Crafting a Comprehensive Hospice Admission Note: A Guide for Registered Nurses
Published on May 30, 2025
Updated on December 19, 2025
Published on May 30, 2025
Updated on December 19, 2025
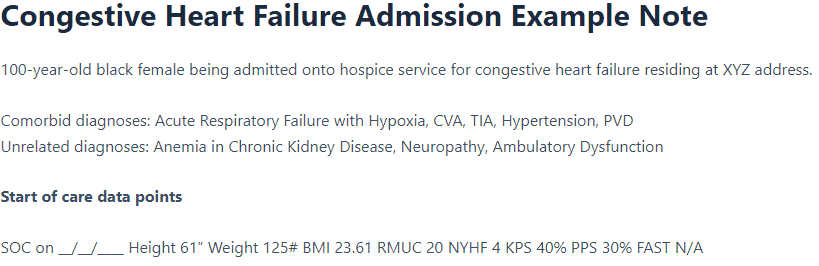
Table of Contents
Creating a comprehensive admission note is one of your most critical tasks as a hospice registered nurse. This document serves as the foundation for patient care and is crucial in demonstrating eligibility for hospice services. Explore why these notes are essential and how they impact patient care and documentation requirements.
Importance of a Comprehensive Admission Note
A thorough admission note is essential for several reasons:
Role in Patient Care and Eligibility Documentation
The admission note plays a dual role in both patient care and demonstrating eligibility for hospice services:
Patient Care:
Eligibility Documentation:
To ensure your admission notes effectively fulfill these roles, consider the following best practices:
Key Components of a Comprehensive Hospice Admission Note
| Section | Important Elements |
|---|---|
| Patient Information | • Demographics • Primary diagnosis • Comorbidities • Location of care |
| Clinical Assessment | • Vital signs • Pain assessment • Symptom evaluation • Functional status (e.g., PPS score) • Cognitive status |
| Psychosocial Evaluation | • Mental health status • Social support system • Spiritual/cultural considerations |
| Care Planning | • Goals of care • Medication review • Equipment needs • Advance directives |
| Eligibility Criteria | • Disease-specific decline indicators • Recent hospitalizations or ER visits • Weight loss or decreased oral intake • Increased dependence on ADLs |
Remember, your admission note is not just a formality – it’s a crucial tool that impacts patient care and supports your essential work. Creating comprehensive, accurate, and thoughtful admission notes sets the stage for high-quality hospice care, ensuring that patients receive the support they need during this sensitive time.
As a hospice-registered nurse, it is crucial to understand the Hospice Item Set (HIS) requirements for Medicare (see “below for the HOPE Tool that will replace HIS on October 1, 2025” down the page of this article). These requirements ensure that hospices provide quality care and report essential data to the Centers for Medicare & Medicaid Services (CMS). Let’s break down the critical aspects of HIS requirements and how they impact your role in patient care.
The Hospice Item Set is a standardized set of data elements used to calculate quality measures for hospice care. Here are the main points to remember:
Complying with HIS requirements is not just about following rules; it’s about ensuring quality care and maintaining the financial health of your hospice. Here’s why compliance matters:
The HIS encompasses several key measures that evaluate various aspects of hospice care. Let’s explore each one:
To ensure your hospice meets HIS requirements effectively, consider these practical tips:
| HIS Requirement | Deadline | Impact of Non-Compliance |
|---|---|---|
| HIS-Admission | 14 days from admission | Potential 2% reduction in annual payment update |
| HIS-Discharge | 7 days from discharge | Potential 2% reduction in annual payment update |
| Final Submission | 30 days from admission/discharge | Potential 2% reduction in annual payment update |
Remember, meeting HIS requirements is not just about compliance; it’s about providing the best possible care for your patients and their families. Integrating these practices into your daily work ensures that your hospice meets regulatory requirements while focusing on what matters most – compassionate, high-quality end-of-life care.
As a hospice-registered nurse, it is essential to be aware of the significant changes to hospice assessment and documentation requirements. Starting October 1, 2025, the Hospice Outcomes & Patient Evaluation (HOPE) tool will completely replace the Hospice Item Set (HIS) as the primary assessment and quality reporting mechanism for hospice care.
The HOPE tool represents a substantial advancement in hospice care quality measurement, offering a more nuanced and patient-centered approach compared to the HIS. This new assessment framework will transform how you document initial evaluations and ongoing care.
