Introduction
Brief Overview of Dementia-Induced Psychosis
Dementia-induced psychosis is a complex and distressing condition that affects individuals with advanced dementia. It is characterized by a range of psychiatric symptoms, including hallucinations, delusions, severe agitation, and paranoia. These symptoms can significantly impact the quality of life for patients and create immense challenges for those providing care. Understanding the nuances of dementia-induced psychosis is crucial for hospice nurses, caregivers, and family members, as it enables them to offer more effective and compassionate care to those in their final stages of life.
Importance of Understanding and Managing This Condition in Hospice Care
Managing dementia-induced psychosis is essential in the context of hospice care, where the primary goal is to ensure comfort and dignity during the end-of-life journey. Misunderstanding or mismanaging this condition can increase patient distress, exacerbate symptoms, and create a more challenging environment for caregivers and family members. By gaining a thorough understanding of dementia-induced psychosis, hospice care providers can implement tailored strategies to alleviate symptoms, reduce patient suffering, and provide a more peaceful and supportive environment. This knowledge also equips caregivers and family members with the tools to manage the emotional and practical demands of caring for someone with this condition.
What is Dementia-Induced Psychosis?
Definition and Explanation
Dementia-induced psychosis is a severe condition that affects individuals with advanced stages of dementia, such as Alzheimer’s disease, Lewy body dementia, or vascular dementia. It involves a severe disturbance in a person’s ability to perceive and interpret reality, leading to symptoms such as hallucinations and delusions.
Hallucinations are sensory experiences that seem natural to the person but are not present. These can be visual (seeing things that aren’t there), auditory (hearing sounds or voices that aren’t real), or even tactile (feeling sensations on the skin).
Delusions are firmly held false beliefs that are not based on reality. For instance, a person might believe that a family member is an impostor or is in danger when they are not. These delusions can be persistent and distressing, making it difficult for the person to function normally.
Dementia-induced psychosis can significantly impact the quality of life for both the patient and their caregivers. The unpredictable and often disturbing nature of the symptoms can create a challenging and stressful environment for everyone involved.
Common Causes and Contributing Factors
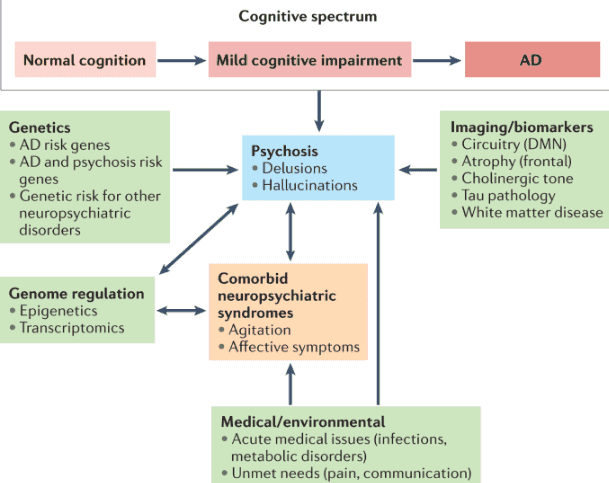
Dementia-induced psychosis is primarily caused by the progressive damage to the brain associated with dementia. As the disease advances, it affects various brain regions responsible for thinking, memory, and perception. Here are some of the critical factors that contribute to the development of psychosis in dementia patients:
- Brain Changes:
- Neurodegeneration: The gradual loss of neurons and the breakdown of neural networks in the brain are hallmarks of neurodegeneration, a condition that often leads to dementia. This damage disrupts normal brain function, leading to cognitive and perceptual disturbances.
- Chemical Imbalances: Neurotransmitters, the chemicals that transmit signals in the brain, become imbalanced in dementia. This can affect mood, perception, and behavior, contributing to psychotic symptoms.
- Disease Progression:
- Advanced Dementia Stages: Psychosis is more common in the later stages of dementia, as the brain has sustained more significant damage over time. As cognitive abilities decline, the brain struggles to process and interpret sensory information correctly.
- Medical and Environmental Factors:
- Infections: Urinary tract infections, pneumonia, or other infections can exacerbate dementia symptoms and trigger psychosis.
- Medication Side Effects: Some medications, particularly those affecting the central nervous system, can induce or worsen psychotic symptoms. These might include certain pain medications, sedatives, or drugs for other medical conditions.
- Sensory Deprivation or Overstimulation: Environments that are too quiet and lack stimulation or those that are chaotic and noisy can confuse dementia patients, potentially leading to psychotic episodes.
