Introduction
When a loved one receives a terminal diagnosis, it’s natural to wonder about the journey ahead. Terminal illnesses follow a unique path, and understanding the signs and symptoms at various stages can help you provide the best care and support. This article aims to guide you through the general progression of terminal illnesses, focusing on observable signs and symptoms as the patient approaches the end of life.
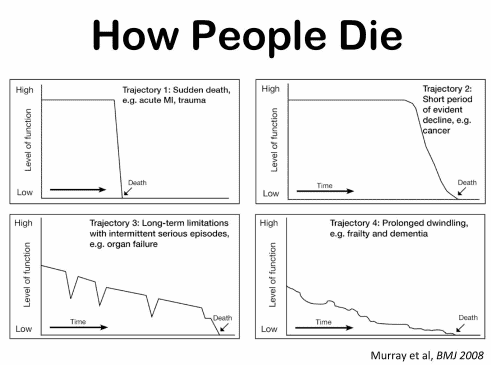
The progression of a terminal illness can vary depending on the type of illness, the person’s age, health, and treatment options. However, some common signs and symptoms indicate that the illness is advancing and the person is approaching the end of life. These signs and symptoms can help you and your loved one prepare for what will come and make the most of the remaining time together.
Some signs and symptoms of terminal illness progression are physical, such as appetite, weight, energy, and mobility changes. Others are emotional, psychological, or spiritual, such as changes in mood, cognition, communication, and beliefs. These signs and symptoms may not occur in a predictable order or simultaneously for everyone. Depending on the person’s condition and treatment, they may fluctuate over time. Therefore, monitoring the person’s condition closely and regularly communicating with their healthcare team is essential.
Six Months or Less to Live
As a terminal illness progresses, certain changes become more common. Around six months before the end of life, you may notice some of the following signs and symptoms:
- Decreased Appetite: Your loved one might show less interest in eating. They may have difficulty swallowing, chewing, or digesting food. They may also experience nausea, vomiting, or constipation. This can lead to dehydration and malnutrition. You can try to offer them small, frequent, and easy-to-eat meals that are high in calories and protein. You can also give them fluids, ice chips, or popsicles to keep them hydrated. However, do not force them to eat or drink if they do not want to. Respect their wishes and preferences. Eating and drinking less may make them more comfortable and reduce the burden on their organs.
- Fatigue: They may become increasingly tired and need more rest. They may have less energy and motivation to do things. They may also have difficulty breathing, especially when lying down. This can affect their quality of life and ability to enjoy activities. You can help them by comfortably arranging their bed or chair, using pillows, blankets, or fans. You can also encourage them to do gentle exercises, such as stretching, walking, or breathing, to improve their circulation and oxygen levels. However, do not push them to do more than they can or want to. Allow them to rest when needed and respect their pace and limits.
- Weight Loss: Significant loss of body weight over the past few months. This can be due to decreased appetite, increased metabolism, or muscle wasting. This can make them look thinner, weaker, and frailer. It can also affect their immune system and increase their risk of infections and complications. You can try to help them maintain their weight by offering them nutritious and appealing foods and drinks. You can also use supplements, vitamins, or medications as their doctor prescribes. However, do not be alarmed or upset if they continue to lose weight. This is a natural part of the dying process and does not mean that they are starving or suffering.
- Physical Decline: A decline in their overall physical abilities and activities. They may have more pain, discomfort, or symptoms related to their illness. They may also have difficulty moving, walking, or performing daily tasks. They may need more assistance and care from you or others. You can help them with pain relief, comfort measures, and supportive devices like a wheelchair, walker, or cane. You can also assist them with personal hygiene, dressing, feeding, and toileting. However, do not do everything for them. Allow them to do as much as they can and want to. Respect their dignity and autonomy.
- Increased Sleep: Spending more time sleeping or in bed (12 to 16 hours per day is typical). They may also become less alert, responsive, or coherent when awake. They may struggle to recognize you or others, remember things, or make decisions. They may also experience confusion, hallucinations, or delusions. This can be due to changes in their brain function, medication side effects, or lack of oxygen. You can help them by creating a calm, quiet environment using soft lighting, music, or aromatherapy. You can also talk to them, touch them, or hold their hand, even if they do not hear or understand you. However, do not try to correct, argue with, or force them to stay awake. Accept their reality and follow their lead.
