Nebulized Morphine: A New Approach to Managing Shortness of Breath in Hospice Care
Published on October 15, 2025
Updated on October 11, 2025
Published on October 15, 2025
Updated on October 11, 2025
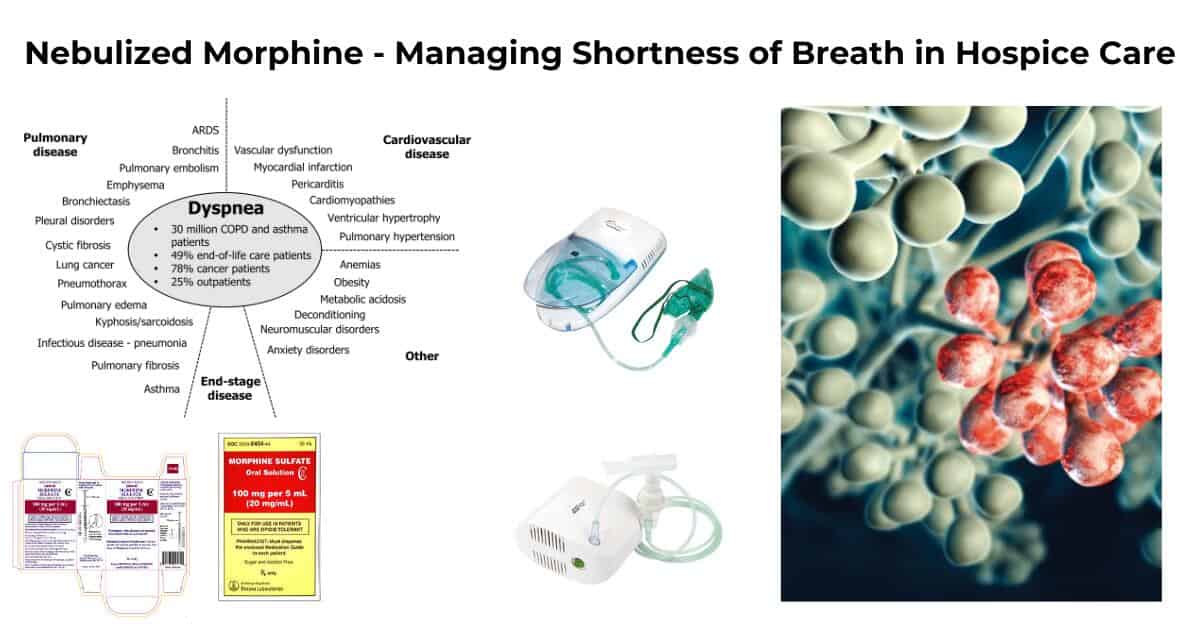
Table of Contents
Caring for terminally ill patients involves not only addressing their medical needs but also providing comfort and dignity during their final days. One of the most distressing symptoms these patients face is dyspnea or shortness of breath. This article is designed to help hospice and palliative care nurses, caregivers, and family members understand the nature of dyspnea in terminally ill patients and the importance of managing this symptom effectively. By employing an empathic approach, we aim to enhance the quality of life for patients and provide support to their families during this challenging time.
Dyspnea is a prevalent and distressing symptom experienced by many terminally ill patients. It significantly impacts their quality of life and can also cause anxiety and distress for caregivers and family members. Here are some key aspects to consider:
Managing dyspnea effectively is crucial in hospice care to ensure that patients remain as comfortable as possible. Here’s why it is essential:
By understanding and implementing these strategies, hospice and palliative care providers can offer compassionate and effective care to patients experiencing dyspnea, ensuring their comfort and dignity during the end-of-life journey.
Nebulized morphine is an innovative approach to managing dyspnea, particularly in hospice and palliative care settings. This method of administration offers several potential benefits over traditional systemic routes, making it an attractive option for patients experiencing severe breathlessness.
Nebulized morphine involves the administration of morphine in a mist form, which is inhaled directly into the lungs. This method allows the medication to act locally on the respiratory system, providing relief from dyspnea with potentially fewer systemic side effects.
Nebulized morphine differs from systemic morphine in several key ways:
| Aspect | Nebulized Morphine | Systemic Morphine |
|---|---|---|
| Route of Administration | Inhaled through a nebulizer | Oral, intravenous, or subcutaneous |
| Onset of Action | Rapid, often within 10-15 minutes | Variable, depending on the route |
| Side Effects | Potentially fewer systemic side effects | There is a higher risk of systemic side effects like sedation |
| Targeted Action | Direct action on lung receptors | Systemic distribution, affecting multiple body systems |
Understanding how nebulized morphine works can help caregivers and healthcare providers appreciate its potential benefits and limitations.
Morphine acts on opioid receptors located in the lungs, particularly in the large airways. These receptors are thought to play a role in reducing the sensation of breathlessness by:
While nebulized morphine primarily targets lung receptors, some systemic effects can still occur:
In conclusion, nebulized morphine offers a promising alternative for managing dyspnea in terminally ill patients. Its ability to provide rapid, targeted relief with potentially fewer systemic side effects makes it a valuable tool in hospice and palliative care. Understanding its mechanism and application can empower nurses and caregivers to make informed decisions about their patients’ care.
Various studies have explored the use of nebulized morphine for managing dyspnea in terminally ill patients, highlighting its potential effectiveness and safety. This section delves into the clinical evidence supporting its use, focusing on study findings and the safety and efficacy of nebulized morphine compared to other treatments.
Research has shown that nebulized morphine can significantly reduce breathlessness in patients with severe respiratory conditions, including those exposed to harmful substances or suffering from chronic pulmonary diseases.
Dosimetric nebulization systems are designed to deliver precise doses of medication directly to the lungs, optimizing the therapeutic effects while minimizing systemic exposure.
Nebulized morphine is generally well-tolerated, with a favorable safety profile compared to systemic administration.
When comparing nebulized morphine to other treatments for dyspnea, several factors are considered:
| Treatment | Effectiveness | Safety Profile |
|---|---|---|
| Nebulized Morphine | Effective in reducing breathlessness | Fewer systemic side effects, rapid relief |
| Systemic Opioids | Effective but with a higher risk of side effects | Greater risk of sedation and respiratory depression |
| Anxiolytics (e.g., Midazolam) | Effective in some cases, often used in combination | Risk of sedation, the potential for dependency |
In conclusion, nebulized morphine presents a promising option for managing dyspnea in hospice and palliative care settings. Its ability to provide targeted relief and a good safety profile makes it a valuable addition to the therapeutic arsenal for patients experiencing severe breathlessness. Understanding the clinical evidence and safety considerations can help healthcare providers make informed decisions to improve patient outcomes.
Nebulized morphine is increasingly recognized as a valuable tool in managing dyspnea in hospice care settings. This section provides detailed guidance on dosage, administration, and benefits for hospice patients, focusing on minimizing systemic side effects and effectively targeting end-stage pulmonary diseases.
Administering nebulized morphine requires careful attention to dosage and method to ensure safety and effectiveness.
Proper preparation of nebulized morphine is crucial for effective treatment.
Nebulized morphine offers several benefits for hospice patients, particularly those with end-stage pulmonary diseases.
Nebulized morphine is particularly beneficial for patients with advanced respiratory conditions, such as COPD and lung cancer, where traditional therapies may be insufficient.
One of the significant advantages of nebulized morphine is its ability to minimize systemic side effects commonly associated with opioid use.
| Advantage | Description |
|---|---|
| Localized Action | It targets lung receptors directly, providing effective relief from dyspnea. |
| Rapid Onset | Relief typically occurs within 10-15 minutes of administration. |
| Reduced Side Effects | Lower risk of systemic side effects due to minimal systemic absorption. |
| Patient Autonomy | Allows patients to manage their symptoms on an as-needed basis. |
In conclusion, nebulized morphine is a promising option for managing dyspnea in hospice care. It offers rapid and effective relief with a favorable safety profile. Understanding the practical aspects of its administration can empower hospice and palliative care nurses to provide compassionate and effective care for their patients.
Implementing nebulized morphine in hospice care requires careful consideration of patient selection and potential challenges. Understanding these factors can help hospice and palliative care nurses provide effective and compassionate care.
Selecting suitable patients for nebulized morphine treatment is crucial to ensure its effectiveness and safety.
When considering nebulized morphine for a patient, the following criteria should be evaluated:
Effective monitoring and assessment are essential to ensure patient safety and treatment efficacy:
| Criteria | Details |
|---|---|
| Diagnosis | Advanced pulmonary diseases with severe dyspnea |
| Medication Regimen | The current use of systemic opioids may enhance the effectiveness |
| Health Status | Consider kidney and liver function |
| Patient Preferences | Align treatment with patient and family goals |
Implementing nebulized morphine in hospice care settings can present several challenges, but with strategic planning, these can be overcome.
| Challenge | Strategy |
|---|---|
| Resource Availability | Ensure access to nebulizers and necessary supplies |
| Staff Training | Provide education on preparation and administration |
| Patient Concerns | Educate on the benefits and safety of nebulized morphine |
| Collaborative Care | Engage multidisciplinary teams for comprehensive care |
In conclusion, while there are challenges in implementing nebulized morphine in hospice care, careful patient selection, effective monitoring, and strategic planning can help overcome these barriers. By doing so, hospice and palliative care nurses can provide compassionate and effective care to patients experiencing severe dyspnea.
Nebulized morphine presents a promising option for managing dyspnea in hospice and palliative care settings. Its ability to provide rapid relief with minimal systemic side effects makes it an attractive alternative to traditional opioid administration methods. This conclusion summarizes the benefits of nebulized morphine and explores future directions and ongoing research needs.
Nebulized morphine offers several advantages for patients experiencing severe breathlessness, particularly in end-of-life care.
| Benefit | Description |
|---|---|
| Rapid Relief | Provides quick relief from dyspnea within minutes. |
| Minimized Side Effects | Localized action reduces systemic side effects. |
| Patient Autonomy | Enables self-administration for better symptom control. |
| Feasibility | Suitable for use in both clinical and home settings. |
While nebulized morphine shows promise, further research is needed to fully understand its potential and optimize its use in clinical practice.
By addressing these research needs, healthcare providers can better understand the role of nebulized morphine in managing dyspnea, ultimately improving patient outcomes and quality of life in hospice and palliative care settings.
Lung opioid receptors: Pharmacology and possible target for nebulized morphine in dyspnea
Opioids in Treatment of Refractory Dyspnea in Chronic Obstructive Pulmonary Disease: Yes, No, or Maybe
Unlabeled uses of nebulized medications
Nebulized Morphine: A Convenient and Safe Alternative to Dyspnea Relief?
Nebulized Versus Subcutaneous Morphine for Patients with Cancer Dyspnea: A Preliminary Study
Nebulized opioids for the palliation of dyspnea in terminally ill patients
Nebulized Morphine for Intractable Cough in Advanced Cancer: Two Case Reports
Nebulized drugs labeled and unlabelled use (SlideShare)
LHP E84 Nebulized Ketamine? (YouTube)
Managing breathlessness in palliative care
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.