- Changes in Routine: Disruptions to familiar routines and environments can increase stress and confusion, contributing to the development of psychotic symptoms.
- Genetic and Biological Factors:
- Family History: A family history of dementia or psychiatric disorders may increase the likelihood of developing psychosis in dementia.
- Underlying Health Conditions: Conditions such as Parkinson’s disease, Huntington’s disease, or other neurological disorders can increase the risk of psychosis.
Understanding these causes and contributing factors is crucial for hospice nurses, caregivers, and family members. It helps in identifying potential triggers and implementing strategies to minimize the impact of psychotic symptoms on the patient’s well-being. Managing the environment, carefully monitoring medications, and maintaining a stable routine can all play vital roles in reducing the frequency and severity of psychotic episodes.
Through compassionate care and a deep understanding of dementia-induced psychosis, caregivers can better support their loved ones and improve their quality of life during the challenging final stages of dementia.
Signs and Symptoms of Dementia-Induced Psychosis
Detailed Description of Typical Symptoms
Dementia-induced psychosis manifests through a range of psychiatric symptoms that significantly impact the patient’s perception, behavior, and emotions. Understanding these symptoms is essential for providing compassionate and effective care.
Hallucinations and Delusions
Hallucinations
Hallucinations are false sensory experiences that can involve any of the senses. They are vivid and convincing to the person experiencing them, even though they have no basis in reality.
- Visual Hallucinations: Seeing people, animals, or objects that are not present. A person might describe seeing children playing in the room or someone standing by their bed.
- Auditory Hallucinations: Hearing sounds or voices that are not there. Patients might hear conversations, music, or someone calling their name.
- Tactile Hallucinations: Feeling sensations on the skin that aren’t real, such as bugs crawling or a hand touching them.
Delusions
Delusions are solid and false beliefs that the person holds with conviction despite evidence to the contrary.
- Paranoid Delusions: Beliefs that others are plotting against them, stealing from them, or causing them harm. For example, a patient might believe that a caregiver is trying to poison them.
- Misidentification Delusions: Believing that a familiar person is an impostor or that an identical copy has replaced them at home. A person might insist that their spouse is a stranger pretending to be their spouse.
These hallucinations and delusions can cause significant distress and confusion, making it challenging for patients to distinguish between reality and their altered perceptions.
Agitation and Aggression
Agitation
Agitation is a state of restlessness and irritability triggered by confusion, frustration, or discomfort. It often manifests in repetitive movements, pacing, or an inability to sit still.
- Physical Restlessness: Constant movement, pacing, or fidgeting.
- Verbal Outbursts: Shouting, swearing, or repetitive questioning.
Aggression
Aggression can emerge as a response to perceived threats or frustrations and can be verbal or physical.
- Verbal Aggression: Yelling, cursing, or making threatening statements.
- Physical Aggression: Hitting, pushing, scratching, or other forms of physical violence.
Environmental stressors or unmet needs, such as hunger, pain, or the need for toileting, often exacerbate both agitation and aggression.
Sleep Disturbances
Sleep disturbances are common in dementia patients and can be particularly pronounced in those experiencing psychosis.
- Insomnia: Difficulty falling or staying asleep, leading to prolonged wakefulness at night.
- Night-time Wandering: Getting up and moving around the house at night can be dangerous if the environment is unsafe.
- Daytime Sleepiness: Increased drowsiness and napping during the day, often resulting from poor sleep at night.
- Sleep-Wake Cycle Reversal: Confusion between day and night causes a person to be awake, active at night, and sleepy during the day.
These sleep disruptions can further contribute to the patient’s confusion and overall cognitive and physical health decline.
Emotional Distress
Emotional distress in dementia-induced psychosis can manifest as anxiety, depression, or severe mood swings.
- Anxiety: Persistent worry or fear, which hallucinations, delusions, or changes in routine can trigger. Patients might display signs such as trembling, sweating, or a rapid heartbeat.
- Depression: Feelings of sadness, hopelessness, or loss of interest in activities they once enjoyed. They may become withdrawn and less responsive to social interactions.
- Mood Swings: Rapid and unpredictable changes in mood, such as going from calm to angry or happy to sad within a short period.
Emotional distress not only affects the patient’s mental health but also impacts their physical well-being, potentially leading to a decline in overall health.
Variations in Symptoms Among Patients
The symptoms of dementia-induced psychosis can vary widely among patients, depending on factors such as the type and stage of dementia, individual health conditions, and environmental influences.