Key Differences Between HOPE and HIS:
Unlike HIS, which primarily collected data at admission and discharge, HOPE introduces multiple assessment timepoints better to track the patient’s journey through hospice care:
Table: HOPE Assessment Timepoints
| Assessment Type | When Required | Purpose |
|---|---|---|
| Admission | Start of hospice care | Establish a baseline, comprehensive needs assessment |
| HOPE Update Visits (HUVs) | Regular intervals during hospice stay | Monitor changing status and needs |
| Symptom Follow-Up Visits (SFVs) | Within 2 days of identifying moderate to severe symptoms | Address specific symptom impacts |
| Discharge | End of hospice care | Document final status and outcomes |
The HOPE admission assessment is critical as it establishes the baseline for future evaluations and care planning. Here’s what you need to include:
Key Components of HOPE Admission Assessment:
Pro Tip: Start familiarizing yourself with the HOPE assessment sections now, focusing on the symptom impact evaluation components (J2051 and J2053), which assess how symptoms affect your patient’s quality of life. The books HOPE in Action: A Practical Guide to Hospice Assessments and HOPE in Practice: Implementing Patient-Centered Outcomes in Hospice Care can be a wonderful asset in your toolkit.
Understanding the implementation timeline will help you prepare for a smooth transition:
Table: HOPE Implementation Timeline
| Date | Milestone |
|---|---|
| September 30, 2025 | Last day for HIS data collection |
| October 1, 2025 | HOPE implementation begins |
| FY 2026 | First-year HOPE data will be used for quality reporting |
| FY 2028 | First-year HOPE data will impact the Annual Payment Update |
Submission Requirements:
HOPE introduces new quality measures that focus on patient outcomes rather than processes. Two initial measures based on HOPE data include:
Both measures assess symptom reduction within two days of the initial assessment, highlighting the importance of prompt intervention and holistic care in hospice.
To ensure your hospice is ready for this significant change:
Remember: While the transition to HOPE requires adjustment, it ultimately provides better tools to deliver high-quality, patient-centered hospice care. By embracing HOPE’s comprehensive structure, you’ll be better equipped to understand and meet your patients’ needs throughout their hospice journey.
By preparing now for the HOPE implementation, you’ll ensure your hospice maintains compliance while enhancing the quality of care provided to your patients during one of life’s most challenging times.
It’s essential to be thorough and precise when documenting patient identification and basic information in a hospice admission note. This section helps establish a clear understanding of the patient’s background and current condition, which is crucial for providing personalized and effective care.
Age: Documenting the patient’s age is crucial, as it can significantly impact their care needs and the progression of their illness. Age-related factors can affect the choice of treatments and interventions.
Race: Recording the patient’s race is vital for understanding potential cultural, genetic, and social factors that might impact their care. Different races can have varying prevalence of certain diseases and may require culturally sensitive approaches to care.
Gender: Gender can play a significant role in the patient’s health status and the progression of their terminal illness. It’s important to note any gender-specific health issues or considerations.
Primary Diagnosis: The primary terminal diagnosis is the main condition that qualifies the patient for hospice care. This diagnosis should be clearly stated and supported by medical evidence. Common primary diagnoses include cancer, heart disease, chronic obstructive pulmonary disease (COPD), and neurological disorders like Alzheimer’s disease.
Example Table for Patient Identification and Basic Information:
| Field | Details |
|---|---|
| Age | 75 years |
| Race | Caucasian |
| Gender | Female |
| Primary Diagnosis | End-stage heart failure |
The location where hospice care will be provided is critical information. Hospice care can be delivered in various settings, each with its own considerations and resources.
Home Hospice Care:
Inpatient Hospice Facilities (GIP):
Nursing Homes or Long-Term Care Facilities:
Hospitals (GIP):
Example Table for Location of Hospice Service:
| Location Type | Description | Considerations |
|---|---|---|
| Home Hospice Care | Care is provided in the patient’s home. | Requires a primary caregiver, regular hospice team visits, and 24/7 availability. |
| Inpatient Hospice Facilities | Specialized facilities for intensive hospice care. | More medical support is suitable for intensive symptom management and GIP level of care. |
| Assisted Living Facilities | Hospice care can be provided in assisted living facilities | Medication technicians often provide care with assistance from resident care assistants and certified nursing assistants with the potential of LPN support. |
| Nursing Homes/Long-Term Care | Hospice care is provided in nursing homes or long-term care facilities. | Continuous care is ideal for patients without a primary caregiver at home. |
| Hospitals | Hospice care is provided in hospital settings, often with dedicated hospice units. | Access to hospital resources is suitable for complex medical needs and GIP level of care. |
By thoroughly documenting patient identification and basic information, including age, race, gender, primary diagnosis, and the location of hospice service, you ensure that the hospice team comprehensively understands the patient’s background and needs. This information is crucial for developing an effective and personalized care plan that respects patients’ preferences and provides the best possible quality of life during their remaining time.
When documenting diagnoses in a hospice admission note, providing a clear and comprehensive picture of the patient’s medical condition is essential. This includes the primary terminal diagnosis, comorbid diagnoses related to the terminal condition, and unrelated but significant diagnoses. Let’s explore each of these components in detail.
The primary terminal diagnosis is the main condition that qualifies the patient for hospice care. This diagnosis should be identified and supported by medical evidence. It is the condition that, if it runs its normal course, is expected to result in the patient’s death within six months.
Examples of Primary Terminal Diagnoses:
Key Points to Document:
Example Table for Primary Terminal Diagnosis:
| Field | Details |
|---|---|
| Primary Diagnosis | End-stage heart failure |
| Supporting Evidence | Echocardiogram showing severe dysfunction, NYHA Class IV symptoms |
| Prognosis | Life expectancy of six months or less |
Comorbid diagnoses are additional medical conditions related to the primary terminal diagnosis that contribute to the patient’s overall health status. These conditions can complicate the primary diagnosis and affect the patient’s prognosis and care needs.
Examples of Comorbid Diagnoses:
Key Points to Document:
Example Table for Comorbid Diagnoses:
| Comorbid Diagnosis | Relation to Primary Diagnosis | Impact on Care |
|---|---|---|
| Diabetes | Contributes to cardiovascular complications | Requires blood sugar monitoring and management |
| Chronic Kidney Disease | Exacerbates fluid retention and electrolyte imbalance | Requires careful management of medications and fluids |
Unrelated but significant diagnoses are medical conditions that are not directly related to the primary terminal diagnosis but are essential for the overall care plan. These conditions may require ongoing management and can impact the patient’s quality of life.
Examples of Unrelated but Significant Diagnoses:
Key Points to Document:
Example Table for Unrelated but Significant Diagnoses:
| Unrelated Diagnosis | Relevance to Care | Management Plan |
|---|---|---|
| Osteoarthritis | It affects mobility and pain levels | Pain management with medications and physical therapy |
| Depression | Impacts mental health and quality of life | Counseling and antidepressant medications |
You provide a comprehensive overview of the patient’s health status by thoroughly documenting the primary terminal diagnosis, comorbid diagnoses related to the terminal condition, and unrelated but significant diagnoses. This detailed documentation helps ensure that the hospice team can develop an effective and personalized care plan that addresses all aspects of the patient’s needs.
Anthropometric measurements are vital indicators of a patient’s health and nutritional well-being. They can help assess patient condition changes over time and guide care planning.
Important anthropometric measurements include:
Right Arm Mid-Upper Arm Circumference (MUAC)
MUAC is particularly useful in hospice care settings.
Here’s why:
MUAC Measurement Guidelines:
MUAC Interpretation Table:
| MUAC Measurement | Interpretation | Action |
|---|---|---|
| < 20 cm | Severe malnutrition | Urgent nutritional intervention is needed if the person is not in hospice |
| 20-24 cm | Moderate malnutrition | Nutritional support required |
| > 24 cm | Normal nutritional status | Continue monitoring |
Remember, a low MUAC (<20 cm) has been associated with higher in-hospital mortality rates, while a higher MUAC (>28 cm) may indicate better outcomes.
Performance scales help assess a patient’s functional status and guide care planning and prognosis estimation. Two commonly used scales in hospice care are the Karnofsky Performance Scale (KPS) and the Palliative Performance Scale (PPS).
Karnofsky Performance Scale (KPS)
The KPS ranges from 100 (normal, no complaints) to 0 (dead), with 10-point increments.
Simplified KPS Table:
| Score | Description |
|---|---|
| 100-80 | Able to carry on normal activities |
| 70-50 | Unable to work but able to live at home with varying amounts of assistance |
| 40-0 | Unable to care for self, requires institutional or hospital care |
Key points about KPS:
Palliative Performance Scale (PPS)
The PPS is designed explicitly for palliative care patients and correlates well with survival times.
Key features of PPS:
Simplified PPS Table:
| PPS Level | Ambulation | Activity & Evidence of Disease | Self-Care | Intake | Consciousness |
|---|---|---|---|---|---|
| 100%-80% | Full | Normal activity / Some disease | Full | Normal | Full |
| 70%-50% | Reduced | Unable to work / Significant disease | Varied | Reduced | Full or confusion |
| 40%-0% | Mainly in bed | Unable to do most activities / Extensive disease | Mainly assistance | Minimal to none | Full to drowsy or coma |
When documenting these key data points, remember to:
By carefully assessing and documenting these key data points, you’ll be better equipped to provide personalized, compassionate care to your hospice patients.
As a hospice registered nurse, documenting the care team and support network is crucial for ensuring comprehensive and coordinated patient care. This information facilitates communication, clarifies roles, and addresses all aspects of the patient’s care. Let’s explore the critical components of this documentation in detail.
Documenting the medical professionals involved in a patient’s care is essential for coordination and continuity. This includes both hospice team members and external healthcare providers.
Key information to document for each medical professional:
Example table for documenting medical professionals:
| Name | Title | Role | Contact Information | Availability |
|---|---|---|---|---|
| Dr. Jane Smith | Hospice Medical Director | Oversees care plan, prescribes medications, certifies hospice eligibility | gro.ecipsoh@htimsj 555-123-4567 | On-call 24/7 |
| John Doe | RN Case Manager | Coordinates care, conducts regular assessments | gro.ecipsoh@eodj 555-987-6543 | Mon-Fri, 9 am-5 pm |
| Sarah Johnson | Social Worker | Provides emotional support, assists with resources | gro.ecipsoh@nosnhojs 555-246-8135 | Tues & Thurs, 10 am-3 pm |
Remember to include:
Documenting family members and caregivers is crucial for understanding the patient’s support system and involving them in care decisions.
Key information to document for family members and caregivers:
Example table for documenting family members and caregivers:
| Name | Relationship | Role in Care | Contact Information | Availability |
|---|---|---|---|---|
| Mary Johnson | Daughter | Primary caregiver, medication management | moc.liame@nosnhojm 555-369-2580 | Lives with patient, available 24/7 |
| Tom Smith | Son | Assists with meals and transportation | moc.liame@htimst 555-147-2589 | Evenings and weekends |
| Lisa Brown | Neighbor | Provides respite care | moc.liame@nworbl 555-753-9514 | Tuesday and Thursday afternoons |
Important considerations:
Documenting legal representatives ensures that the patient’s wishes are respected and that the appropriate individuals are involved in the decision-making process.
Key information to document for legal representatives:
Example table for documenting legal representatives:
| Name | Relationship | Type of Authority | Contact Information | Scope of Authority |
|---|---|---|---|---|
| Robert Johnson | Son | Healthcare Power of Attorney | moc.liame@nosnhojr 555-951-7532 | All healthcare decisions |
| Susan Davis | Sister | Financial Power of Attorney | moc.liame@sivads 555-357-9514 | Financial decisions only |
| Michael Brown | Attorney | Legal Executor | moc.wal@nworbm 555-159-7532 | Estate matters |
Important considerations:
You create a comprehensive picture of the patient’s care ecosystem by thoroughly documenting the care team and support network. This information is invaluable for:
Update this information regularly as changes occur in the patient’s care team or support network. By maintaining accurate and up-to-date documentation, you contribute to providing the highest quality of compassionate care for your hospice patients.
As a hospice-registered nurse, I believe that providing a clear justification for hospice care is essential to ensuring patients receive the appropriate care and support. This involves documenting the recent decline in health and explaining why hospice care is the most suitable option for this individual. Let’s explore these components in detail.
Documenting the patient’s health decline over the past six to twelve months is crucial for demonstrating eligibility for hospice care. This information suggests that the patient’s condition is worsening and that they may benefit from hospice services.
Key Indicators of Health Decline:
Example Table for Documenting Recent Health Decline:
| Indicator | Details |
|---|---|
| Hospitalizations/ER Visits | Three hospital admissions in the last six months due to heart failure exacerbations |
| Weight Loss | The patient lost 15 pounds in the last three months, representing a 10% weight loss. |
| Functional Status | Now requires assistance with all ADLs, previously independent with some ADLs |
| Symptom Burden | Increased pain and shortness of breath, requiring higher doses of medication |
| Cognitive Decline | Increased confusion and memory loss, and inability to recognize family members |
The “Why Hospice, Why Now?” explanation is a narrative that provides context for the decision to pursue hospice care at this particular time. It should highlight the patient’s recent decline in health and explain how hospice care can address their current needs.
Key Points to Include:
Example: “Why Hospice, Why Now?”
Explanation:
Summary of Health Decline:
Over the past six months, Mr. Johnson has experienced significant health decline, including three hospital admissions for heart failure exacerbations, a 15-pound weight loss representing 10% in three months, increased dependence on others for all activities of daily living, worsening pain and shortness of breath, and increased confusion and memory loss.
Impact on Quality of Life:
These changes have significantly impacted Mr. Johnson’s quality of life. He is no longer able to enjoy his favorite activities, struggles with daily tasks, and experiences frequent discomfort and distress.
Goals of Care:
Mr. Johnson and his family aim to prioritize comfort and quality of life. They wish to avoid further hospitalizations and want to ensure that Mr. Johnson’s remaining time is as peaceful and pain-free as possible.
Benefits of Hospice Care:
Hospice care can provide the comprehensive support Mr. Johnson needs at this time. The hospice team will work to manage his symptoms, provide emotional and spiritual support, and offer respite care for his family. By choosing hospice care, Mr. Johnson can receive compassionate, patient-centered care that aligns with his and his family’s goals.
Example Table for “Why Hospice, Why Now?”
Explanation:
| Component | Details |
|---|---|
| Summary of Decline | Significant health decline over the past six months, including hospitalizations, weight loss, and cognitive decline |
| Impact on Quality | Decreased ability to enjoy activities, struggles with daily tasks, frequent discomfort, and distress. |
| Goals of Care | Focus on comfort and quality of life, and avoid further hospitalizations |
| Benefits of Hospice | Symptom management, emotional and spiritual support, and respite care for family |
By thoroughly documenting the recent health decline and clearly explaining “Why Hospice, Why Now?”, you help ensure that the patient receives the appropriate level of care and support. This documentation supports the patient’s eligibility for hospice care and helps communicate the patient’s needs and goals to the entire care team.
Conducting a thorough head-to-toe physical examination is crucial for providing comprehensive patient care as a hospice registered nurse. This assessment helps identify current issues, anticipate potential problems, and inform the development of a care plan. Let’s explore each component in detail.
A thorough skin assessment is vital for identifying potential pressure injuries, infections, or other skin-related issues.
Key points to assess:
Braden Scale for Predicting Pressure Sore Risk:
| Risk Factor | 1 Point | 2 Points | 3 Points | 4 Points |
|---|---|---|---|---|
| Sensory Perception | Completely Limited | Very Limited | Slightly Limited | No Impairment |
| Moisture | Constantly Moist | Very Moist | Occasionally Moist | Rarely Moist |
| Activity | Bedfast | Chairfast | Walks Occasionally | Walks Frequently |
| Mobility | Completely Immobile | Very Limited | Slightly Limited | No Limitation |
| Nutrition | Very Poor | Probably Inadequate | Adequate | Excellent |
| Friction & Shear | Problem | Potential Problem | No Apparent Problem | – |
Note: Lower scores indicate higher risk for pressure injuries
Observe the patient’s overall appearance and condition, which can provide valuable insights into their health status.
Assess the following:
A neurological assessment helps evaluate cognitive function and identify any neurological deficits.
Key components:
Glasgow Coma Scale:
| Response | Score |
|---|---|
| Eye Opening | |
| Spontaneous | 4 |
| To verbal stimuli | 3 |
| To pain | 2 |
| None | 1 |
| Verbal Response | |
| Oriented | 5 |
| Confused | 4 |
| Inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| None | 1 |
| Motor Response | |
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion | 3 |
| Abnormal extension | 2 |
| None | 1 |
Evaluating the patient’s psychological state is crucial for providing holistic care.
Assess the following:
A thorough cardiopulmonary assessment helps identify respiratory and circulatory issues.
Key components:
New York Heart Association (NYHA) Functional Classification:
| Class | Symptoms |
|---|---|
| I | There is no limitation on physical activity |
| II | Slight limitation of physical activity |
| III | Marked limitation of physical activity |
| IV | Unable to carry out any physical activity without discomfort |
Assessing the gastrointestinal system helps identify issues with nutrition and elimination.
Key points to assess:
Evaluating the genitourinary system helps identify issues with urination and potential infections.
Assess the following:
Evaluating the patient’s ability to perform activities of daily living (ADLs) helps determine their level of independence and care needs.
Assess the following ADLs:
Katz Index of Independence in Activities of Daily Living:
| Activity | Independent (1 point) | Dependent (0 points) |
|---|---|---|
| Bathing | Bathes self wholly or needs help in bathing only a single part of the body. | Needs help with bathing more than one part of the body, getting in or out of tub or shower |
| Dressing | Gets clothes from closets and drawers and puts on clothes and outer garments complete with fasteners | Needs help with dressing self or needs to be completely dressed |
| Toileting | Goes to the toilet, gets on and off, arranges clothes, cleans genital area without help | Needs help transferring to the toilet, cleaning self, or using a bedpan or commode |
| Transferring | Moves in and out of bed or chair unassisted | Needs help in moving from bed to chair or requires a complete transfer |
| Continence | Exercises complete self-control over urination and defecation | Is partially or totally incontinent of bowel or bladder |
| Feeding | Gets food from a plate into the mouth without help | Needs partial or total help with feeding or requires parenteral feeding |
Assessing and managing symptoms is a crucial aspect of hospice care.
Pain Assessment:
Shortness of Breath Assessment:
Nausea and Vomiting:
Other Areas of Discomfort:
Conducting a thorough head-to-toe physical examination can help you gain a comprehensive understanding of your patient’s condition and needs. This information is crucial for developing an effective care plan and providing compassionate, patient-centered hospice care.
Documenting a patient’s recent medical history provides valuable insights into their overall health status and helps identify potential areas of concern. Here are the key elements to include:
Falls are a significant concern for hospice patients, as they can lead to severe injuries and complications. Thorough documentation of fall history is essential for preventing future incidents and ensuring patient safety.
Key components to document in the fall history:
Fall Risk Assessment Table:
| Risk Factor | Low Risk | Moderate Risk | High Risk |
|---|---|---|---|
| Age | < 65 years | 65-80 years | > 80 years |
| Fall History | No falls in the past year | 1-2 falls in the past year | 3+ falls in the past year |
| Mobility | Independent | Uses an assistive device | Bed-bound or chair-bound |
| Medications | < 4 medications | 4-6 medications | > 6 medications |
| Cognitive Status | Alert and oriented | Mild confusion | Severe confusion or dementia |
Documenting emergency room visits and hospitalizations is crucial for understanding the patient’s recent health challenges and coordinating care with other healthcare providers.
For each emergency room visit or hospitalization, record the following:
Impact of ER Visits and Hospitalizations on Hospice Care:
Tips for Effective Documentation:
By carefully documenting recent medical history, fall history, and emergency room visits and hospitalizations, you provide valuable information that helps ensure the best possible care for your hospice patients. This comprehensive documentation enables the entire care team to understand the patient’s recent health challenges and collaborate to address their evolving needs with compassion and expertise.
As a hospice-registered nurse, documenting eligibility for hospice care is crucial for ensuring that patients receive the appropriate care and support. This involves understanding and applying Local Coverage Determination (LCD) criteria. Let’s examine the key components of eligibility documentation, with a focus on LCD matching areas.
Local Coverage Determinations (LCDs) provide guidelines for determining whether a patient meets the clinical criteria for hospice care. These guidelines are crucial for documenting medical necessity and ensuring compliance with Medicare requirements.
Key Components of LCD Matching Areas:
1. Terminal Illness Prognosis
The primary criterion for hospice eligibility is a physician’s certification that the patient has a terminal illness with a life expectancy of six months or less if the disease runs its normal course.
Key Points to Document:
2. Disease-Specific Guidelines
LCDs provide specific criteria for various terminal illnesses. These guidelines help determine if a patient’s condition meets the requirements for hospice care.
Examples of Disease-Specific Guidelines:
Cancer:
Heart Disease:
Dementia:
Example Table for Disease-Specific Guidelines:
| Disease | Key Criteria | Supporting Documentation |
|---|---|---|
| Cancer | Widespread, aggressive disease | PPS < 70%, refusal of therapy |
| Heart Disease | NYHA Class IV symptoms | Optimally treated with medications |
| Dementia | FAST Stage 7C or beyond | Significant conditions in the past 12 months |
3. Non-Disease Specific Decline
Patients may also qualify for hospice care based on a general decline in clinical status, even if they do not meet specific disease criteria.
Key Indicators of Non-Disease Specific Decline:
Example Table for Non-Disease Specific Decline:
| Indicator | Description | Documentation |
|---|---|---|
| Weight Loss | Unintentional weight loss of > 10% in the past six months | Weight records, nutritional assessments |
| Functional Status | Increased dependence in ADLs | ADL assessments, caregiver reports |
| Hospitalizations | Multiple admissions in the past six months | Hospital records, discharge summaries |
| Symptom Burden | Worsening pain, dyspnea | Symptom assessments, medication records |
4. Supporting Documentation
Supporting documentation, including clinical notes, test results, and other relevant information, is essential for demonstrating that the patient meets the LCD criteria for hospice eligibility.
Key Points to Include:
Example Table for Supporting Documentation:
| Document Type | Description | Example |
|---|---|---|
| Clinical Notes | Detailed progress notes from healthcare providers | Physician notes, nursing assessments |
| Test Results | Relevant lab results and diagnostic tests | Blood tests, imaging studies |
| Symptom Assessments | Pain scales, dyspnea scales | Numeric Rating Scale, Modified Borg Scale |
| Functional Assessments | ADL assessments, PPS scores, FAST scores | Katz Index, PPS chart, FAST chart |
By thoroughly documenting eligibility using LCD matching areas, you help ensure that your hospice patients receive the appropriate level of care and support. This comprehensive documentation supports the patient’s eligibility for hospice care and helps communicate the patient’s needs and goals to the entire care team.
As hospice registered nurses, developing a comprehensive care plan is crucial for providing high-quality, patient-centered care. Let’s explore the key components of care planning in detail.
Determining and documenting a patient’s code status is essential for respecting their end-of-life wishes.
Key points to consider:
Common Code Status Options:
Example Table for Code Status Documentation:
| Code Status | Description | Interventions Allowed |
|---|---|---|
| Full Code | All life-saving measures | CPR, intubation, medications |
| DNR | No resuscitation | Comfort measures, medications |
| DNI | No intubation | CPR, medications, no intubation |
| Comfort Measures Only | Focus on comfort | Pain management, symptom control |
Identifying and documenting the primary caregiver is crucial for coordinating care and providing support.
Key information to document:
Caregiver Assessment Checklist:
Assessing and documenting equipment needs ensures patients have the necessary tools for comfort and safety.
Common hospice equipment:
Example Table for Equipment Documentation:
| Equipment | Purpose | Date Ordered | Date Received | Special Instructions |
|---|---|---|---|---|
| Hospital bed | Comfort and positioning | MM/DD/YYYY | MM/DD/YYYY | Electric, with side rails |
| Oxygen concentrator | Oxygen therapy | MM/DD/YYYY | MM/DD/YYYY | 2 liters/minute continuous |
| Wheelchair | Mobility | MM/DD/YYYY | MM/DD/YYYY | 18-inch seat width |
Accurate documentation of medication orders is crucial for managing symptoms and ensuring patient comfort.
