Living Better with Cancer: Why Palliative Care Should Start on Day One
Published on June 6, 2025
Updated on June 4, 2025
Published on June 6, 2025
Updated on June 4, 2025
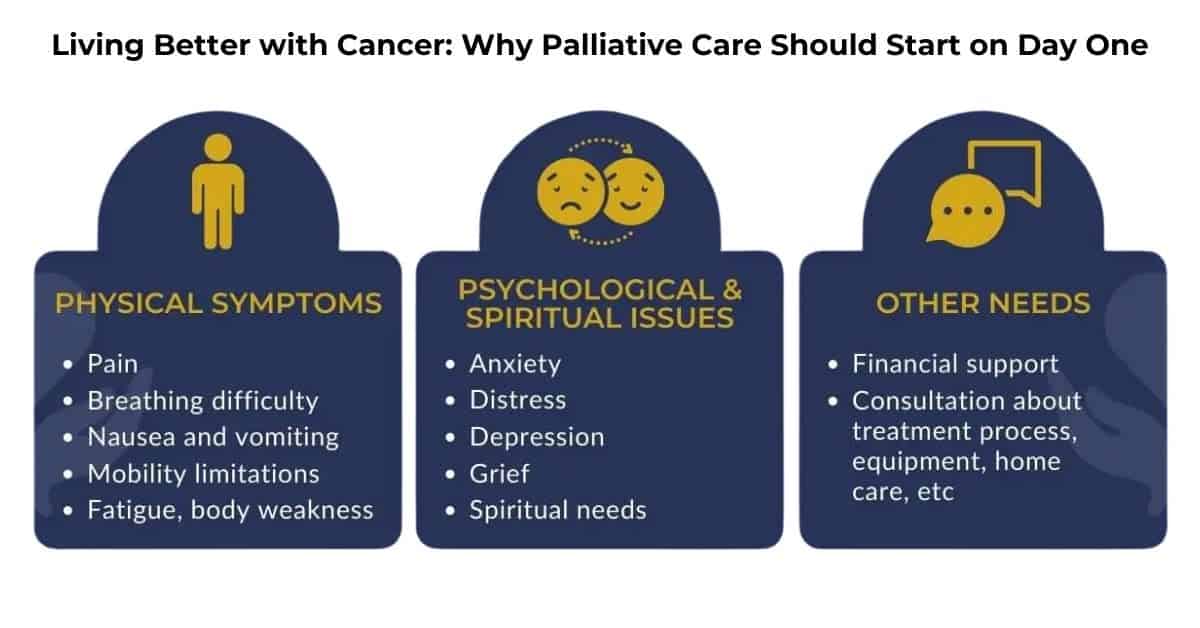
Table of Contents
Think of palliative care as an extra layer of support, like having a specialized team of experts who focus entirely on helping your loved one feel better while going through cancer treatment. This care is about treating the whole person, not just their cancer.
What Is Palliative Care?
Palliative care is specialized medical care that relieves symptoms of severe illness, pain, and stress. It works alongside your loved one’s cancer treatment to:
The palliative care team typically includes:
| Team Member | Role |
|---|---|
| Doctors | Manage symptoms and medications |
| Nurses | Provide direct patient care and family education |
| Social Workers | Help with emotional support and resources |
| Chaplains | Offer spiritual care if requested |
| Therapists | Assist with physical and occupational needs |
Common Myths and Misconceptions
Let’s clear up some common misunderstandings about palliative care:
The Difference Between Palliative Care and Hospice
This comparison helps clarify the distinct roles of each type of care:
| Aspect | Palliative Care | Hospice Care |
|---|---|---|
| Timing | Can start at a diagnosis | Begins in final months of life |
| Treatment | Supports ongoing treatment | Focuses on comfort care |
| Location | Any setting | Home or facility |
| Prognosis | Any stage of illness | Terminal diagnosis |
| Duration | No time limits | Generally last 6 months |
Remember, choosing palliative care early in cancer treatment can:
When your loved one receives a cancer diagnosis, ask their oncologist about including palliative care as part of their treatment plan. Many major cancer centers have palliative care teams in place to help from the very beginning. You don’t have to wait – the sooner palliative care begins, the more it can help both you and your loved one navigate this challenging journey together.
Starting palliative care as soon as your loved one is diagnosed with cancer can make a significant difference in their journey. Think of it like having an extra support system from the very beginning – one that helps manage challenges before they become overwhelming.
Why Timing Matters
Early integration of palliative care creates a strong foundation for your loved one’s cancer journey. Here’s why starting early is crucial:
Benefits from Day One
Starting palliative care alongside cancer treatment offers immediate advantages:
| Benefit Area | Impact on Patient | Impact on Family |
|---|---|---|
| Physical Comfort | Better pain and symptom control | Less distress seeing a loved one suffering |
| Emotional Support | Reduced anxiety and depression | Greater confidence in caregiving |
| Communication | A clearer understanding of treatment | Better prepared for care decisions |
| Practical Help | Easier navigation of the healthcare system | Access to resources and support |
| Quality of Life | More energy for daily activities | More quality time together |
Quality of Life Improvements
Early palliative care can enhance life in many ways:
Physical Improvements
Emotional Benefits
Social Advantages
Treatment Outcomes
For Caregivers and Family
Early palliative care also supports you as a caregiver by:
Making It Work
To get the most benefit from early palliative care:
Starting palliative care early doesn’t mean giving up hope or stopping treatment. Instead, it means giving your loved one the best possible support system to face cancer treatment with strength and dignity. The palliative care team becomes your partner in ensuring the highest quality of life throughout the cancer journey.
When your loved one feels better physically and emotionally, they’re more vigorous in their fight against cancer. Early palliative care helps make this possible by addressing problems before they become severe and creating a comprehensive support system from the start.
Don’t hesitate to ask the oncology team about integrating palliative care into your loved one’s treatment plan immediately. The sooner this extra layer of support begins, the more confidently and comfortably you and your loved one can navigate the challenges ahead.
When your loved one is fighting cancer, palliative care works alongside their cancer treatment to make the journey more manageable. Think of palliative care as your family’s support system, helping everyone cope better with the challenges ahead.
Pain and Symptom Management
The palliative care team excels at managing common cancer-related symptoms:
| Symptom | Management Approaches |
|---|---|
| Pain | Medications, massage, relaxation techniques |
| Nausea | Anti-nausea drugs, dietary changes, acupuncture |
| Fatigue | Energy conservation, exercise plans, sleep hygiene |
| Breathing Problems | Breathing exercises, medications, positioning |
| Loss of Appetite | Nutritional counseling, appetite stimulants |
Key benefits of expert symptom management:
Emotional and Mental Health Support
Cancer affects more than the body. The palliative care team helps manage the following:
Support services often include:
Family and Caregiver Resources
As a caregiver, you receive direct support through:
Educational Resources
Practical Support
Emotional Support
Coordinated Care Team Approach
The palliative care team coordinates with all healthcare providers to ensure comprehensive care:
| Team Member | Role in Coordination |
|---|---|
| Palliative Doctor | Oversees symptom management, communicates with oncology |
| Nurse Coordinator | Manages daily care, responds to concerns |
| Social Worker | Connects family with resources, provides counseling |
| Chaplain | Offers spiritual support when requested |
| Pharmacist | Review medications, prevent interactions |
| Therapists | Provides physical, occupational, and speech support |
Benefits of Coordinated Care:
Daily Support Activities
The palliative care team helps with the following:
Remember, palliative care is about helping your loved one live as well as possible while fighting cancer. The team works to:
Your palliative care team becomes partners in your loved one’s cancer journey, offering support, guidance, and expertise every step of the way. They’re available to answer questions, address concerns, and help navigate difficult decisions.
Don’t hesitate to lean on your palliative care team. They support you and your loved one through this challenging time. Regular communication with the team helps ensure the best possible care and support for everyone involved.
The earlier palliative care begins, the more effectively the team can support your family through the cancer journey. Ask about including palliative care in your loved one’s treatment plan today.
Getting started with palliative care might feel overwhelming, but taking it step by step makes the process manageable. Let’s break down how to make palliative care work best for your family’s needs.
Starting the Conversation
Begin by having an open discussion with your loved one’s healthcare team. Here are key questions to ask:
Tips for a productive conversation:
| Do | Don’t |
|---|---|
| Write down questions beforehand | Wait until crisis points |
| Bring a family member for support | Feel embarrassed to ask questions |
| Take notes during the meeting | Hesitate to ask for clarification |
| Express concerns openly | Keep symptoms to yourself |
| Ask about all available services | Assume anything is off-limits |
Building Your Support Team
Creating a strong palliative care team involves several steps:
Insurance and Financial Considerations
Understanding the financial aspects helps reduce stress:
Coverage Options
Common Covered Services
| Service Type | Typically Covered | May Need Approval |
|---|---|---|
| Doctor Visits | Yes | Sometimes |
| Nursing Care | Yes | Usually |
| Social Services | Often | Sometimes |
| Medical Equipment | Partially | Usually |
| Medications | Most | Some |
Financial Planning Steps
Tips for Managing Costs
Making the Most of Services
To maximize palliative care benefits:
Remember, palliative care is flexible and can be adjusted as needs change. Don’t hesitate to:
Open communication and active participation are essential to the success of palliative care. Your palliative care team wants to make this journey easier for you and your loved one. They’re there to support you every step of the way, so reach out whenever you need guidance or assistance.
Starting palliative care early allows you to build strong relationships with your care team and establish effective support systems before they’re urgently needed. Take the first step today by discussing palliative care options with your loved one’s oncology team.
Real experiences from patients, families, and healthcare providers show how palliative care can meaningfully improve the cancer journey. These stories highlight the positive impact of starting palliative care early.
Patient Perspectives’ Story – Stage 3 Breast Cancer
“When I started palliative care alongside my chemotherapy, everything changed. My pain became manageable, and I could still play with my grandchildren. The team helped me stay strong enough to complete my treatment. They didn’t just treat my symptoms – they helped me live my life.”Key benefits Sarah experienced:
Michael’s Story – Lung Cancer
“I was afraid palliative care meant giving up. Instead, it gave me strength. They helped manage my breathing problems and anxiety. I could focus on fighting cancer because I wasn’t struggling with symptoms every day.”
Family Experiences– The Martinez Family
“As caregivers for our mother, we felt lost until palliative care stepped in. They taught us how to:
Lisa’s Experience Caring for Her Husband
“Palliative care became our lifeline. They supported both of us through the following:
| Challenge | How Palliative Care Helped |
|---|---|
| Pain Crisis | 24/7 support and quick medication adjustments |
| Family Stress | Counseling and communication tools |
| Work Balance | Resources for home care and respite |
| Treatment Decisions | Clear information and guidance |
| Daily Living | Practical tips and equipment |
Healthcare Provider Insights – Dr. Rodriguez, Palliative Care Physician
“Starting palliative care early allows us to:
Nurse Jennifer’s Observations
“I’ve seen remarkable differences between patients who start palliative care early versus those who wait:
| Early Start | Late Start |
|---|---|
| Better symptom control | More crisis management |
| Stronger family coping | Increased stress |
| Fewer hospitalizations | More emergency visits |
| Clear care plans | Rushed decisions |
| Better outcomes | Harder recovery |
Social Worker Maria’s Perspective
“Families who embrace palliative care early often experience:
Success Factors
Common themes from successful palliative care experiences:
These stories show that palliative care can transform the cancer journey for both patients and families. The common thread is that earlier integration leads to better outcomes and more positive experiences.
Remember, every cancer journey is unique, but palliative care can be tailored to meet your specific needs. These stories illustrate how palliative care enables families to face cancer with greater strength, comfort, and hope.
Consider talking to your healthcare team today about including palliative care in your loved one’s cancer treatment plan. The support and expertise of a palliative care team can make a significant difference in your family’s cancer journey, just as it has for countless others.
Now is the time to take steps toward integrating palliative care into your loved one’s cancer treatment. Here’s your roadmap to getting started.
Questions to Ask Your Doctor
During your next oncology appointment, ask these essential questions:
About Starting Palliative Care
About Services
Finding Palliative Care Services
Start your search with these steps:
| Feature | Why It Matters |
|---|---|
| Board Certification | Ensures expertise |
| 24/7 Availability | Crisis support |
| Team Approach | Comprehensive care |
| Home Visits | Convenient access |
| Family Support | Complete care |
Creating Your Support Plan
Build your personalized care plan:
| Team Member | Contact Method | When to Contact |
|---|---|---|
| Palliative Doctor | Phone/Portal | Symptoms, Questions |
| Nurse | Direct Line | Daily Issues |
| Social Worker | Email/Phone | Resources, Support |
| After Hours | Emergency Line | Urgent Concerns |
Daily Management Tools
Create these essential tracking systems:
Next Steps Checklist
Take action today by:
Remember, starting palliative care is about enhancing your loved one’s quality of life during cancer treatment. Don’t wait for symptoms to become severe or for stress to overwhelm your family.
Take the first step today by calling your loved one’s oncology team and requesting a palliative care consultation. The sooner you begin, the more support and benefits your family will receive throughout the cancer journey.
Your actions now can significantly affect how well your loved one feels during treatment and how supported your family feels throughout this challenging time. Contact us today to begin building your palliative care support system.
Your journey with cancer doesn’t have to be walked alone. Palliative care provides a supportive hand that can make each step more manageable, from the very beginning.
Why Act Now
Starting palliative care early provides:
Take These Simple Steps Today
Remember
| What Palliative Care Offers | How It Helps You |
|---|---|
| Expert Symptom Management | Feel better during treatment |
| Emotional Support | Cope with challenges |
| Family Resources | Support your loved ones |
| Coordination of Care | Keep everything organized |
| Crisis Prevention | Peace of mind |
Your Next 24 Hours
Take these immediate steps:
Your Rights as a Patient
You have the right to:
Don’t let another day pass without taking action: your comfort, your family’s peace of mind, and your quality of life matter.
Pick up the phone now. Call your healthcare team and say: “I’d like to learn about adding palliative care to our treatment plan.” This one call can transform your cancer journey, providing the support and comfort you deserve.
Remember: Starting palliative care isn’t giving up – it’s giving yourself and your family every possible advantage in your cancer journey. Make the call today. Your future self will thank you.
Your Action Steps Right Now:
Your quality of life matters just as much as your treatment. Take action now to ensure you have the support you deserve throughout your cancer journey.
Greater Education Needed to Bring Palliative Care to Cancer Patients
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
Remember that there is currently no official accrediting body for end-of-life doula programs. Certification only means one graduated from a program. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.