Type of Dementia
- Alzheimer’s Disease: Patients may experience more frequent hallucinations and delusions in the later stages.
- Lewy Body Dementia: Hallucinations, particularly visual ones, are common even in the early stages.
- Vascular Dementia: Psychotic symptoms may be less predictable and more related to the specific areas of the brain affected by strokes.
Stage of Dementia
- Early Stages: Psychotic symptoms might be mild and sporadic, often mistaken for confusion or simple forgetfulness.
- Middle Stages: Symptoms become more pronounced and frequent, with hallucinations and delusions becoming a regular part of the patient’s experience.
- Late Stages: Psychotic symptoms may peak, causing significant distress and requiring intensive management.
Individual Health Conditions
- Physical Health: Coexisting health issues like infections, pain, or medication side effects can exacerbate psychotic symptoms.
- Mental Health History: A history of psychiatric disorders may influence the type and severity of psychotic symptoms.
Environmental Influences
- Stressful Environments: Noise, chaos, or frequent changes can increase confusion and trigger psychotic episodes.
- Calm and Familiar Settings: Establishing familiar routines, incorporating comforting objects, and maintaining a stable environment can help reduce the frequency and severity of symptoms.
By recognizing the signs and symptoms of dementia-induced psychosis and understanding how they can vary among patients, hospice nurses, caregivers, and family members can better support their loved ones. Through compassionate care and tailored interventions, it is possible to improve the quality of life for those affected by this challenging condition.
Differentiating Dementia-Induced Psychosis vs Unmanaged Pain and Anxiety
Recognizing and differentiating between dementia-induced psychosis, unmanaged pain, and anxiety is critical for providing appropriate and effective care. These conditions can present overlapping symptoms, making an accurate diagnosis essential to ensure patients receive the proper treatment and support.
Common Symptoms of Unmanaged Pain and Anxiety
Unmanaged Pain
Unmanaged pain in dementia patients often manifests in ways that might not be immediately recognized as pain, especially if the patient cannot communicate their discomfort. Here are some common signs:
- Physical Indicators: Grimacing, moaning, or crying, especially during movement or touch.
- Behavioral Changes: Increased restlessness, agitation, or refusal to move or participate in activities.
- Verbal Complaints: While some patients may verbalize their pain, many may struggle to articulate it clearly.
- Protective Movements: Guarding a part of the body, avoiding specific movements, or withdrawing from physical contact.
Anxiety
Anxiety in dementia patients can be triggered by confusion, changes in routine, or unfamiliar environments. Common symptoms include:
- Restlessness: Pacing, fidgeting, or an inability to sit still.
- Increased Heart Rate: Palpitations or rapid breathing, often accompanied by sweating.
- Verbal Expressions: Repetitive questioning, expressing fears or worries, and increased irritability.
- Avoidance Behaviors: Reluctance to engage in activities or interact with others, accompanied by a persistent need for constant reassurance from caregivers.
Key Differences Between These Conditions and Dementia-Induced Psychosis
While there are overlapping symptoms among unmanaged pain, anxiety, and dementia-induced psychosis, several key differences can help distinguish between these conditions.
Hallucinations and Delusions
- Dementia-Induced Psychosis: Hallucinations (seeing, hearing, or feeling things that are not present) and delusions (firmly held false beliefs) are hallmark symptoms. These experiences are vivid and real to the patient, often involving intricate and detailed perceptions that persist over time.
- Unmanaged Pain and Anxiety: These conditions typically do not cause hallucinations or delusions. Instead, they lead to more straightforward expressions of discomfort or fear.
Nature of Agitation and Aggression
- Dementia-Induced Psychosis: Agitation and aggression often stem from the patient’s altered perceptions and misinterpretations of reality. For example, a patient might become aggressive because they believe a caregiver is trying to harm them.
- Unmanaged Pain: Agitation due to pain usually responds to physical discomfort. It might become apparent during specific activities or movements that exacerbate the pain.
- Anxiety: Agitation related to anxiety is often linked to environmental stressors, changes in routine, or overwhelming stimuli. The agitation here is more about a general sense of fear or unease rather than specific delusions or hallucinations.
Emotional Responses
- Dementia-Induced Psychosis: Emotional distress in psychosis is directly linked to hallucinations and delusions. The patient’s mood can shift dramatically based on their altered perceptions.
- Unmanaged Pain: Emotional responses to pain include frustration, irritability, or withdrawal, primarily due to the persistent discomfort.
- Anxiety: Anxiety-induced emotional distress involves fear, worry, and sometimes panic attacks. It is more about an internal sense of dread rather than external perceptions.
Sleep Disturbances
- Dementia-Induced Psychosis: Sleep disturbances can be caused by the patient’s altered perception of reality, leading to nighttime agitation, wandering, or fear of imaginary threats.
- Unmanaged Pain: Pain can disrupt sleep due to physical discomfort, making it hard for the patient to fall or stay asleep.
- Anxiety: Anxiety can cause insomnia or restless sleep due to racing thoughts, worries, or a general inability to relax.
Importance of Accurate Diagnosis
Accurately diagnosing whether a patient is experiencing dementia-induced psychosis, unmanaged pain, or anxiety is crucial for several reasons:
Effective Treatment
- Targeted Interventions: Proper diagnosis enables the delivery of specific treatments tailored to the individual’s condition. For example, antipsychotic medications may be appropriate for dementia-induced psychosis. At the same time, pain management strategies are essential for unmanaged pain, and anxiety might be best treated with calming techniques or medications.
- Avoiding Harm: Misdiagnosis can lead to inappropriate treatments that might exacerbate symptoms. For instance, using antipsychotics to treat pain-related agitation could lead to unnecessary side effects without addressing the root cause.
Improved Quality of Life
- Symptom Relief: Accurate diagnosis and treatment improve the patient’s comfort and overall quality of life. Properly managing pain and anxiety reduces unnecessary suffering and enhances the patient’s ability to engage in daily activities.
- Reduced Stress for Caregivers: When caregivers understand the true nature of the patient’s symptoms, they can provide more effective and compassionate care. This reduces their stress and helps them feel more confident in their caregiving role.
Comprehensive Care Plans
- Holistic Approach: Accurate diagnosis leads to a comprehensive care plan that addresses all aspects of the patient’s health and well-being, including physical, emotional, and psychological support.
- Coordination of Care: It facilitates better communication and coordination among the healthcare team, ensuring that all providers are aligned regarding the patient’s condition and treatment plan.
By differentiating between dementia-induced psychosis, unmanaged pain, and anxiety, hospice nurses, caregivers, and family members can provide more precise and empathetic care. This approach alleviates the patient’s suffering and enhances the overall caregiving experience, creating a more supportive and understanding environment for everyone involved.
Symptom Management of Dementia-Induced Psychosis
Managing dementia-induced psychosis requires a comprehensive approach that includes both non-pharmacological and pharmacological interventions. Each patient’s needs are unique, so individualized care plans are essential.
Non-Pharmacological Interventions
Environmental Modifications
Creating a safe, calm, and familiar environment can significantly reduce the triggers for psychotic symptoms. Here are some strategies:
- Reduce Noise and Clutter: A quiet, orderly space helps minimize confusion and agitation. Soft background music can be calming, while excessive noise can be distressing.
- Consistent Routine: Establishing a regular daily routine provides stability and predictability. Regular mealtimes, bathing, and bedtime routines can help reduce anxiety.
- Comfort Items: To provide comfort and reassurance, surround the patient with familiar objects, such as family photos, favorite blankets, or familiar scents.
- Lighting: Ensure adequate lighting, especially at night, to reduce shadows that can be misinterpreted as threatening. Soft, warm lighting is more soothing than harsh, bright lights.
Behavioral Therapies
Behavioral therapies focus on engaging the patient in meaningful activities and interactions that can help manage symptoms.
- Validation Therapy: This approach involves acknowledging and empathizing with the patient’s feelings without trying to correct their perceptions. For example, if a patient believes they see someone who isn’t there, instead of arguing, acknowledge their feelings and gently redirect the conversation.
- Reminiscence Therapy: Encouraging patients to talk about their experiences and memories can provide comfort and reduce agitation. Using photos, music, or familiar objects can help stimulate these memories.
- Sensory Stimulation: Activities that engage the senses, such as listening to music, holding a soft object, or smelling familiar scents, can help calm the patient and reduce anxiety.
- Physical Activity: Gentle exercises, such as walking, stretching, or simple yoga, can improve mood and reduce restlessness.
Pharmacological Treatments
In some cases, medications may be necessary to manage severe symptoms of dementia-induced psychosis. However, these should be used with caution and under close medical supervision.
Antipsychotic Medications
Antipsychotics can help manage hallucinations, delusions, and severe agitation. Common antipsychotics used include:
- Risperidone (Risperdal)
- Quetiapine (Seroquel)
- Olanzapine (Zyprexa)
Considerations:
- Risks and Benefits: Antipsychotics can have serious side effects, such as increased risk of stroke, sedation, and worsening of cognitive function. The potential benefits must be weighed against these risks.
- Lowest Effective Dose: Always start with the lowest effective dose and closely monitor for side effects. Regularly review the necessity of the medication.
Sedatives and Other Medications
In addition to antipsychotics, other medications might be used to manage symptoms:
- Benzodiazepines: Drugs like lorazepam (Ativan) can help with severe anxiety and agitation, but should be used sparingly due to the risk of dependency and sedation.
- Mood Stabilizers: Medications like valproate (Depakote) may be used to manage mood swings and aggression.
- Sleep Aids: Medications to help with sleep disturbances should be used cautiously to avoid excessive sedation and falls.
Strategies for Families and Caregivers
Caring for a loved one with dementia-induced psychosis can be challenging and stressful. Here are some strategies to help manage symptoms and provide support.
Communication Techniques
Effective communication can help reduce frustration and enhance interactions with patients.
- Simple, Clear Language: Use short sentences and speak in a clear, slow tone. Avoid complex instructions or questions.
- Eye Contact and Body Language: Maintain eye contact and use positive body language to convey empathy and understanding.
- Calm Tone: Speak in a relaxed, reassuring voice. Avoid arguing or correcting the patient’s perceptions, as this can increase agitation.
- Distraction and Redirection: Gently distract or redirect the patient if they become fixated on a distressing hallucination or delusion.
Support Systems
Building a support network is crucial for both caregivers and patients.
- Professional Support: Engage with healthcare professionals, including doctors, nurses, social workers, and therapists, who can provide guidance and support.
- Support Groups: Join support groups for caregivers to share experiences, gain insights, and receive emotional support.
- Respite Care: Utilize respite care services to take breaks and recharge. Caring for yourself is essential to maintain your ability to care for your loved one.
Role of Hospice Nurses in Managing Symptoms
Hospice nurses play a critical role in the care and management of patients with dementia-induced psychosis. Their expertise and compassion are vital in patient comfort and dignity.
Assessment and Monitoring
Regular assessment and monitoring of symptoms are crucial for providing effective care.
- Symptom Tracking: Keep detailed records of the patient’s symptoms, including the frequency, duration, and triggers of hallucinations, delusions, and agitation.
- Pain Assessment: Regularly assess for signs of pain, as unmanaged pain can exacerbate psychotic symptoms. Utilize pain assessment tools specifically designed for patients with dementia.
- Medication Review: Continuously review medications for effectiveness and side effects and adjust treatment plans as necessary.
Coordination with Healthcare Team
Effective management of dementia-induced psychosis requires a coordinated approach involving the entire healthcare team.
- Interdisciplinary Meetings: Participate in regular multidisciplinary team meetings to discuss the patient’s condition and care plan. This ensures that all team members are informed about changes and can contribute to providing comprehensive care.
- Family Communication: Keep open lines of communication with the patient’s family. Provide updates on the patient’s condition, explain treatment options, and offer support and guidance.
- Education and Training: Educate caregivers and family members about dementia-induced psychosis, symptom management techniques, and the importance of self-care.
Managing dementia-induced psychosis involves a combination of non-pharmacological and pharmacological interventions tailored to each patient’s needs. By creating a supportive environment, utilizing behavioral therapies, and closely monitoring medications, hospice nurses, caregivers, and family members can significantly enhance the quality of life for individuals affected by this condition. Effective communication, support systems, and coordinated care are crucial in navigating the challenges of dementia-induced psychosis with empathy and compassion.
Conclusion
Recap of Key Points
Dementia-induced psychosis presents significant challenges for patients, hospice nurses, caregivers, and family members. Understanding and managing this condition require a thorough and compassionate approach. Here’s a summary of the key points discussed:
- Understanding Dementia-Induced Psychosis:
- Defined as a state where dementia patients experience hallucinations, delusions, agitation, aggression, sleep disturbances, and emotional distress.
- Recognizing the symptoms is crucial for providing appropriate care.
- Differentiating Symptoms:
- It’s essential to distinguish between dementia-induced psychosis, unmanaged pain, and anxiety to ensure the correct treatment.
- Key differences include the nature of hallucinations and delusions in psychosis versus the physical and emotional expressions of pain and anxiety.
- Non-Pharmacological Interventions:
- Environmental modifications such as reducing noise, maintaining a consistent routine, and using comfort items can help manage symptoms.
- Behavioral therapies, including validation therapy, reminiscence therapy, sensory stimulation, and physical activity, effectively relieve and improve quality of life.
- Pharmacological Treatments:
- Medications, including antipsychotics and sedatives, can be necessary for severe symptoms but should be used cautiously and monitored closely for side effects.
- Using the lowest effective dose and regularly reassessing medication needs is vital.
- Strategies for Families and Caregivers:
- Effective communication techniques involve using simple language, maintaining eye contact, and speaking calmly and clearly.
- Support systems, including professional support, support groups, and respite care, are essential for caregiver well-being and effective patient care delivery.
- Role of Hospice Nurses:
- Hospice nurses play a pivotal role in assessing and monitoring symptoms, coordinating with the healthcare team, and educating caregivers and family members.
- Regular interdisciplinary meetings and open communication ensure comprehensive and compassionate care.
Final Thoughts on the Importance of Compassionate Care
Compassionate care is the cornerstone of managing dementia-induced psychosis, providing a foundation for all interventions and treatments. Here are some final thoughts on its importance:
- Empathy and Understanding: Recognizing that patients with dementia-induced psychosis are experiencing real distress, even if their perceptions are not based on reality, is crucial. Approaching them with empathy can alleviate their anxiety and fear.
- Patient-Centered Approach: Tailoring care plans to each patient’s unique needs, considering their history, preferences, and current symptoms, ensures that interventions are effective and respectful.
- Holistic Care: Addressing a patient’s physical, emotional, and psychological needs leads to better outcomes and enhances their overall quality of life.
- Support for Caregivers: Providing caregivers with resources, education, and emotional support helps them manage their responsibilities and maintain their own well-being, enabling them to offer better care to their loved ones.
- Communication and Coordination: Effective communication among caregivers, healthcare professionals, and family members ensures a unified approach to care, minimizing confusion and optimizing treatment plans.
By embracing these principles, hospice nurses, caregivers, and family members can create a nurturing environment that respects the dignity and individuality of patients with dementia-induced psychosis. Compassionate care alleviates suffering and fosters a sense of connection and comfort, making the end-of-life journey as peaceful and meaningful as possible.
Resources
Dementia-Related Psychosis
Understanding the Burden of Dementia-Related Psychosis
Behavior Disorders of Dementia: Recognition and Treatment
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
PAINAD Scale Offers Alternative to Assessing Pain in the Dementia Patient – JEMS: EMS, Emergency Medical Services – Training, Paramedic, EMT News
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Chronic Pain & Symptom Tracker: A 90-Day Guided Journal: Detailed Daily Pain Assessment Diary, Mood Tracker & Medication Log for Chronic Illness Management
Pain And Symptom Tracker: Daily Pain Tracking Journal Detailed Pain Assessment Diary, Medication, Supplements Food & Activities Log for Chronic Illness Management
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
FLACC Pain Scale
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
My Loved One with Dementia
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy. (Video)
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Disease and Other Dementias
How Do I Know You? Dementia at the End of Life
The Dementia Caregiver: A Guide to Caring for Someone with Alzheimer’s Disease and Other Neurocognitive Disorders (Guides to Caregiving)
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
The Caregiver’s Guide to Dementia: Practical Advice for Caring for Yourself and Your Loved One (Caregiver’s Guides)
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
How to read and apply the FAST Scale to stage any type of dementia. Dementia Staging Made Easy
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer’s Disease and Other Dementias
Creating Moments of Joy Along the Alzheimer’s Journey: A Guide for Families and Caregivers, Fifth Edition, Revised and Expanded
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Caregiver Support Book Series
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
The Validation Breakthrough: Simple Techniques for Communicating with People with ‘Alzheimer’s-Type Dementia’
Dementia Home Care: How to Prepare Before, During, and After
DEMENTIA DENIED: One Woman’s True Story of Surviving a Terminal Diagnosis & Reclaiming Her Life
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Fading Reflection: Understanding the complexities of Dementia
Dementia Caregiving: A Self Help Book for Dementia Caregivers Offering Practical Coping Strategies and Support to Overcome Burnout, Increase Awareness, and Build Mental & Emotional Resilience
Navigating the Dementia Journey: A Compassionate Guide to Understanding, Supporting, and Living With Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare