Category: Symptom Management
Articles relating to managing symptoms of terminally ill patients with the goal of maintaining comfort through the natural dying process.
Articles relating to managing symptoms of terminally ill patients with the goal of maintaining comfort through the natural dying process.
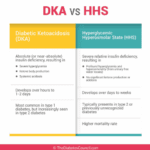
As an experienced hospice nurse, I understand that managing diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) at end of life can be challenging, especially when patients choose to stop taking their diabetic medications or when those medications are no longer an option. In this article, I will provide information on recognizing the signs and symptoms of hyperglycemic crises and outline comfort-based treatment options that align with hospice goals of care.

I know that the journey you and your loved one are on can be challenging, especially when facing a terminal illness. As an experienced hospice nurse caring for terminally ill patients, I want to provide you with some valuable insights on a common issue that may arise during this time: contractures.

Discover effective non-pharmacological methods to manage shortness of breath in hospice care. Learn about positioning techniques, breathing exercises, and environmental adjustments that can comfort and relieve patients experiencing dyspnea, enhancing their quality of life during end-of-life care.
Learn effective strategies for managing hallucinations in terminally ill patients. This guide covers pharmacological and non-pharmacological methods to improve comfort and quality of life.

Doll therapy offers a compassionate approach to enhancing the quality of life for dementia patients. By providing comfort, reducing anxiety, and promoting social interaction, this non-pharmacological intervention can significantly improve emotional well-being and cognitive function in individuals with dementia.
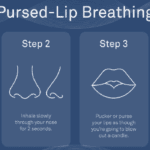
Dealing with shortness of breath can be challenging for terminally ill patients, but there are techniques that can help manage this symptom and improve their overall comfort. One such technique is pursed lip breathing. Pursed lip breathing is a simple and effective breathing technique that can help reduce shortness of breath and improve oxygen exchange in the lungs. As an experienced hospice nurse with years of experience, I will guide you through the steps of pursed lip breathing in a compassionate and easy-to-understand manner.

Caring for a loved one with dementia can be both rewarding and challenging. If your loved one has been restless throughout their life, this restlessness may continue as a symptom of their dementia. As an experienced hospice nurse, I understand the difficulties you may face in managing habitual restlessness while ensuring the safety and welfare of your loved one. In this article, I'll provide you with practical tips and evidence-based practices to create a calming environment for your loved one, even if they have trouble with fine motor control due to arthritis or other factors.

This article will delve into common infections in geriatric patients, encompassing early, middle, and late-stage symptoms, preventive measures, and prevalent treatment approaches, particularly for patients facing a terminal illness prognosis of six months or less.
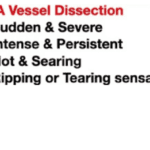
The purpose of this article is to provide you with some information and guidance about AAAs and how they can be managed in hospice patients.
The PAINAD scale is a comprehensive tool that assesses and manages pain in older adults with dementia and delirium. It focuses on observable signs of pain rather than patient self-report, making it particularly useful for individuals who cannot communicate their discomfort

It is common for family members and caregivers who are not trained in end-of-life topics to be concerned about their loved one's oxygen concentration (SpO2 and sometimes also abbreviated SPaO2) reading from a pulse oximeter. Suppose their loved one refuses external oxygen or takes off the external oxygen. In that case, this often causes distress to the family and caregivers because they are focused on the numbers vs. the patients themselves. Hospice is about patient-centered care, and I would like to present four case studies to demonstrate how hospice manages this situation with compassion.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.
If you have a loved one diagnosed with Parkinson's disease, you may have many questions and concerns about what to expect and how to provide the best care possible. As an experienced hospice nurse with extensive experience in managing terminal illnesses, I am here to guide you through the journey of Parkinson's disease and offer compassionate support. In this article, we will explore Parkinson's disease, the changes your loved one may experience over time, and practical tips to care for them from the onset to the end-of-life phase.

Radiation therapy is a common treatment for head and neck cancers, but it can lead to the loss of taste, also known as dysgeusia, in some patients. This can be a distressing side effect, but there are steps that patients and caregivers can take to help restore the patient's sense of taste as quickly as possible, with minimal risk. While there is no guaranteed way to restore taste, these tips and strategies may help patients regain some of their enjoyment of food and drink.
Dementia is a progressive disease that affects memory, thinking, and behavior. While there is no cure for dementia, there are ways to minimize its progression and improve the quality of life for those living with the disease. Here are some activities to do, activities to avoid, dietary changes to make, and activities to perform to minimize the progression of dementia.
When a loved one is terminally ill, it can be a perplexing and emotional journey. Understanding the root cause of their declining health becomes paramount. It's a complex puzzle where family members often grapple with questions: Are the symptoms a result of medications prescribed, or are they intrinsic to the terminal disease? This article delves into the critical distinctions between medication side effects and the natural progression of terminal illnesses, offering insights to empower families and caregivers in making informed decisions about their loved one's care.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
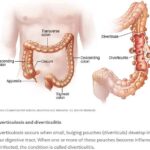
Caring for a loved one with a history of diverticulitis requires a combination of preventive measures, early detection of warning signs, and understanding the common signs and symptoms of this condition. Your role as a caregiver is crucial in providing support and assistance to ensure their well-being. In this comprehensive guide, we will explore essential aspects of caring for someone with diverticulitis, including prevention, early warning signs, and treatment options.

In the realm of hospice care, where empathy and compassion are paramount, a remarkable approach called Validation Therapy has emerged as a beacon of hope and comfort for individuals facing dementia and cognitive disorders in their final journey. As an experienced hospice registered nurse case manager, I've witnessed the transformative impact of Validation Therapy on patients, allowing them to find solace, regain their self-worth, and experience a sense of dignity during their end-of-life phase.

Caring for a terminally ill loved one is a profound and challenging journey that requires compassion, understanding, and a willingness to alleviate any discomfort they may experience. In this guide, we will explore the concept of discomfort, its distinction from pain, and the importance of recognizing and addressing discomfort in addition to pain. You'll be better equipped to provide holistic care that enhances your loved one's quality of life during this sensitive time.
Throughout your loved one's illness, you might find yourself thinking that they don't require "pain medication" because they don't seem to be in pain. They might even respond with a direct "no" when asked about their pain. However, are you aware that most types of pain medication can alleviate discomfort? Did you also know that your loved one could be feeling uncomfortable without necessarily being in severe pain? Nonetheless, it's important to recognize that their discomfort requires the same treatment as if they were in pain.

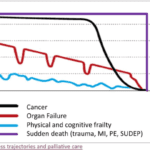
One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.
I have seen firsthand the benefits and drawbacks of different medications for managing pain and anxiety in terminally ill patients. Fentanyl patches and Ativan gel are two commonly used medications, but their effectiveness can vary depending on a patient’s build and weight, particularly for very thin or cachexic individuals.

One of the most important roles is detecting and managing infections in terminally ill geriatric patients with dementia. These patients are often at higher risk for infections due to their weakened immune systems, underlying health conditions, and limited mobility. Detecting infections in these patients can be challenging due to their limited communication abilities and other cognitive and physical impairments. However, early detection and management of infections can significantly improve the patient’s quality of life and potentially prolong their life.