Assessing Patients on the FAST Scale: A Guide for Nurses
Published on May 20, 2024
Updated on July 29, 2025
Published on May 20, 2024
Updated on July 29, 2025
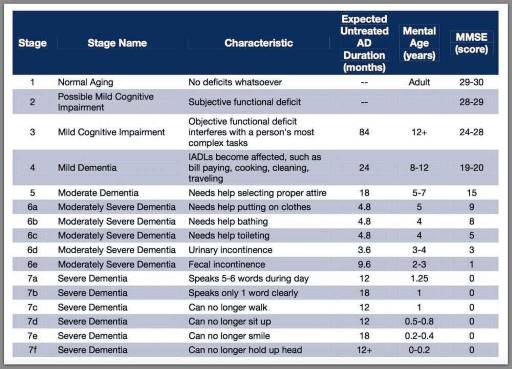
Table of Contents
As a nurse who has cared for many terminally ill individuals with Alzheimer’s disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer’s disease, helping to guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.
If you are more of a visual-audio person, please see the first link in the resource section below for a YouTube video that explains how to read the scale.
The FAST scale, or the Functional Assessment Staging Tool, is a reliable and widely used measure to assess the functional status of patients with dementia. It was developed by Dr. Barry Reisberg, a leading expert in Alzheimer’s disease, in the 1980s. The FAST scale helps nurses, doctors, and caregivers to understand, communicate, and monitor the progression of dementia and its impact on the patient’s ability to perform daily tasks.
The FAST scale consists of seven stages, with the first two representing the functional ability of an adult without dementia and the last one representing the disease’s final and most severe stage. Each stage describes the patient’s level of functioning and activities of daily living (ADLs), such as dressing, bathing, eating, speaking, and walking. The FAST scale also indicates the patient’s eligibility for hospice care, usually recommended when the patient reaches stage 7.
It is essential to note that the FAST scale emphasizes functional abilities and activities of daily living (ADLs) rather than cognitive decline, which can vary from patient to patient. Therefore, the FAST scale should be used with other tools and tests that measure the patient’s cognitive and behavioral changes, such as the Mini-Mental State Examination (MMSE) or the Neuropsychiatric Inventory (NPI). The FAST scale should also be used with caution and sensitivity, as it may not capture the patient’s individuality, preferences, and quality of life.
Using the FAST scale, the nurse should interview the patient and their caregiver and observe their behavior and performance. Based on the guidelines and examples provided by the FAST scale, the nurse should identify the highest consecutive level of disability the patient exhibits. The nurse should document the patient’s score on the FAST scale and compare it with previous scores to track the changes over time.
The FAST scale is a quick and straightforward tool used during each office or home visit. However, the nurse should be aware of its limitations and challenges, such as the subjective nature of some items, the variability of the patient’s condition, and the influence of environmental factors. The nurse should also be respectful and empathic when communicating the results of the FAST scale to the patient and their caregiver and providing them with appropriate information and support.
Here are some examples of patients at various stages of the FAST scale, along with some nursing interventions and recommendations:
FAST Stage 5 represents moderately severe functional losses. Here’s an example of how to assess a patient at this stage:
FAST Stage 6D indicates severely impaired functional abilities. Here’s an example of how to assess a patient at this stage:
FAST Stage 7C represents total dependence, indicating the most advanced stage of Alzheimer’s disease. Here’s an example of how to assess a patient at this stage:
Remember, these examples provide a general idea of the functional abilities at each stage, but each patient is unique, and their progression may vary. Assessing individuals holistically and considering their specific needs and abilities is crucial.
The Functional Assessment Staging Tool (FAST) is a valuable instrument for assessing the functional decline of individuals with dementia, particularly Alzheimer’s disease. It provides an efficient and comprehensive evaluation of functional ability and the potential for functional decline over time, enabling healthcare professionals, caregivers, and family members to monitor the patient’s capabilities. The FAST scale consists of seven stages, with the first two representing the functional ability of an adult without dementia and the last one representing the disease’s final and most severe stage. It focuses on functional abilities and activities of daily living (ADLs), making it a valuable tool for care planning and determining eligibility for hospice care.
When using the FAST scale, nurses should interview the patient and their caregiver, observe the patient’s behavior and performance, and identify the highest consecutive level of disability exhibited by the patient. Using the FAST scale in conjunction with other tools and tests that measure cognitive and behavioral changes is essential, as it communicates the results respectfully and empathetically to the patient and their caregiver.
The FAST scale should be completed on the admission of any patient with Dementia/Alzheimer’s Disease as the primary or secondary diagnosis for each re-certification period, any time a patient’s cognitive function would be considered a prognostic indicator for survival, or any time there are significant status changes.
In conclusion, the FAST scale is a valuable tool for assessing the functional decline of individuals with dementia. Its proper use can significantly contribute to developing personalized care plans and providing appropriate support for patients and their families.
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy (YouTube Video by author of this article – includes several examples)
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
The Mini-Mental State Examination (MMSE)
Neuropsychiatric Inventory (NPI)
Validation Therapy a helpful tool for all caregivers
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.