Breast Cancer: Navigating the Journey with Compassion
Published on January 8, 2024
Updated on May 16, 2024
Published on January 8, 2024
Updated on May 16, 2024
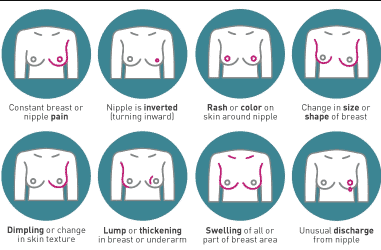
Table of Contents
Breast cancer is a tough road, affecting patients and their families profoundly. As a hospice nurse case manager specializing in compassionate end-of-life care, I comprehend the significance of offering clear, empathetic guidance to families in this challenging situation. This article delves into the journey through breast cancer, the changes your loved one might undergo, and how to deliver optimal care from diagnosis to life’s end.
Breast cancer is a disease that affects the cells in the breasts. Sometimes, these cells grow too fast and form lumps or tumors. These tumors can differ in size, shape, and how much they spread to other body parts. Doctors use stages to describe how serious the breast cancer is and what kind of treatment is needed. Knowing the stages can help you and your family understand what your loved one is going through and how you can help them.
In the early stages, breast cancer is small and has not spread to other parts of the body. The main goal of treatment is to remove the tumor and stop it from growing back. Treatment may include surgery, radiation, or targeted therapies. Surgery is when the doctor cuts out the tumor and some of the healthy tissue around it. Radiation is when the doctor uses high-energy rays to kill the cancer cells. Targeted therapies are medicines that work on specific types of breast cancer cells.
Possible Changes: Your loved one may need time to recover and heal after the treatment. They may feel tired, sore, or weak. They may also lose some or all of their hair due to radiation. They may have different emotions, such as sadness, anger, fear, or hope. It is normal to have these feelings, and it is important to talk about them. You can help your loved one by being there for them, listening to them, and encouraging them. You can also help them with daily activities, such as cooking, cleaning, or driving.
In the advanced stages, breast cancer is large and has spread to other parts of the body, such as the bones, lungs, liver, or brain. The main goal of the treatment is to slow down the growth of the cancer and make the symptoms less severe. The treatment may include chemotherapy, immunotherapy, or hormone therapy. Chemotherapy is when the doctor uses strong medicines to kill the cancer cells. Immunotherapy is when the doctor uses medicines to boost the immune system, the body’s natural defense against diseases. Hormone therapy is when the doctor uses medicines to block or lower the hormones that make the cancer grow.
Possible Changes: The treatment for advanced breast cancer can have many side effects, such as nausea, vomiting, diarrhea, mouth sores, infections, or bleeding. These side effects can make your loved one feel extremely sick and uncomfortable. They may also lose more of their hair and weight. They may have more emotional challenges, such as depression, anxiety, guilt, or loneliness. They may worry about their future and their family. It is hard to cope with these changes, and it is okay to feel overwhelmed. You can help your loved one by being supportive, understanding, and respectful. You can also help them find comfort, joy, and meaning.
In the end-of-life stage, the breast cancer has spread too much, and the treatment is no longer working. The main goal of the care is to make your loved one feel as comfortable and peaceful as possible. The care may include palliative care, pain management, or emotional support. Palliative care is when the doctor and nurse work together to provide your loved one with the best quality of life. They can help with physical, emotional, social, and spiritual needs. Pain management is when the doctor and the nurse use medications or other methods to reduce or relieve the pain. Emotional support is when the doctor, the nurse, the counselor, or the chaplain helps your loved one and your family cope with the emotions and the grief.
Possible Changes: In the end-of-life stage, your loved one may have more physical and emotional symptoms, such as increased fatigue, pain, reduced appetite, difficulty breathing, confusion, or restlessness. They may also have more spiritual needs, such as finding peace, forgiveness, or closure. They may want to say goodbye to their loved ones and express their wishes. It is hard to say goodbye, and it is normal to feel sad, angry, or scared. You can help your loved one by being present, attentive, and loving. You can also help them fulfill their wishes, such as playing their favorite music, reading their favorite book, or visiting their favorite place. You can also help them say goodbye in their way, such as writing a letter, making a video, or giving a gift.
