Understanding Aggression in Elderly Patients with Dementia
Published on November 11, 2024
Updated on November 8, 2024
Published on November 11, 2024
Updated on November 8, 2024
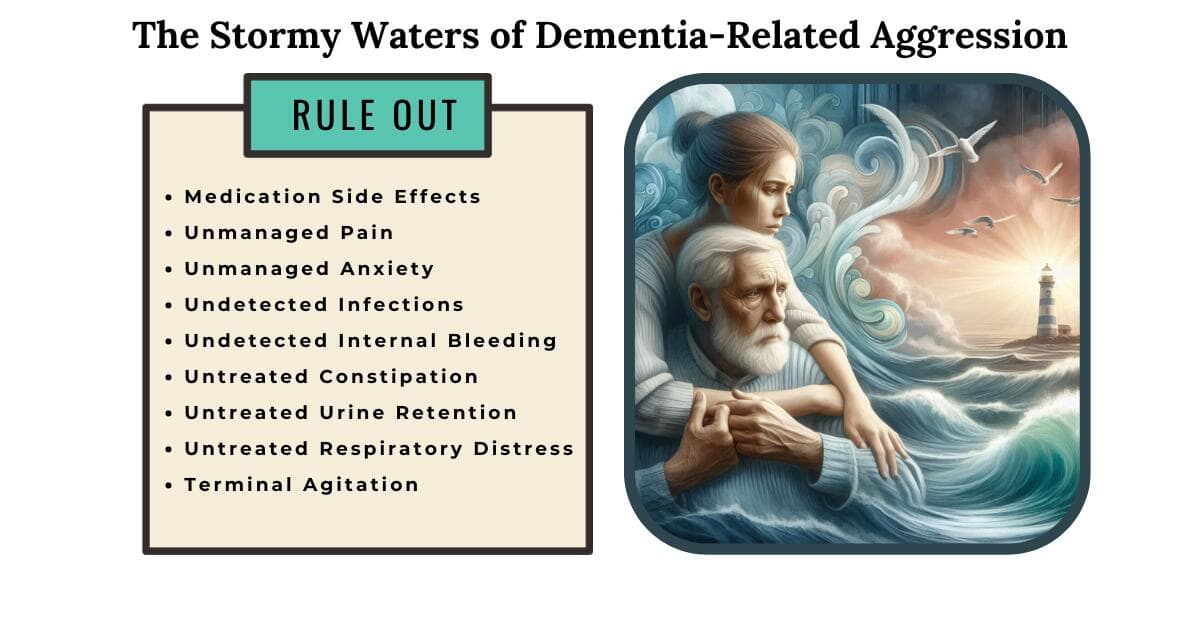
Table of Contents
Dementia is a condition that touches the lives of many older adults. It affects memory, thinking, and behavior, making everyday tasks more challenging. As we care for our loved ones, we encounter various aspects of dementia, including its impact on emotions and behavior.
Imagine a beautiful tapestry woven over a lifetime—a rich collection of memories, experiences, and relationships. Unfortunately, dementia begins to unravel this tapestry. It affects the brain, causing forgetfulness, confusion, and sometimes even fear. Our parents, grandparents, or dear friends may struggle to recognize us or recall shared moments. It’s like watching a cherished book lose its pages, one by one.
Now, let’s talk about something crucial: aggression. When dementia enters the picture, it can lead to unexpected outbursts. Your gentle grandmother might suddenly become upset or even lash out. It’s not her fault; it’s the dementia speaking. But these moments impact everyone involved—the patient, the family, and the caregivers.
So, let’s embark on this journey together. We’ll explore the reasons behind aggression, learn how to respond and find ways to ease the burden because every thread in our tapestry matters, and every act of kindness makes a difference.
Stay with us as we delve deeper into the world of dementia and aggression. Together, we’ll weave a more robust fabric of care and compassion.
