and the spirit. Pain can make people feel sad, angry, scared, or hopeless. Pain can make people feel alone, helpless, or worthless. Pain can make people lose their faith, meaning, or purpose. We need to care for the whole person, not just the body. We need to feel what they feel and show them we care. We need to listen to their stories and respect their choices. We need to comfort them and support them. We need to be kind and gentle. Feeling and showing empathy helps them cope with pain and find peace.
Conclusion
The PAINAD scale is an invaluable tool for assessing pain in terminally ill patients, especially those with cognitive impairments or communication barriers. By focusing on observable behaviors such as breathing, vocalization, facial expression, body language, and consolability, the scale provides insights into the patient’s pain experience, enabling healthcare providers to address pain effectively and ensure the utmost comfort and care during the end-of-life journey.
The scale’s significance lies in its ability to aid in pain assessment for individuals with cognitive impairments, communication barriers, consistent over- or underreporting of pain, disease progression, challenging pain management, and involving family members in the assessment and management process. Additionally, the scale emphasizes the importance of empathy and sensitivity in pain assessment, complementing clinical judgment and enhancing the delivery of compassionate care.
Furthermore, the scale’s practical application involves careful observation, detailed documentation, collaboration with other healthcare professionals and family members, regular reassessment, patient and caregiver education, and the expression of empathy to address the emotional and spiritual aspects of pain.
Ultimately, the PAINAD scale serves as a critical instrument in ensuring that terminally ill patients receive comprehensive and personalized pain management, aligning with the core values of empathy and compassion that are central to hospice care.
Resources
Discomfort should be managed
Pain Assessment in Nonverbal Patients
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
PAINAD Scale Offers Alternative to Assessing Pain in the Dementia Patient – JEMS: EMS, Emergency Medical Services – Training, Paramedic, EMT News
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Chronic Pain & Symptom Tracker: A 90-Day Guided Journal: Detailed Daily Pain Assessment Diary, Mood Tracker & Medication Log for Chronic Illness Management
Pain And Symptom Tracker: Daily Pain Tracking Journal Detailed Pain Assessment Diary, Medication, Supplements Food & Activities Log for Chronic Illness Management
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
FLACC Pain Scale
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
My Loved One with Dementia
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Disease and Other Dementias
How Do I Know You? Dementia at the End of Life
The Dementia Caregiver: A Guide to Caring for Someone with Alzheimer’s Disease and Other Neurocognitive Disorders (Guides to Caregiving)
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
The Caregiver’s Guide to Dementia: Practical Advice for Caring for Yourself and Your Loved One (Caregiver’s Guides)
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
The Last Hours of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home