Three Months or Less to Live
As the illness advances, these signs and symptoms may become more pronounced:
- Pain: Physical discomfort may increase, leading to grimacing, fidgeting, or moaning. This can be due to the progression of the disease, inflammation, infection, or pressure on the nerves or organs. Pain can affect the person’s mood, sleep, and quality of life. You can help them by giving them pain medication as their doctor prescribes, using non-medical methods such as massage, heat, cold, or distraction, and reporting any changes or concerns to their healthcare team. However, please do not assume they are always in pain or need more medication. Ask them how they feel and what they need. Respect their choices and preferences.
- Emotional Distress: Feelings of nervousness, anxiety, or confusion might arise. This can be due to the fear of death, the loss of control, the uncertainty of the future, or the changes in brain function. Emotional distress can affect a person’s behavior, communication, and relationships. You can help them by providing emotional support, listening to them, validating their feelings, and reassuring them that they are not alone. You can also seek professional help from a counselor, therapist, or chaplain if needed. However, do not judge, dismiss, or try to fix them. Accept them as they are and be there for them.
- Withdrawal: They might become less engaged with others and more focused inward. This can be due to the loss of interest, the lack of energy, or the preparation for death. Withdrawal can affect the person’s social and spiritual needs. You can help them by respecting their need for solitude, giving them space and privacy, and letting them know you are available if they want to talk or spend time with you. You can also encourage them to connect with their loved ones, friends, or faith community. However, do not take their withdrawal personally, force them to socialize, or make them feel guilty. Understand that this is a natural and normal part of the dying process.
- Restlessness: Agitation and restlessness could become more noticeable. This can be due to discomfort, anxiety, confusion, or unresolved issues. Restlessness can affect the person’s safety, comfort, and peace of mind. You can help them by creating a calm and soothing environment, using soft music, gentle touch, or aromatherapy. You can also try to identify and address the probable causes of their restlessness, such as pain, medication, environment, or emotional needs. However, do not restrain or argue with or scold them. Be patient, gentle, and compassionate with them.
- Sleeping more: Sleeping and napping tend to be around 14 to 18 hours per day. This can be due to fatigue, medication, or the body shutting down. Sleeping more can affect the person’s awareness, responsiveness, and communication. You can help them by making them comfortable, adjusting their position, and keeping them clean and dry. You can also talk to them, read to them, or play their favorite music, even if they do not seem to respond. However, do not wake them up, shout at them, or assume they cannot hear you. Believe that they can sense your presence and love.
One Month or Less to Live
In the final weeks, you may observe:
- Cognitive Changes: A decrease in cognitive ability and concentration. This can be due to the reduced blood flow to the brain, medication effects, or metabolic changes. Cognitive changes can affect a person’s memory, judgment, logic, and awareness. You can help them by speaking clearly and simply, using short sentences and familiar words, repeating essential information, and giving them time to process and respond. You can also remind them who you are, where they are, and what day it is. However, do not quiz them, correct them, or expect them to remember everything. Be flexible, understanding, and respectful of their reality.
- Changes in Breathing: Breathing patterns may become irregular or more labored. This can be due to the fluid buildup in the lungs, the weakness of the respiratory muscles, or the pressure on the chest. Breathing changes can affect the person’s oxygen level, comfort, and anxiety. You can help them by elevating their head, using a fan or humidifier, or giving them oxygen as their doctor prescribes. You can also reassure them, calm them, and breathe with them. However, please do not panic, force them to cough, or give them fluids or medications without consulting their health care team.
- Hallucinations: Visions or hallucinations might occur. This can be due to changes in brain function, medication effects, or spiritual experiences. Hallucinations can affect a person’s perception, emotion, and communication. You can help them by listening to them, acknowledging their expertise, and asking them what they see or hear. You can also try to comfort them, distract them, or join them in their vision if it is positive. However, do not dismiss them, argue with them, or try to rationalize them. Accept their experience and follow their lead.
