Category: Best Practice
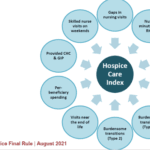
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.
I know how important it is to provide comfort and support during this challenging journey. One aspect of hospice care that often raises concerns is deprescribing medications. In this article, we'll explore what deprescribing is and why it can benefit patients nearing the end of life.
As a hospice nurse, I understand the importance of documenting observational signs of discomfort in terminally ill patients. This guide covers recognizing physical and behavioral cues indicating discomfort, even if patients don't express it. It also highlights the benefits of journaling for families and nurses, with tips for effective documentation to enhance patient comfort and care.

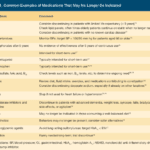
Proper documentation is crucial for hospice nurses to ensure Medicare compliance and maintain the patient's eligibility for services. Auditors, who may not have a healthcare background, review these documents to determine if the patient's condition is terminal. To avoid having the patient removed from service due to improper documentation, hospice nurses should be mindful of the words and phrases they use in their nursing narratives and progress notes. This article will guide what to avoid and why it is essential to paint a picture of a terminally ill patient.

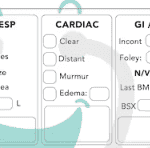
Heart failure is a complex medical condition that can impact the quality of life of patients, especially those in hospice care. As a hospice nurse, assessing the heart failure stage is crucial to providing appropriate care accurately. This article will explore the New York Heart Failure Classification System, its stages, and how to assess patients for their stages. Additionally, we will emphasize the importance of documentation in compliance with Medicare guidelines for terminally ill patients with heart failure.
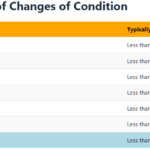
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.

Medication reconciliation plays a pivotal role in hospice care, ensuring terminally ill patients receive safe medication regimens. This process involves maintaining an accurate medication list to prevent adverse drug events. It's essential at various stages, including admission, recertification, and changes in condition. Healthcare professionals should be familiar with tools like the Beers Criteria and STOPP/START criteria to identify potentially inappropriate medications and prescribing omissions in older adults.
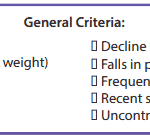
It’s essential to familiarize yourself with the key local coverage determination (LCD) facts for different terminal illnesses to avoid admitting patients who are not eligible for services only to be required to refund the money back to Medicare; otherwise, only have the patient on for one benefit period then discharged for failure to decline. These determinations provide guidelines on the coverage of hospice services for specific conditions. If you are the admitting nurse, please do not just admit because you were told to admit by someone, regardless of the position or standing of the person or party that told you to admit. Use your critical thinking and clinical judgment skills to evaluate the patient for admission. Most doctors will write "evaluate and treat" or something to that effect; never lose sight of the "evaluate" portion of the doctor's order.
Based on the provided PDF files, as noted in the resources section below, let’s explore some essential information for each terminal illness.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.
I understand the challenges that patients and families face when receiving hospice services. One common issue that arises is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can play a crucial role in reducing after-hour calls and providing better support to patients and their families. Here’s how:
Hospice nurses play a vital role in providing quality care and comfort to terminally ill patients and their families. They must make accurate and timely assessments of the patient’s condition, needs, and preferences every visit. This article will outline the key aspects that hospice nurses should assess every visit, in addition to the standard physical assessment.

This article offers guidance for new visiting hospice nurses struggling with work-life balance. It covers strategies like maintaining a recertification journal, pre-charting before visits, assessing end-of-life status, educating families, and preparing for a "good death." By following these tips, nurses can take less work home while delivering focused, compassionate care.

Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider:
Hospice care is focused on symptom management, pain relief, emotional support, and spiritual care. It is a privilege to be a part of a patient’s end-of-life journey, and as a new hospice nurse, you may feel overwhelmed, but you can make a difference in a patient’s life. One of the essential skills you need to learn as a hospice nurse is to recognize when to increase the scheduled visit frequency for a terminally ill patient under hospice care.

Our primary focus for our patients is comfort at the end of life as hospice nurses. We work tirelessly to ensure that our patients receive the best possible care during their end-of-life journey. An aspect of that care that is often overlooked, but incredibly important is timely documentation.
Documenting hospice visits at the bedside is crucial for several reasons. Not only does it help ensure that our patients are receiving the best possible care, but it also helps the hospice team as a whole and reduces issues when the caregiver must be involved in triage services. Here are just a few reasons why documenting hospice visits at the bedside is so important:

There are observation and interviewing skills you can develop which will help you learn:
What could cause the current change in condition
Determining if a patient is having terminal restlessness
Determining if your patient is within two weeks or less of life to live
Knowing where your patient is in the dying process
While this article is primarily meant for new nurses, what I’m sharing is also valuable for family members and loved ones. Anyone with patience and love toward the person being observed and interviewed can hone and develop these skills.
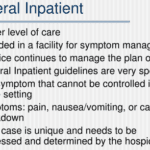
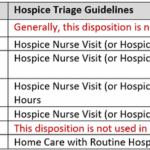
GIP, or General Inpatient Hospice, is an often misunderstood aspect of hospice care. Both hospital staff and families sometimes have misconceptions about GIP. Families may assume it's readily available upon request, while hospital professionals may believe it allows patients to remain in the hospital indefinitely, even when death is weeks away. This article will clarify the basics of GIP for hospice, including eligibility requirements, doctor's orders, care plans, documentation, and education. We'll conclude with two real-life cases to illustrate these points.

If you are a new nurse to hospice, one of the tasks you probably dread is doing an admission especially if you have scheduled visits the same day as the admission.
I would like to share with you some tips that when applied may help lower your stress level, and help you remain on time even in cases where you have three to four visits including recertification to do the same day.