Key components of medication orders:
Example Table for Medication Orders:
| Medication | Dosage | Route | Frequency | Purpose | Special Instructions |
|---|---|---|---|---|---|
| Morphine Sulfate | 5 mg | Buccal | Every 2 hours as needed | Pain management | Monitor for respiratory depression |
| Lorazepam | 0.5mg | Sublingual | Every 4 hours as needed | Anxiety relief | May cause drowsiness |
| Ondansetron | 4 mg | Oral | Every 6 hours as needed | Nausea control | Take with food if possible |
Developing and documenting follow-up plans ensures continuity of care and addresses evolving patient needs.
Key components of follow-up plans:
Example Follow-up Plan:
By thoroughly addressing these critical care planning components, you can ensure that your hospice patients receive comprehensive, compassionate care tailored to their needs. Remember to regularly review and update the care plan as the patient’s condition changes, always keeping their comfort and quality of life at the forefront of your care.
Creating clear, detailed documentation guidelines is essential for consistency across your hospice team.
Key components to include:
Pro tip: Create a quick reference guide or checklist that nurses can easily access during patient visits.
Staying up-to-date with regulatory requirements is crucial for proper documentation and avoiding penalties.
Steps to maintain compliance:
Comprehensive training ensures all team members understand documentation expectations and best practices.
Effective training strategies:
Continuous support helps reinforce good documentation habits and address challenges as they arise.
Ways to offer ongoing support:
Regular assessment of documentation quality helps identify areas for improvement and ensures consistency.
Monitoring and evaluation techniques:
Recognizing and rewarding good documentation practices motivates team members and reinforces the importance of quality documentation.
Ideas for celebrating success:
Encouraging open dialogue about documentation challenges and best practices fosters a culture of continuous improvement.
Strategies for promoting open communication:
Utilizing technology can streamline documentation processes, improving accuracy and consistency.
Technology solutions to consider:
| Solution | Benefits |
|---|---|
| Electronic Health Records (EHR) | Standardized forms, built-in prompts, easy access to patient history |
| Mobile devices | Real-time documentation at the point of care |
| Voice-to-text software | Faster note-taking reduced typing strain |
| Digital signature tools | Streamlined approval processes |
Protecting patient information is a legal requirement and essential for maintaining trust.
Best practices for safeguarding privacy:
Clear, concise documentation ensures that all team members can easily understand and act on the information provided.
Tips for clear documentation:
Timely documentation ensures accuracy and helps prevent essential details from being forgotten.
Strategies for timely documentation:
By implementing these best practices, your hospice team can achieve consistent, high-quality documentation that supports excellent patient care and meets regulatory requirements. Remember, good documentation is a skill that improves with practice and ongoing support.
100-year-old black female being admitted to hospice service for congestive heart failure, residing at XYZ address.
Comorbid diagnoses: Acute Respiratory Failure with Hypoxia, CVA, TIA, Hypertension, PVD
Unrelated diagnoses: Anemia in Chronic Kidney Disease, Neuropathy, Ambulatory Dysfunction
Start of care data points
SOC on __/__/____ Height 61” Weight 125# BMI 23.61 RMUC 20 NYHF 4 KPS 40% PPS 30% FAST N/A
Coordination
Coordination took place with hospice medical director Dr John Jones, who gave the verbal certificate of terminal illness (CTI), attending physician Dr. Jane Doe for her CTI under the same primary terminal diagnosis, primary caregivers Penny and Bonnie with all parties in agreement with the initial plan of care.
Why Hospice? Why Now?
The patient was admitted to _____ Hospital from 5/20 to 5/31 for Acute on Chronic CHF with acute respiratory failure with hypoxia and tachypnea. Before this current hospital discharge, the hospital providers were recommending hospice due to disease progression as this was the third hospital admission this year, with the patient progressively getting worse, as evidenced by the previous admission of the patient at New York Heart Class III, yet being able to ambulate with a rolling walker. Now, the patient is at New York Heart Class IV, is bedbound, unable to tolerate being in a chair, and is now in complete care.
In the two weeks before May 20th, the patient went from ambulating with her rolling walker to activities to staying in her room, complaining of weakness and being too short of breath on room air to go to activities, including meals. On May 1st, the patient weighed 134#.
On hospital discharge, the patient and power of attorney decided on hospice service for comfort care only. The patient is DNR and DNI and is not to be hospitalized.
Physical Assessment
100-year-old female with a sallow complexion, frail, visible bony prominences, and paper-thin, fragile skin. Extensive ecchymosis is in the right lower extremity, and mild ecchymosis is in the left lower extremity. Reports moderate “burning” pain in the left foot that did resolve in approximately ten minutes. A bilateral foot exam showed intact skin. The patient has a history of neuropathy. Disoriented x2 with forgetfulness. Murmur auscultated. Hypertensive 160/60 manual right arm blood pressure lying at rest. Diminished lung sounds bilaterally, with poor air exchange and weak inspiratory and expiratory effort, accompanied by pleural friction rub in the bases. Oxygen saturation is 87% on room air, and there is no shortness of breath at complete rest. Placed on 2L of continuous oxygen, saturation reached 94%, with the heart rate decreasing but remaining within normal limits. Frequent non-productive cough. 16 fr Foley draining clear yellow urine. Incontinent of bowel. Unable to ambulate, being bedbound, requiring complete care.
Medical Management and Primary Care
The patient’s daughter, Penny, will manage the medications, and Penny’s sister, Bonnie, who lives nearby, will assist. Comfort medications were present at the time of admission. They reviewed the procedure with Penny and Bonnie, including a return demonstration of how to use a 1 mL syringe to draw up 0.25 mL of morphine concentrate and administer it buccally to the patient.
All current medications were refused, and recommendations were made to discontinue vitamins and supplements as well as atorvastatin, to which the daughters agreed. At this time, no refills or new prescriptions are needed.
Equipment
The hospital bed, low-loss air mattress overlay, overbed table, 5 liters per minute oxygen concentrator with humidification, nasal cannula, and extension tubing were delivered and set up before admission. At this time, no further equipment is needed.
Follow Up
The post-admission visit will occur tomorrow; please print medium-tab briefs, a wash basin, lotion, soap, and barrier cream.
As we conclude our discussion on comprehensive hospice admission documentation, let’s reflect on the key points and their importance in delivering quality end-of-life care.
Thorough documentation is the backbone of quality hospice care. Here’s why it’s so crucial:
Your documentation directly affects patient care and hospice eligibility in several ways:
| Impact Area | Description |
|---|---|
| Patient-Centered Care | Detailed notes help tailor care to each patient’s specific needs and preferences. |
| Symptom Management | Accurate tracking of symptoms and interventions leads to more effective pain and symptom control. |
| Family Support | Documentation of family interactions and education helps ensure comprehensive support for caregivers. |
| Eligibility Maintenance | Clear evidence of ongoing terminal decline supports continued hospice eligibility. |
| Quality Metrics | Thorough documentation contributes to better performance on quality measures. |
Remember: Every note you write tells a part of your patient’s story. By documenting thoroughly and compassionately, you’re not just fulfilling a requirement – you’re ensuring that each patient receives the best possible care during their final journey. As hospice nurses, your role in documentation is invaluable. Your notes provide the foundation for the following:
By prioritizing thorough, accurate, and empathetic documentation, you’re significantly impacting the lives of your patients and their families during one of life’s most challenging times.
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Diagnosis Codes That Cannot Be Used As Primary Diagnosis Codes on the Hospice Claim (PDF)
CMS Hospice Determining Terminal Status
CMS Billing and Coding: Hospice: Determining Terminal Status
Home Care and Hospice Conference Expo: Diagnosis Coding in Hospice (PDF)
Compliance-based, Eligibility Driven Hospice Documentation: Tips for Hospice Nurses
HOPE in Action: A Practical Guide to Hospice Assessments
HOPE in Practice: Implementing Patient-Centered Outcomes in Hospice Care
Mastering Dementia Admissions: Essential Guidelines for Hospice Eligibility
Mastering Hospice Eligibility: An Essential Guide for RNs and Clinical Managers
Hospice Eligibility Documentation Tips and Strategies (PDF)
Hospice Documentation Guidelines and Resources
Compelling Hospice Nursing Narratives: Ensuring Continued Eligibility And Comprehensive Care
Avoiding Problematic Language In Hospice Nursing Narratives
Hospice Documentation Checklist (PDF – one type) and Hospice Documentation Checklist (PDF – another type)
Hospice Documentation Cheat Sheet (PNG image)
Certification and Recertification Requirements
GHPCO Annual Conference: Painting a Picture of Eligibility Through Documentation (PDF)
Hospice – Documenting Slow Decline (PDF)
Documentation to Support Patient Decline (PDF)
Documentation+to+Support+Hospice+Medicare+Recertification.pdf (PDF)
Bates Jenson Wound Assessment Tool (PDF)
FRAIL Palliative Wound Care: Palliative Wound Care And Healing Probability Assessment Tool (PDF)
Confusion Assessment Method (CAM)
Cumulative Illness Rating Scale (CIRS)
Edmonton Symptom Assessment Scale (ESAS) and ESAS Form (PDF)
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp)
Hospitalization Risk Profile (HRP)
Mini-Mental State Examination (MMSE)
Timed Up & Go (TUG) Assessment Test
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.