When someone you love has breast cancer, you want to do your best to help them. You can help them by noticing the changes in their body and mind and giving them the support they need.
Physical Changes: Breast cancer and its treatment can make your loved one feel different in their body. They may feel more tired, hungry, or in pain. They may also have trouble moving around or doing things they used to do. You can help them by watching how they feel and what they need. You can help them with their daily tasks, such as dressing, showering, or going to the bathroom. You can also make them healthy and tasty food and ensure they have a comfortable resting place.
Emotional Changes: Breast cancer and its treatment can also make your loved one feel different in their mind. They may have many emotions, such as sadness, anger, fear, or hope. Sometimes, they may feel happy, and sometimes they may feel low. You can help them by being aware of their mood and how they cope. You can start honest conversations, listen to them compassionately, and encourage them to share their feelings. You can also help them find ways to relax, such as reading, listening to music, or meditating.
Communication and Support: Breast cancer and its treatment can be hard to understand and deal with. You and your loved one may have many questions and concerns. You can help them by keeping the lines of communication open. You can offer your company and let them know you are there for them. You can also go to the medical appointments with them, write down notes, and ask the doctor or nurse questions. You can help them understand their treatment plan and what to expect.
Palliative and Hospice Care: As the breast cancer gets worse, the treatment may not work anymore. The goal of the care is to make your loved one feel as comfortable and peaceful as possible. You can help them by focusing on their comfort and quality of life. You can work with the healthcare experts to manage their symptoms, make sure they have less pain, and give them emotional support. You can also help them find meaning and purpose in their life and prepare for the end of their life.
There may come a time when the cancer treatment is no longer working, and your loved one is nearing the end of life. This can be an exceedingly difficult and emotional time for both of you. You may feel sad, angry, scared, or numb. You may also have many questions and concerns about what will happen and how to help your loved one. This section will give tips on providing end-of-life care and ensuring comfort and peace for your loved one.
Hospice Care: Hospice care focuses on making your loved one as comfortable as possible in the last months, weeks, or days of life. Hospice care does not try to cure cancer or prolong life but rather to relieve pain and other symptoms, such as nausea, shortness of breath, or anxiety. Hospice care also provides emotional and spiritual support for your loved one and family. Hospice care can be given at home, in a hospital, or at a hospice facility, depending on your loved one’s needs and preferences. You can help your loved one by:
Emotional Well-being: The end of life can be a time of mixed emotions for your loved one and family. Your loved one may feel grateful, peaceful, or relieved but also sad, angry, or scared. They may also have regrets, unfinished business, or unfulfilled dreams. You can help your loved one by:
The journey through breast cancer is a challenging and life-altering experience for patients and their families. Understanding the stages of breast cancer and the changes your loved one might undergo is crucial in delivering optimal care from diagnosis to end of life. The early stages involve treatments such as surgery, radiation, and targeted therapies, while the advanced stages may require chemotherapy, immunotherapy, or hormone therapy. In the end-of-life stage, the focus shifts to providing comfort and peace through palliative care, pain management, and emotional support. Patients’ experiences are deeply affected by the different medical stages, each unleashing specific physical, emotional, cognitive, and social processes. Recognizing the physical and emotional changes, providing tender care, and offering communication and support are essential in helping patients navigate this journey compassionately. As a hospice nurse case manager specializing in compassionate end-of-life care, I emphasize the importance of empathy, understanding, and respectful support throughout the breast cancer journey, from diagnosis to end-of-life, to empower patients, caregivers, and families.
Caring for a Loved One with Terminal Cancer: A Guide for Families
Understanding Cancer Metastasis: A Guide for Patients and Families
American Cancer Society – Breast Cancer Guide
National Cancer Institute – Understanding Breast Cancer
Signs & Symptoms of Breast Cancer
Basic Information About Breast Cancer
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death