Imagine a cherished family photo album with memories of birthdays, holidays, and shared laughter. Now, picture the pages fading, faces blurring, and names slipping away. Dementia does precisely that—it erases the familiar. Your dear one may look at you, searching for recognition, but find only confusion. Their once-clear memories now dance in the mist.
Dementia paints a surreal canvas. Imagine your loved one convinced that unseen enemies lurk in the shadows. They hear whispers, see faces that vanish, and feel the ground shift beneath their feet. Paranoia, delusion, and hallucinations—these are not mere words; they’re their daily companions.
Frontotemporal dementia (FTD) targets the brain’s control center—the frontal lobes. It’s like a storm brewing within. Impulsivity becomes their companion, and reason takes a back seat.
Dear caregivers, you’re the lighthouses in this storm—your love and understanding matter. As we explore these facets of dementia, remember that empathy is our compass. Together, we’ll navigate the uncharted waters, one wave at a time.
Our dear ones with dementia often face discomfort—aches, spasms, and unspoken pains. Imagine their frustration when words fail them. They can’t say, “My back hurts” or “My head throbs.” Instead, they express it through actions—sometimes with aggression.
Imagine a room filled with noise—chatter, clattering dishes, and blaring TV. For our loved ones with dementia, it’s overwhelming. Environmental triggers set off alarms in their minds, and sometimes, aggression follows.
Caregiving is a marathon, not a sprint. We juggle medications, appointments, and emotions. Sometimes, we’re the target of their frustration. Stress creeps in, and we feel overwhelmed.
Infections—tiny invaders—can wreak havoc. Undiagnosed infections add fuel to the fire of aggression. Imagine a fever brewing inside, confusing their senses.
Dear caregivers, you’re the anchors in this storm. Your love and resilience matter. As we explore these facets of dementia, remember that empathy is our compass. Together, we’ll navigate the uncharted waters, one wave at a time.
When a new medication enters the scene, it’s like adding a character to our loved one’s story. Assessing its impact becomes crucial. Here’s what you need to know:
Cholinesterase inhibitors—fancy words, but let’s break them down. Imagine a delicate balance in the brain—a dance of chemicals. These inhibitors aim to preserve that balance:
Imagine a journey. Cholinesterase inhibitors are companions along this road. But what happens when the road stretches too far?
Remember, dear caregivers, you’re the navigators. You hold the compass—their well-being. As we explore these medications, let empathy guide us. Each decision matters, and each step is taken with care.
Picture a table set for a feast—the aroma of warm soup and fresh vegetables’ colors. Now imagine our loved ones with dementia, their appetites waning. Poor food intake becomes a silent struggle:
Imagine a restless night—the clock ticking, shadows dancing. For our loved ones with dementia, sleep can be elusive. Aggression tiptoes in when sleep departs:
Imagine the bathroom—a place of privacy, vulnerability, and sometimes, confusion. Routine toileting becomes part of our caregiving landscape:
Dear caregivers, you’re the guardians of comfort—the keepers of these moments. Your love and patience matter. As we explore these facets of dementia care, let empathy guide us. Each act of kindness weaves a tapestry of compassion.
Aggression in dementia isn’t a single puzzle piece; it’s the entire mosaic—the colors, the shapes, the gaps. We can’t solve it with a single strategy. Instead, we embrace a holistic approach:
Caregivers, you’re the unsung heroes who hold hands, wipe tears, and carry the weight. Your journey is both beautiful and challenging:
As we close this chapter, remember that empathy is our compass. With each smile, touch, and whispered reassurance, we’re weaving a tapestry of care.
Thank you for being the lightkeepers who guide our loved ones through the storm. May your hearts find solace, and may your compassion continue to shine.
Assessment and Management of Dementia-Related Agitation
Pharmacologic Management of Agitation in Patients with Dementia
Alzheimer’s Violence, Aggression, Anger: Causes & Treatments
How long does the aggressive stage of dementia last?
Aggressive behavior and dementia
How to Respond to Anger and Aggression in Dementia
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?