Understanding ME/CFS: A Caregiver’s Guide to Non-Medical Support and End-of-Life Care
Published on June 20, 2025
Updated on June 20, 2025
Published on June 20, 2025
Updated on June 20, 2025
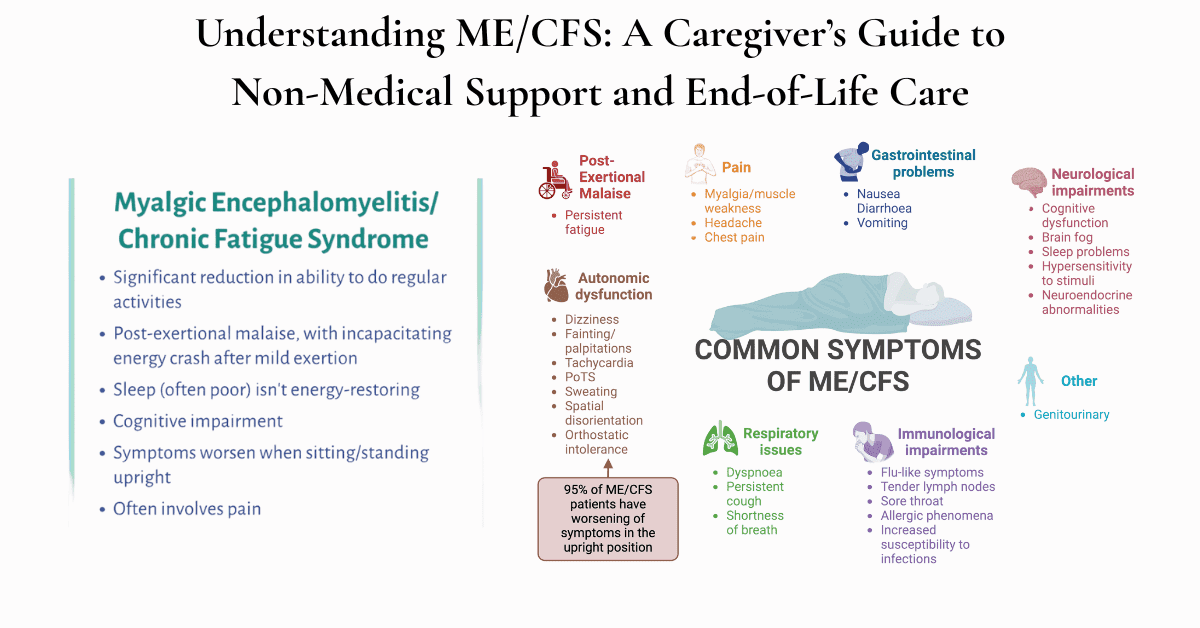
Table of Contents
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a serious, long-term illness that affects multiple body systems. This complex condition goes far beyond normal tiredness and can leave patients severely disabled for years or even decades.
The core symptoms that define ME/CFS include:
Many patients also experience chronic pain, sensitivity to light and sound, dizziness, and heart rate problems. These symptoms can fluctuate daily, making the condition unpredictable and challenging to manage.
Why understanding ME/CFS matters for everyone: Whether you’re a healthcare professional, patient, caregiver, or family member, understanding ME/CFS is crucial because it affects every aspect of daily life. Patients may require specialized care approaches that prioritize comfort and quality of life. Some become completely bedbound and require total care for basic needs like eating, bathing, and communication. The most severely affected patients face increased mortality risks and may benefit from palliative care services earlier in their disease journey than with other conditions.
For healthcare professionals, this knowledge enables them to provide better care, as ME/CFS patients often have unique needs related to environmental sensitivities, energy management, and symptom control. For patients and families, understanding the condition helps with advocacy, care planning, and making informed decisions about treatment approaches.
ME/CFS is often called an “invisible disability” because patients may look healthy on the outside while experiencing devastating symptoms internally. This creates several challenges that impact patients, families, and even healthcare providers:
Common misunderstandings include:
The impact on patients and families is profound. Many patients lose their careers, relationships, and independence. Families often struggle with financial hardship, social isolation, and the stress of caregiving. Children may miss years of school, and adults may become utterly dependent on others for basic care. The lack of understanding from healthcare providers, friends, and even family members can lead to additional trauma and delayed access to appropriate care.
For everyone involved in ME/CFS care – whether you’re a patient learning about your condition, a family member trying to understand what your loved one is experiencing, a caregiver providing daily support, or a healthcare professional working with ME/CFS patients – recognizing these challenges is the first step toward giving compassionate, informed care that validates the patient’s experience and supports everyone through what may be a long and challenging journey.
ME/CFS affects people differently, and understanding these severity levels helps everyone involved make better decisions about care and support. The condition is typically classified into four primary severity levels, each with distinct characteristics and care needs.
Mild ME/CFS allows patients to maintain some daily activities, though they may need to reduce work hours or give up certain hobbies. These individuals can usually care for themselves and may still be able to work part-time or attend school with accommodations. However, they often use all their available energy for essential activities, such as work, leaving little energy for social activities or household tasks.
Moderate ME/CFS significantly impacts daily functioning. Patients typically cannot work full-time or attend school regularly. They may be mobile, but often need to rest frequently and may use mobility aids, such as wheelchairs, for longer distances. Many people at this level can still live independently with some support, but have significantly reduced social and recreational activities.
Severe ME/CFS leaves patients mostly housebound or bedbound for significant portions of the day. They require assistance with basic activities, such as shopping, cooking, and sometimes personal care. Cognitive symptoms become more pronounced, making it difficult to concentrate, read, or follow conversations. Light and sound sensitivity often require patients to spend time in darkened, quiet rooms.
Very Severe ME/CFS represents the most debilitating form of the condition. These patients are typically bedbound 24 hours a day and may need tube feeding, assistance with all personal care, and constant quiet, darkened environments. Some cannot tolerate any light or sound and may need to communicate through simple gestures or written notes. This level requires full-time caregiving support.
The progression of ME/CFS varies significantly between individuals. Some people experience a gradual decline over months or years, while others may have sudden crashes that leave them at a more severe level. Understanding these patterns helps families and healthcare providers plan appropriate care.
Common decline patterns include:
Factors that can trigger decline include:
The early phase (first 1-2 years) often involves the most dramatic changes as patients and families adjust to the new reality of living with ME/CFS. During this time, many people are still seeking a diagnosis and trying various treatments. The focus should be on learning about the condition, establishing effective pacing strategies, and building a support system.
The chronic phase (2- 10+ years) typically involves finding a new normal and developing long-term management strategies. Some patients may experience slight improvements with careful management, while others continue to decline. This phase often requires ongoing adjustments to living situations, relationships, and care needs.
The advanced phase occurs when patients have lived with severe or very severe ME/CFS for many years. During this time, complications may develop, and the focus often shifts toward comfort care and quality of life rather than attempting to improve function.
End-of-life care may become appropriate for ME/CFS patients earlier than many people expect. While ME/CFS itself is not typically considered a terminal illness, patients with very severe ME/CFS face increased mortality risks and may benefit from palliative or hospice care approaches.
Situations where end-of-life care should be considered:
Recognizing signs of decline helps families and healthcare providers respond appropriately and consider additional support services. These indicators don’t necessarily mean death is imminent, but they suggest that more intensive support may be needed.
| Physical Indicators | Cognitive Indicators | Functional Indicators |
|---|---|---|
| Increased time bedbound | Severe brain fog | Loss of independence in daily tasks |
| Difficulty swallowing or eating | Memory problems | Need for full-time care |
| Frequent infections | Communication difficulties | Unable to tolerate visitors |
| Cardiovascular complications | Confusion or disorientation | Extreme environmental sensitivities |
| Significant weight loss | Inability to make decisions | Complete social isolation |
When these indicators appear, it’s important to:
Understanding the ME/CFS disease trajectory helps everyone involved make informed decisions about care, set realistic expectations, and ensure that patients receive appropriate support at every stage of their journey. Whether you’re a patient, family member, caregiver, or healthcare professional, recognizing these patterns enables better planning and more compassionate care.
Post-exertional malaise (PEM) is the hallmark symptom of ME/CFS and the most important concept for everyone to understand. PEM occurs when a person with ME/CFS uses more energy than their body can handle, leading to a significant worsening of all symptoms. This isn’t the usual tiredness that healthy people feel after exercise or a busy day – it’s a severe crash that can last days, weeks, or even months.
What makes PEM different from normal fatigue:
Common triggers for PEM include:
Understanding PEM is crucial because the goal of pacing is to prevent these crashes from happening. When patients avoid PEM, they often feel more stable and may even experience gradual improvements over time.
Pacing means staying within the person’s “energy envelope” – the amount of energy they have available each day without triggering post-exertional malaise (PEM). As a caregiver, family member, or healthcare provider, you can help by learning and supporting these techniques.
The 50% Rule is a good starting point for pacing. If someone thinks they can do an activity for 20 minutes, they should only do it for 10 minutes. This leaves energy in reserve and helps prevent crashes. Many people with ME/CFS overestimate their abilities because they remember what they could do before becoming ill.
Breaking activities into smaller pieces makes tasks more manageable. Instead of cleaning an entire room, the person might dust one shelf, rest, and then vacuum one small area later. Instead of cooking a full meal, they might prepare one ingredient, rest, then continue when they feel able.
Rest breaks should be planned, not just taken when exhausted. Encourage rest periods between activities, even if the person feels okay. These breaks might involve lying down, sitting quietly, or doing gentle breathing exercises. The key is stopping before symptoms worsen.
Activity rotation helps distribute different types of energy use throughout the day. If someone performs a mental task, such as paying bills, the next activity should be physical but gentle, like folding laundry while sitting. This prevents overreliance on a single type of energy.
Tracking energy and symptoms helps identify patterns and limits. Simple logs noting activities, energy levels, and symptoms can reveal what triggers crashes and what activities are manageable. Many people use smartphone apps or simple paper charts for this purpose.
The physical environment plays a considerable role in ME/CFS symptom management. Minor adjustments to living spaces can significantly enhance comfort and functionality for patients while reducing the burden on caregivers.
The bedroom should be the primary focus since many ME/CFS patients spend considerable time there. Keep this space as comfortable as possible with blackout curtains or eye masks for light sensitivity, noise-reducing materials such as heavy curtains or a white noise machine, and comfortable temperature control, as many patients struggle to regulate their body temperature.
Essential items should be within easy reach to minimize energy expenditure. This includes water bottles, medications, tissues, communication devices, and comfort items like pillows or blankets. A bedside table or rolling cart can keep necessities organized and accessible.
Bathroom modifications often become necessary as the condition progresses. Consider installing grab bars, shower chairs, raised toilet seats, and non-slip mats to enhance safety and accessibility. A handheld showerhead and long-handled sponges can make bathing easier and safer.
Kitchen adaptations help maintain some independence with food preparation. Lightweight dishes, ergonomic utensils, a rolling cart for transporting items, and organizing frequently used items at waist level can all help reduce the energy required for meal preparation.
Many people with ME/CFS develop severe sensitivities to light, sound, touch, and smell that can trigger symptoms or worsen existing ones. Managing these sensitivities is essential for comfort and preventing symptom flares.
Light sensitivity management:
Sound sensitivity solutions:
Managing other sensitivities:
Personal care needs vary greatly depending on the severity of ME/CFS, but even those with milder forms may need help during symptom flares. Understanding how to provide this assistance with dignity and efficiency benefits everyone involved.
Bathing and hygiene support may range from simple assistance to complete care. For those who can shower independently, consider shower chairs, grab bars, and handheld showerheads. Some patients may require assistance with washing their hair or accessing certain areas. For bedbound patients, bed baths, dry shampoo, and no-rinse cleansing products can maintain hygiene with less energy expenditure.
Dressing assistance should focus on comfort and ease. Choose clothing that’s easy to put on and take off, such as items with front closures, elastic waistbands, and soft fabrics. Compression garments may help some patients with circulation issues, while others may find any tight clothing uncomfortable.
Medication management becomes crucial as many ME/CFS patients take multiple medications and supplements. Pill organizers, medication reminders, and keeping a current medication list help ensure nothing is missed. Some patients may require assistance with opening bottles or remembering to take medications during episodes of cognitive fog.
Effective communication becomes more challenging as ME/CFS progresses, especially during symptom flares when cognitive function is impaired. Developing good communication strategies helps reduce frustration and ensures essential information is shared.
During conversations:
For non-verbal communication:
Supporting cognitive function:
Mobility needs in ME/CFS can change rapidly depending on symptom severity and energy levels. Planning for various scenarios helps maintain safety and independence.
| Mobility Level | Helpful Equipment | Safety Considerations |
|---|---|---|
| Walking with fatigue | Lightweight cane, folding chair for rest breaks | Monitor for overexertion signs |
| Limited walking | Walker with seat, wheelchair for longer distances | Clear pathways, remove trip hazards |
| Primarily wheelchair | Manual or electric wheelchair, transfer aids | Accessible bathroom, ramps if needed |
| Bedbound | Hospital bed, lift equipment, pressure-relief mattress | Fall prevention, skin care, positioning |
Home accessibility modifications may include installing ramps, widening doorways, lowering light switches and door handles, adding stair lifts or platform lifts, and creating accessible bathroom facilities. Many of these modifications can be temporary or adjustable as needs change.
Transportation considerations become important for medical appointments and essential errands. This may involve using wheelchair-accessible vehicles, planning rest stops during longer trips, considering medical transportation services, or arranging for others to handle errands when possible.
Planning for emergencies is especially crucial for individuals with ME/CFS, as they may not be able to respond quickly to urgent situations. Keep emergency contact information easily accessible, ensure medical information is readily available for first responders, have backup power for essential medical equipment, and establish communication plans with neighbors or family members who can regularly check on the patient.
These non-medical support strategies form the foundation of good ME/CFS care. While they may seem simple, implementing them thoughtfully and consistently can dramatically improve the quality of life for patients and reduce stress for caregivers and families. Remember that needs may change over time, so regular reassessment and adjustment of these strategies are essential for optimal support.
Palliative care focuses on improving the quality of life and managing symptoms for people with serious illnesses. It can be appropriate for ME/CFS patients much earlier than many people realize. Unlike hospice care, palliative care can be provided alongside treatments aimed at improving the condition and doesn’t require a terminal prognosis.
When ME/CFS symptoms become severe and complex to manage, palliative care can provide specialized expertise in symptom control. This is especially important because ME/CFS involves multiple, complex symptoms that often don’t respond well to standard treatments.
Signs that symptom burden may warrant palliative care:
Breathing difficulties, heart rate problems, and digestive issues are also common in severe ME/CFS and may benefit from palliative care approaches. The key is recognizing when symptoms are causing significant suffering despite best efforts at management.
Functional decline in ME/CFS can happen gradually or suddenly, and recognizing these changes helps determine when additional support is needed. Palliative care teams are skilled at helping families navigate these transitions and adjust care plans accordingly.
Important functional decline markers include:
The rate of decline also matters. Some people with ME/CFS remain stable at one functional level for years, while others experience rapid changes that require quick adjustments to care plans. Palliative care teams can help families prepare for and manage these transitions.
Quality of life is deeply personal, and what matters most varies from person to person. Palliative care teams excel at helping patients and their families identify what is most important and finding ways to preserve or improve those aspects of life.
Common quality of life concerns in ME/CFS:
Palliative care can help address these concerns through counseling, spiritual care, social work services, and practical support. The goal isn’t necessarily to fix these problems but to help people find ways to cope and maintain dignity and meaning despite their limitations.
Hospice care is designed for people with a life expectancy of six months or less, but determining this timeline can be challenging with ME/CFS. Unlike cancer or heart disease, ME/CFS doesn’t follow predictable patterns, making prognosis difficult to determine.
Factors that may indicate hospice appropriateness:
The decision to pursue hospice care should involve honest discussions among patients, their families, and healthcare providers about goals, values, and what constitutes an acceptable quality of life. Some families may choose hospice care even when the prognosis is uncertain if the focus shifts to comfort rather than attempting to improve function.
ME/CFS patients have specific needs that differ from those of other hospice patients, and understanding these differences helps ensure the provision of appropriate care planning.
Environmental sensitivities are often extreme in severe ME/CFS, requiring hospice teams to modify their usual approaches. This might mean limiting the number of staff members who visit, using fragrance-free products, keeping voices low, and dimming lights during visits.
Communication challenges may require creative solutions. Some patients can only communicate through writing, gestures, or brief whispered words. Hospice teams must be patient and develop individualized communication strategies tailored to each patient.
Family dynamics in ME/CFS often involve years of caregiving stress, financial hardship, and social isolation. Families may be exhausted, grieving multiple losses, and struggling with complex emotions about the disease progression. Hospice social workers and counselors need to understand this unique context.
Medication sensitivities are common in ME/CFS, and patients may react poorly to standard hospice medications. Close monitoring and individualized medication plans are often necessary.
Palliative and hospice care teams bring specialized expertise in managing complex symptoms that can significantly improve comfort for ME/CFS patients.
Pain management often requires creative approaches since ME/CFS patients may be sensitive to many medications. This might include low-dose medications, topical treatments, positioning techniques, and environmental modifications to reduce pain triggers.
Nausea and digestive issues can be addressed through medication, dietary modifications, and alternative approaches such as acupressure or aromatherapy. The goal is to find what works for each individual patient.
Sleep disturbances may improve with sleep hygiene education, environmental modifications, and carefully chosen sleep aids that don’t worsen other ME/CFS symptoms.
Anxiety and depression are common in ME/CFS and can be addressed through counseling, support groups, medications when appropriate, and spiritual care.
Palliative and hospice care recognize that the family is the unit of care, not just the patient. This is especially important in ME/CFS, where family members often serve as primary caregivers for extended periods.
| Support Service | How It Helps ME/CFS Families |
|---|---|
| Respite Care | Provides temporary relief for exhausted caregivers |
| Counseling Services | Helps process grief, stress, and relationship changes |
| Support Groups | Connects families with others facing similar challenges |
| Social Work Services | Assists with financial resources and practical needs |
| Bereavement Support | Continues support after the patient’s death |
Education and training help family members feel more confident in providing care, understanding what to expect, and knowing when to seek additional help.
24/7 availability provides peace of mind for families who may feel overwhelmed by the responsibility of caring for someone with complex needs.
Palliative and hospice care teams can help create optimal environments for ME/CFS patients while working within the constraints of the home setting.
Lighting modifications might include providing special bulbs, light filters, or blackout materials to reduce light sensitivity. Some hospice programs can arrange for these accommodations as part of their services.
Sound management involves training staff and volunteers to speak quietly, move carefully to avoid sudden noises, and respect the patient’s need for quiet and calm.
Air quality considerations include using fragrance-free products, ensuring good ventilation, and being aware of how cleaning products or medical equipment might affect sensitive patients.
Equipment and supplies provided by hospice programs can be modified to meet the needs of ME/CFS patients. This may include specialized mattresses for pressure relief, quiet medical equipment, or adaptive devices that require minimal energy to operate.
Scheduling flexibility allows visits to be timed when patients feel best and can be shortened or postponed during symptom flares. This individualized approach recognizes that ME/CFS symptoms can be unpredictable.
The decision to pursue palliative or hospice care for ME/CFS patients requires careful consideration of individual circumstances, values, and goals. These services can provide valuable support for managing complex symptoms, supporting families, and maintaining dignity and comfort throughout the disease journey. Whether you’re a patient, family member, caregiver, or healthcare professional, understanding these options helps ensure that appropriate care is available when needed.
Caring for someone with ME/CFS can be emotionally and physically exhausting, especially when the caregiving role continues for months or years. Many caregivers don’t recognize when they’re experiencing burnout because they’re so focused on their loved one’s needs that they ignore their own warning signs.
Common signs of caregiver stress include:
The unique challenges of ME/CFS caregiving make burnout especially common. Unlike other conditions where patients may gradually improve, ME/CFS often involves unpredictable symptoms, long-term disability, and limited treatment options. Caregivers may feel helpless watching their loved one suffer while dealing with financial stress, social isolation, and the physical demands of providing care.
Recognizing these feelings is normal and doesn’t mean you’re failing as a caregiver. The stress of watching someone you love struggle with a poorly understood condition while managing complex care needs would challenge anyone. Acknowledging caregiver stress is the first step toward getting the support you need.
Taking care of yourself isn’t selfish – it’s essential for providing good care to your loved one. When caregivers are exhausted and stressed, they’re more likely to make mistakes, become impatient, or develop health problems that prevent them from continuing their caregiving role.
Practical self-care strategies include:
Creating a support network is crucial for long-term caregiving success. This might include family members who can provide respite care, friends who offer emotional support, neighbors who help with errands, or professional services that assist with caregiving tasks. Don’t wait until you’re overwhelmed to ask for help – building these relationships early makes it easier to use them when needed.
Professional counseling can be extremely helpful for caregivers dealing with the complex emotions that come with ME/CFS caregiving. Many counselors specialize in chronic illness and can provide strategies for managing stress, grief, and relationship changes.
Education is one of the most powerful tools families have for supporting their loved one with ME/CFS. When family members understand the condition, they’re better able to provide appropriate support, avoid harmful suggestions, and advocate effectively with healthcare providers and others.
Key concepts for families to understand:
Common misconceptions to address include the belief that exercise will help (it often makes ME/CFS worse), that the person just needs to “push through” symptoms (this can cause severe crashes), or that positive thinking will cure the condition (while emotional support is essential, ME/CFS is a physical illness that requires medical management).
Learning about ME/CFS severity levels helps families understand what to expect and plan appropriate support. Someone with mild ME/CFS may need help with household tasks and emotional support, while someone with severe ME/CFS may require total care for basic needs like eating and personal hygiene.
Families often need to advocate for their loved one with ME/CFS because the condition is poorly understood by many healthcare providers, employers, schools, and social service agencies. Effective advocacy requires preparation, persistence, and clear communication.
Preparing for advocacy situations:
Effective advocacy strategies include:
Every day, advocacy situations include medical appointments where providers dismiss symptoms, workplace or school accommodation requests, disability benefit applications, and social situations where family members or friends don’t understand the condition’s impact.
Recognizing when professional help is needed can prevent caregiver burnout and ensure the patient receives appropriate care. Many families try to manage everything themselves until they reach a crisis point, but seeking help earlier often leads to better outcomes for everyone involved.
Signs that additional professional support may be needed:
Types of professional support that may be helpful:
Many communities have resources available to support families dealing with chronic illness, though finding and accessing these resources can be challenging. Starting with a few key organizations can help identify additional resources specific to your area and situation.
| Resource Type | Examples | How to Access |
|---|---|---|
| Medical Support | Palliative care programs, home health agencies, specialty clinics | Ask healthcare providers for referrals |
| Financial Assistance | Disability benefits, utility assistance, food banks, medication assistance programs | Contact social services or 211 helpline |
| Respite Care | Adult day programs, volunteer visitor programs, temporary home care | Search online or ask social workers |
| Support Groups | ME/CFS support groups, caregiver support groups, online communities | Check with hospitals, community centers, or online |
| Practical Help | Meal delivery, transportation services, housekeeping assistance | Contact faith communities, volunteer organizations |
National organizations that provide information and support for ME/CFS families include patient advocacy groups, organizations focused on chronic illnesses, and caregiver support networks. Many of these organizations provide online resources, support groups, and educational materials that can be accessed from the comfort of home.
Local resources might include community health centers, faith-based organizations, volunteer groups, and government programs. The 211 helpline (dial 2-1-1) is available in most areas and can provide information about local resources for families dealing with chronic illness.
Online resources have become increasingly crucial for ME/CFS families, particularly those who are homebound or reside in areas with limited local support. Online support groups, educational webinars, and virtual counseling services can provide valuable support and information.
Building relationships with resource providers before you need them makes it easier to access help during crisis situations. This might mean attending a support group meeting when things are stable, establishing relationships with respite care providers, or connecting with other families who have similar experiences.
Supporting caregivers and families is essential for successful ME/CFS management. Whether you’re a patient recognizing your family’s stress, a caregiver struggling with burnout, a family member trying to understand how to help, or a healthcare professional working with ME/CFS families, remember that seeking support is a sign of strength, not weakness. The challenges of ME/CFS affect the entire family system, and addressing these challenges with appropriate resources and support leads to better outcomes for everyone involved.
Understanding a person’s functional capacity helps everyone involved make better decisions about care, support needs, and when to seek additional help. Simple assessment tools can provide valuable information without overwhelming patients or families.
Basic functional assessment tools offer practical options: comprehensive questionnaires that evaluate multiple areas of daily functioning and shorter monitoring tools for regular check-ins. These tools examine key areas including personal hygiene, walking and movement, being upright, home activities, communication, outside activities, reactions to light and sound, and concentration.
Hours of upright activity provides a simple daily measure by tracking time spent with feet on the floor – walking, standing, and sitting. This straightforward approach helps identify patterns and changes in functional capacity over time, eliminating the need for complex calculations.
Quick daily indicators to monitor include:
Simple severity classifications help communicate needs: mild ME/CFS allows some work or school with accommodations, moderate ME/CFS significantly limits daily activities and may require mobility aids, severe ME/CFS leaves patients mostly housebound, and very severe ME/CFS requires bedbound care with total assistance.
Effective symptom tracking doesn’t need to be complicated, but consistency is key for identifying patterns and triggers. The goal is to gather useful information without creating an additional burden for patients or caregivers.
Essential elements to track daily:
Modern tracking options include smartphone apps that calculate daily stability scores using heart rate variability and simple daily questions, as well as general symptom-tracking apps that allow customization for ME/CFS-specific needs. For those preferring paper methods, simple daily logs or printable templates work equally well.
The key is finding a system that works for the individual situation. Some patients can manage detailed tracking, while others require assistance from family members or prefer very simple rating scales. The most important factor is consistency rather than complexity.
Having reliable resources readily available helps families navigate challenges and access appropriate support when needed. These organizations offer education, advocacy, and practical support for individuals with ME/CFS and their families.
| Organization Type | Examples | Services Provided |
|---|---|---|
| Patient Advocacy | MEAction, Solve ME/CFS Initiative | Research funding, policy advocacy, patient education |
| Medical Resources | Bateman Horne Center, Stanford ME/CFS Clinic | Clinical guidance, provider education, research |
| Support Communities | Health Rising, Science for ME | Information sharing, patient forums, updates |
| Self-Help Resources | CFIDS & Fibromyalgia Self Help | Online courses, educational materials, practical tools |
National organizations provide valuable resources, including educational materials, research updates, advocacy efforts, and connections to local support groups. Many offer online resources that can be accessed from home, which is especially important for patients who cannot travel to in-person meetings.
Local resources vary by community but may include support groups, respite care services, meal delivery programs, and transportation assistance. Contacting local hospitals, community health centers, or calling your local helpline can help identify available services in your area.
Online communities have become essential for many ME/CFS families, providing around-the-clock access to information, emotional support, and practical advice from others with similar experiences. These platforms can be particularly valuable for patients who are isolated and caregivers who are overwhelmed.
Emergency planning is crucial for ME/CFS patients because their unique needs may not be understood by emergency responders or hospital staff. Having essential information readily available can prevent complications and ensure appropriate care during medical crises.
Essential emergency preparations include:
Comprehensive emergency planning resources are available, including downloadable medical consideration letters for healthcare providers and detailed crash survival guides. These materials can be customized with personal information and kept readily available for emergency situations.
Key emergency considerations for ME/CFS patients include treating orthostatic symptoms aggressively with IV fluids, reducing sensory stimuli like bright lights and loud sounds, allowing patients to remain lying down when possible, and understanding that standard treatments may need modification. Having this information prepared in advance helps ensure that appropriate care is provided when patients may be too ill to advocate for themselves.
Family members and caregivers should be familiar with emergency plans and have copies of essential medical information. Regular review and updates of emergency supplies and information help ensure everything remains current and accessible when needed.
These practical tools offer immediate support for managing ME/CFS while laying the groundwork for longer-term care planning. Whether you’re a patient learning to track your symptoms, a family member trying to understand functional changes, a caregiver preparing for emergencies, or a healthcare professional working with ME/CFS patients, having these resources readily available can improve care quality and reduce stress during challenging situations.
ME/CFS is a serious, complex illness that requires compassionate understanding from everyone involved in patient care. Whether you’re a healthcare professional encountering ME/CFS patients for the first time, a family member trying to support your loved one, or a patient navigating this challenging condition yourself, recognition of the disease’s severity and impact is the foundation of good care.
The invisible nature of ME/CFS symptoms makes understanding especially important. Patients may appear healthy while experiencing devastating fatigue, pain, and cognitive difficulties that profoundly limit their daily functioning. Post-exertional malaise, the hallmark symptom of ME/CFS, means that activities most people take for granted can trigger severe symptom flares lasting days, weeks, or months.
True understanding goes beyond knowing the symptoms – it involves recognizing the profound losses patients and families experience, the social isolation that often accompanies the condition, and the unique challenges of managing an unpredictable, poorly understood illness. This understanding forms the basis for providing appropriate support and avoiding well-meaning but potentially harmful suggestions, such as “just push through it” or “exercise will help.”
Palliative and hospice care can provide valuable support for ME/CFS patients much earlier than many people realize. Unlike other conditions where these services are reserved for end-stage disease, ME/CFS patients may benefit from palliative care approaches when symptoms become severe and complex to manage, regardless of prognosis.
Consider palliative care when patients experience uncontrolled symptoms that significantly impact quality of life, functional decline that affects independence and safety, or when families are struggling with the complex care needs and emotional burden of the condition. Palliative care teams offer specialized expertise in symptom management, family support, and care coordination, which can enhance comfort and quality of life for both patients and their families.
Hospice care becomes appropriate when the focus shifts from attempting to improve function to maintaining comfort and dignity. This might occur when patients become completely bedbound with total care needs, experience frequent medical crises, or when families choose comfort-focused care over life-prolonging treatments. The decision should always involve honest discussions about goals, values, and what constitutes an acceptable quality of life for each individual situation.
Maintaining dignity and quality of life for ME/CFS patients requires individualized approaches that respect each person’s values, preferences, and remaining abilities. This means recognizing that the quality of life looks different for everyone. Some patients find meaning in small daily activities, while others focus on maintaining meaningful relationships or engaging in spiritual practices.
Practical support strategies that preserve dignity include respecting the patient’s need for environmental modifications, supporting their communication preferences and limitations, involving them in care decisions to the extent possible, and recognizing their expertise about their own condition and needs. Simple accommodations, such as dimming lights, speaking quietly, and allowing adequate time for responses, can make a significant difference in patient comfort and sense of dignity.
Quality of life extends beyond the patient to include family members and caregivers who are also affected by the condition. Supporting the entire family system through education, respite care, counseling services, and practical assistance helps ensure that everyone’s needs are met and that care can be sustained over time.
The journey with ME/CFS is often long and challenging. Still, with understanding, appropriate support, and compassionate care, patients can maintain dignity and find meaning even in the face of significant limitations. Whether providing professional care services, supporting a family member, or managing your own condition, remember that small acts of kindness, patience, and understanding can have profound impacts on quality of life and overall well-being.
The goal is not to cure ME/CFS, but to provide the best possible support, comfort, and care throughout the disease journey, honoring each person’s unique needs and preserving their dignity at every step.
American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society
American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society, a message for caregivers
Caring for the Patient with Severe or Very Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Onset patterns of chronic fatigue syndrome and myalgic encephalomyelitis
Prognosis for myalgic encephalomyelitis and chronic fatigue syndrome
Mortality in Patients with Myalgic Encephalomyelitis and Chronic Fatigue Syndrome
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an autoimmune disease
Other Supportive Strategies for Living with ME/CFS
Restorative Care Services for Patients with Chronic Fatigue
Shedding Light on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Functional Capacity in ME/CFS: an assessment questionnaire
Functional Assessment of ME/CFS Disability – WHODAS 2.0
Strategies to Prevent Worsening of Symptoms (of ME/CFS)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Holistic Nurse: Skills for Excellence book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series