- Loss of Appetite: Appetite further diminishes. This can be due to the reduced need for food and fluids, difficulty swallowing or digesting, or loss of taste or smell. Loss of appetite can affect the person’s hydration, nutrition, and comfort. You can help them by offering them small, soft, moist foods and drinks they like. You can moisten their mouth, lips, and eyes with water, ice, or gel. However, please do not force them to eat or drink, use a feeding tube, or give them intravenous fluids without consulting their healthcare team.
- Skin Changes: Skin temperature and color may fluctuate. This can be due to poor circulation, reduced blood pressure, or organ failure. Skin changes can affect the person’s warmth, sensation, and appearance. You can help them by keeping them warm, dry, and clean using blankets, pads, or wipes. You can gently massage their hands, feet, or back using lotion or oil. However, do not use electric blankets, heating pads, or alcohol-based products, as they may cause burns or irritation.
- Sleeping more: Sleeping and napping tend to be around 20+ hours per day. This can be due to exhaustion, medication effects, or the body shutting down. Sleeping more can affect the person’s awareness, responsiveness, and communication. You can help them by making them comfortable, adjusting their position, and keeping them clean and dry. You can also talk to them, read to them, or play their favorite music, even if they do not seem to respond. However, do not wake them up, shout at them, or assume they cannot hear you. Believe that they can sense your presence and love.
Two Weeks or Less to Live
In the last two weeks, the following changes might occur:
- Inactivity: Decreased activity and loss of function. This can be due to weakness, fatigue, or paralysis of the muscles and nerves. Inactivity can affect a person’s mobility, posture, and comfort. You can help them by supporting their body with pillows, cushions, or wedges, using a bedpan, catheter, or diaper, and turning them every two hours to prevent bedsores. You can also gently move their limbs, massage their muscles, or apply warm compresses to ease their stiffness and pain. However, please do not force them to move, sit, or stand up. Allow them to rest and relax in their preferred position.
- Communication: Difficulty in talking and expressing thoughts. This can be due to the reduced blood flow to the brain, the mouth’s dryness, or the vocal cords’ weakness. Communication can affect the person’s cognition, emotion, and interaction. You can help them by speaking softly and slowly, using simple and direct questions, and giving them time to respond. You can also use non-verbal cues, such as eye contact, facial expressions, or gestures, to communicate with them. However, please do not ignore them, interrupt them, or finish their sentences. Listen to them, understand them, and respect them.
- Congestion: Congestion in the lungs or throat could lead to changes in breathing. This can be due to the accumulation of mucus, saliva, or blood in the airways, the infection or inflammation of the lungs, or the relaxation of the throat muscles. Congestion can affect the person’s oxygen level, comfort, and sound. You can help them by raising their head, suctioning their mouth, or giving them medication as prescribed by their doctor. You can also reassure them, calm them, and breathe with them. However, please do not panic, force them to cough, or give them fluids or medications without consulting their health care team.
- Sleeping more: Sleeping and napping tend to be around 22+ hours per day. This can be due to exhaustion, medication effects, or the body shutting down. Sleeping more can affect the person’s awareness, responsiveness, and communication. You can help them by making them comfortable, adjusting their position, and keeping them clean and dry. You can also talk to them, read to them, or play their favorite music, even if they do not seem to respond. However, do not wake them up, shout at them, or assume they cannot hear you. Believe that they can sense your presence and love.
Last Days of Life
In the final days, expect:
- Withdrawal from the External World: Increased isolation and disengagement. This can be due to the loss of interest, the lack of energy, or the preparation for death. Withdrawal from the external world can affect the person’s social and spiritual needs. You can help them by respecting their need for solitude, giving them space and privacy, and letting them know you are available if they want to talk or spend time with you. You can also encourage them to connect with their loved ones, friends, or faith community. However, do not take their withdrawal personally, force them to socialize, or make them feel guilty. Understand that this is a natural and normal part of the dying process.
- Loss of Appetite: Appetite may cease entirely. This can be due to the reduced need for food and fluids, difficulty swallowing or digesting, or loss of taste or smell. Loss of appetite can affect the person’s hydration, nutrition, and comfort. You can help them by offering them small, soft, moist foods and drinks they like. You can moisten their mouth, lips, and eyes with water, ice, or gel. However, please do not force them to eat or drink, use a feeding tube, or give them intravenous fluids without consulting their healthcare team.
- Change in Bowel and Bladder Functions: Bowel and bladder functions may change. This can be due to the decreased intake of food and fluids, the reduced activity of the digestive system, or the loss of muscle control. Changes in bowel and bladder functions can affect the person’s hygiene, comfort, and dignity. You can help them by using a bedpan, catheter, or diaper, keeping them clean and dry, and applying cream or powder to prevent rashes or infections. However, do not be embarrassed, disgusted, or angry. Be gentle, respectful, and supportive of them.
- Confusion: Confusion and disorientation could become more prominent. This can be due to the reduced blood flow to the brain, medication effects, or metabolic changes. Confusion can affect the person’s memory, judgment, logic, and awareness. You can help them by speaking clearly and simply, using short sentences and familiar words, repeating vital information, and giving them time to process and respond. You can also remind them who you are, where they are, and what day it is. However, do not quiz them, correct them, or expect them to remember everything. Be flexible, understanding, and respectful of their reality.
- Visions: Visions and hallucinations might occur. This can be due to changes in brain function, medication effects, or spiritual experiences. Visions can affect a person’s perception, emotion, and communication. You can help them by listening to them, acknowledging their experience, and asking them what they see or hear. You can also try to comfort them, distract them, or join them in their vision if it is positive. However, do not dismiss them, argue with them, or try to rationalize them. Accept their experience and follow their lead.
- Sleeping more: Sleeping and napping tend to be around 23+ hours per day to not waking up at all. This can be due to exhaustion, medication effects, or the body shutting down. Sleeping more can affect the person’s awareness, responsiveness, and communication. You can help them by making them comfortable, adjusting their position, and keeping them clean and dry. You can also talk to them, read to them, or play their favorite music, even if they do not seem to respond. However, do not wake them up, shout at them, or assume they cannot hear you. Believe that they can sense your presence and love.
Remember, Every Journey is Unique
You may notice These signs and symptoms in your loved one as they approach the end of life. They may not experience all of them the same way and may also have other signs and symptoms not listed here. Therefore, consulting with their doctor or hospice team for more specific and personalized information and guidance is essential.
Conclusion
Terminal illness is a disease or condition that cannot be cured and is expected to lead to death within a certain period. The progression of a terminal illness can vary depending on the type of illness, the person’s age, health, and treatment options. However, some common signs and symptoms indicate that the illness is advancing and the person is approaching the end of life. These signs and symptoms can help you and your loved one prepare for what will come and make the most of the remaining time together.
Some signs and symptoms of terminal illness progression are physical, such as appetite, weight, energy, and mobility changes. Others are emotional, psychological, or spiritual, such as changes in mood, cognition, communication, and beliefs. These signs and symptoms may not occur in a predictable order or simultaneously for everyone. Depending on the person’s condition and treatment, they may fluctuate over time. Therefore, monitoring the person’s condition closely and regularly communicating with their healthcare team is essential.
As the person nears the end of life, they may experience more pronounced and noticeable changes, such as increased pain, fatigue, confusion, restlessness, and sleep. They may also withdraw from the external world, lose their appetite, have difficulty breathing, and see visions or hallucinations. These changes are natural and normal parts of the dying process and do not mean the person is suffering or starving. You can help them with pain relief, comfort measures, emotional support, and spiritual care. You can also respect their wishes, preferences, and choices.
I hope that this information has been helpful and informative for you. This is an exceedingly difficult and emotional time for you and your loved one. I want you to know that you are not alone. Many resources and support services are available for you and your loved one, such as hospice care, palliative care, counseling, support groups, and spiritual care. You can ask your doctor or hospice team for more information and referrals.
Resources
The Importance of Caregiver Journaling
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
The Last Hours of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying