Managing Infections in the Geriatric Population
Published on January 5, 2024
Updated on September 9, 2024
Published on January 5, 2024
Updated on September 9, 2024
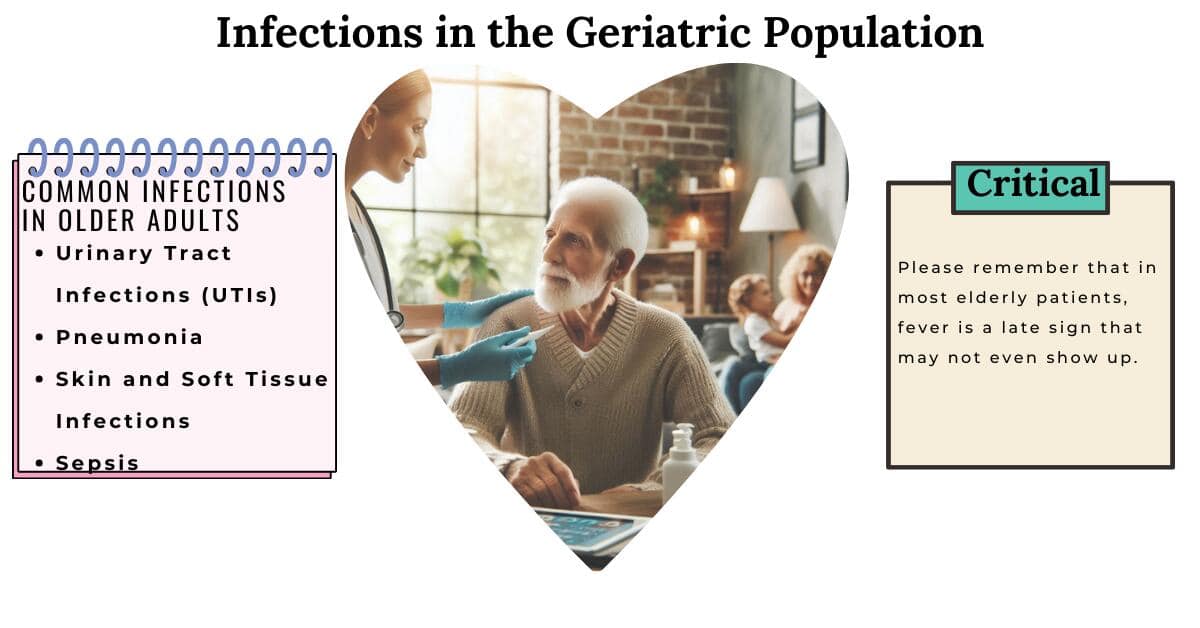
Table of Contents

Even with advancements in antibiotic treatments, infections remain a significant contributor to mortality among older adults. Managing infections in this population poses unique challenges, necessitating early detection and treatment due to the increased risk of morbidity and mortality. This article will delve into common infections in geriatric patients, encompassing early, middle, and late-stage symptoms, preventive measures, and prevalent treatment approaches, particularly for patients facing a terminal illness prognosis of six months or less.
Do you know what epidemiology means? It is the study of how often and why diseases occur in diverse groups of people. This section will discuss the epidemiology and risk factors of infections in older people.
Older people can get many infections, but some are more common. Here are some of the most common types and sources of infections in older adults:
Why do older people get more infections than younger people? And why are their infections more serious? Many factors make older people more vulnerable and less able to fight infections. Here are some of them:
What are pathogens? They are germs that can cause diseases. Some pathogens are more dangerous than others. They can be emerging or resistant. Emerging pathogens are new or rare germs that can cause outbreaks or epidemics. Resistant pathogens are germs that can survive or grow despite antibiotics. Both types of pathogens can pose a threat to the geriatric population. Here are some examples of them:
How do you know if you or someone else has an infection? Usually, you look for signs and symptoms. You can see or measure signs like fever, rash, or blood pressure. You can feel or describe symptoms, such as pain, nausea, or fatigue. Signs and symptoms can help doctors diagnose infections and determine the best treatment.
But what if the signs and symptoms are not clear or typical? This can happen in older people, who may have different or fewer signs and symptoms of infections than younger people. This can make it harder to diagnose and treat infections in older people. This section will discuss the typical and atypical signs and symptoms of infections in older people and how they can be diagnosed using laboratory tests, imaging studies, and microbiologic cultures.
Some of the typical signs and symptoms of infections in older adults are:
Some of the atypical signs and symptoms of infections in older adults are:
How can doctors confirm if an older person has an infection? Besides looking for signs and symptoms, they can also use laboratory tests, imaging studies, and microbiologic cultures. These methods can help identify the type and source of the infection and guide the treatment. However, these methods also have some limitations and challenges for older people. Here are some of them:
Why is it essential to diagnose and treat infections in older people as soon as possible? Infections can have severe and sometimes fatal consequences. They can worsen existing health problems, cause new complications, or lead to sepsis, a life-threatening condition that occurs when the body’s response to an infection damages its organs. Therefore, detecting and treating infections in older people early and promptly is crucial.
How can we do that? By being aware and alert of the signs and symptoms of infections in older people and seeking medical attention when they occur. Using laboratory tests, imaging studies, and microbiologic cultures appropriately and judiciously and interpreting the results carefully and accurately. By starting the antibiotic therapy as soon as possible and adjusting the dose and duration according to the type and severity of the infection. By monitoring the response and outcome of the treatment and changing the strategy if needed. By preventing infections first, following the hygiene recommendations, and avoiding the risk factors and sources of infection.
UTIs stand as the most prevalent bacterial infections among older adults. Symptoms may encompass fever, chills, confusion, agitation, and incontinence. Yet, pinpointing UTIs early in the elderly proves challenging, as typical signs like fever and leukocytosis are often absent. In older adults, a change in mental status, such as confusion or agitation, might be the sole indicator of a UTI.
Pneumonia is a common respiratory infection in the elderly. Symptoms may involve cough, fever, chills, shortness of breath, chest pain, and confusion. Nonetheless, older adults might lack fever or cough, with confusion or a decline in functional status as their primary symptom.
Skin and soft tissue infections, like cellulitis, are frequent in older adults. Symptoms may manifest as redness, warmth, swelling, and pain at the infection site. Cellulitis necessitates systemic antibiotic therapy, especially in patients displaying signs of systemic infection alongside bedsores.
Sepsis is a life-threatening condition caused by the body’s response to infection, which harms its tissues and organs. Symptoms in older adults may include lethargy, rapid breathing (tachypnea), appetite loss, dehydration, weakness, and confusion. Unique symptoms of infection in older patients encompass dehydration, weakness, and appetite loss.
Do you want to stay healthy and avoid getting sick? Of course you do! Nobody likes to have infections, illnesses caused by tiny germs that can make you ill. Infections can be quite common and severe in older people, who have a more challenging time fighting off germs than younger people. That is why it is essential to prevent infections in older people.
How can you do that? Following some simple tips can help you keep germs away from your body. Here are some of the best practices to prevent infections in older adults:
These are some of the best practices for preventing infections in older adults. Following these tips can reduce your chances of getting sick and improve your health and well-being. Remember, prevention is better than cure!
How can you get better if you have an infection? The best thing is to get the proper treatment. Treatment helps your body fight off the germs that make you sick, can help you feel better, and can prevent complications.
But not all infections are the same. Germs, such as bacteria, viruses, fungi, or parasites, can cause them. They can also affect different parts of your body, such as your lungs, bladder, skin, or blood. They can also be mild, moderate, or severe, depending on how sick you are and how much the infection affects your health.
That is why the treatment for infections depends on the type and severity of the infection. In this section, we will talk about the standard treatment approaches for infections in older people.
Bacterial infections are infections caused by bacteria, which are tiny living things that can multiply and cause diseases. Some examples of bacterial infections are urinary tract infections (UTIs), pneumonia, and skin infections.
Antibiotics are the most common treatment for bacterial infections. They are drugs that can kill or stop the growth of bacteria. There are many antibiotics, each one against a specific type of bacteria. For example, penicillin is an antibiotic that can treat strep throat caused by streptococcus bacteria.
However, antibiotics are not always practical or safe. Some bacteria can become resistant to antibiotics, which means that the antibiotics cannot kill them anymore. This can make the infection harder to treat and more dangerous. Some antibiotics can also cause side effects or interactions with other drugs, harming your health. Therefore, you should only take antibiotics when your doctor prescribes them and follow the instructions carefully. It would be best not to take antibiotics for viral infections, such as the flu or the common cold, because they will not work and may cause harm.
Viral infections are caused by viruses, tiny particles that can infect and damage cells. Some examples of viral infections are influenza (the flu), herpes, and shingles.
The most common treatment for viral infections is antiviral medications. Antiviral medications can interfere with viruses’ life cycles and prevent them from multiplying and spreading. There are many kinds of antiviral medicines, each working against a specific type of virus. For example, oseltamivir is an antiviral medication that can treat influenza caused by a virus called influenza.
However, antiviral medications are not always practical or safe. Some viruses can become resistant to antiviral drugs, meaning the medicines cannot stop them anymore. This can make the infection harder to treat and more dangerous. Some antiviral medications can also cause side effects or interactions with other drugs, which can harm your health. Therefore, you should only take antiviral medications when your doctor prescribes them and follow the instructions carefully.
Severe infections are profoundly serious and can threaten life. Some examples are sepsis, meningitis, and endocarditis.
The most common treatment for severe infections is hospitalization. Hospitalization is when you stay in the hospital for medical care and monitoring. You can get the best treatment for your infection in the hospital, such as intravenous (IV) antibiotics or antiviral medications, fluids, oxygen, or surgery. You can also get the best support for your health, such as pain relief, nutrition, or physiotherapy. You can also get the best protection from complications, such as organ failure, shock, or death.
However, hospitalization is not always easy or pleasant. It can be stressful, uncomfortable, or lonely. It can also expose you to other infections, such as hospital-acquired infections, which you get while in the hospital. Therefore, you should only go to the hospital when necessary and follow the advice of your doctor and the hospital staff. It would be best if you also tried to stay positive, calm, hopeful, and connected with your family and friends. It would help if you also tried to recover and return to your home and normal activities as soon as possible.
What if you have an infection and are very old and extremely sick? What if the doctors say that you have only a few months or weeks to live? What kind of treatment can you get?
When you have a terminal illness, it means that you have a disease that cannot be cured and will cause your death. When you have a terminal prognosis, it means that the doctors estimate how much time you have left to live. If you have a terminal prognosis of six months or less, you may want to change the focus of your treatment.
Instead of trying to cure your infection or prolong your life, you may want to focus on your comfort and quality of life. This is called palliative care. Palliative care is a type of care that helps you and your family cope with your illness and your symptoms. Palliative care can help you with things like:
Palliative care can also help you with other symptoms, such as fatigue, anxiety, depression, or insomnia. Palliative care can also help you with your emotional, spiritual, and social needs. Palliative care can help you express your feelings, find meaning and purpose, and connect with your loved ones.
One form of palliative care is hospice care. Hospice care is a type of care you can get in the final stages of your life. Hospice care can offer you comfort and support in your home, in a hospital, or in a particular facility. Hospice care can provide a team of professionals, such as doctors, nurses, social workers, chaplains, and volunteers, who can help you and your family with your physical, emotional, and spiritual needs. Hospice care can also provide you with equipment, supplies, and medicines that you may need.
When you have a terminal illness, you and your family can decide what kind of treatment you want for your infection. You can ask your doctor, your power of attorney (if you cannot make your own decisions), and your family to help you. You can get treatment for your infection, such as antibiotics or antiviral medications, or you can only get comfort care, such as pain relief or oxygen.
However, you should also be aware that if you are in the last week or two of your life, treatment for your infection may not help you much. It may not make you live longer or feel better. It may even make you feel worse or cause you more problems. Your body is too weak to fight or treat the infection. This is called futility. Futility means that the treatment is useless or harmful.
Therefore, you should think carefully about what kind of treatment you want for your infection when you have a terminal illness. You should weigh the benefits and risks of the treatment and consider your goals and values. It would be best to talk to your doctor, your power of attorney, and your family about your wishes and preferences. Writing your wishes and preferences in an advance directive document would be best. An advance directive is a way to tell your doctor and your family what kind of care you want or don’t want when you cannot speak for yourself. An advance directive can help you get the care that you want and avoid the care that you don’t want.
In conclusion, managing infections in the geriatric population is crucial due to the increased risk of morbidity and mortality. The unique challenges in diagnosing and treating infections in older adults, including the atypical presentation of symptoms and the limitations of diagnostic methods, necessitate a proactive approach to early detection and prompt initiation of treatment. Common infections such as urinary tract infections (UTIs), pneumonia, and skin and soft tissue infections pose significant risks to older adults, often presenting with atypical symptoms, making early identification challenging. Furthermore, the emergence of resistant pathogens, such as Methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-resistant enterococcus (VRE), underscores the importance of vigilance in infection prevention and control.
Emphasizing hand and oral hygiene is essential to preventing infections in older adults. Additionally, it is crucial to understand the treatment approaches for different types of infections, including the appropriate use of antibiotics for bacterial infections and the challenges associated with antiviral medications for viral infections.
In summary, a comprehensive approach to managing infections in the geriatric population involves early recognition of atypical symptoms, judicious use of diagnostic methods, proactive infection prevention strategies, and tailored treatment approaches to ensure the well-being of older adults. By prioritizing these measures, healthcare providers, caregivers, and family members can contribute to the overall comfort and quality of life for older adults facing infections.
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Common Infections in Older Adults
Common Infections in the Elderly: Causes, Facts, and Treatments
Urinary tract infections in long-term care: Improving outcomes through evidence-based practice
Infections in the Elderly Critically-Ill Patients
Predisposition to Infection in the Elderly
Challenges with Diagnosing and Managing Sepsis in Older Adults
Skin and Wound Infections: An Overview
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying